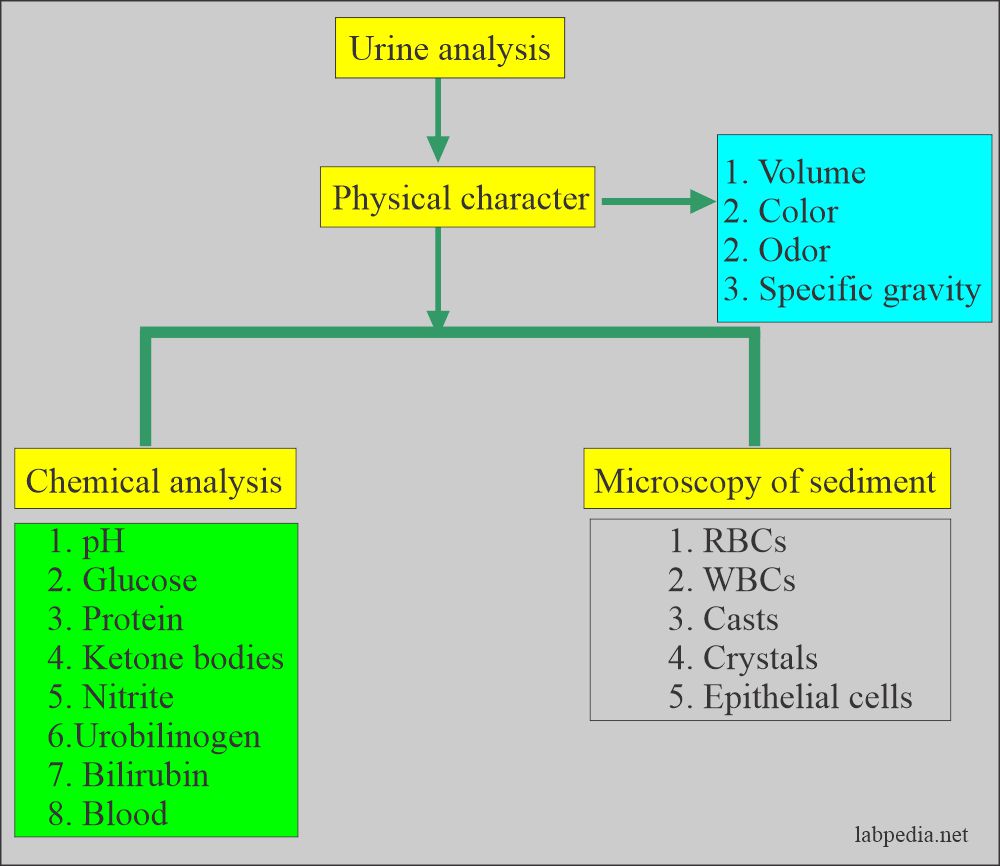
Urine Analysis:- Part 2 – Microscopic Examination and Interpretations
Urine analysis
Urine Microscopic Examination
Sample for urine analysis
- Freshly voided urine is the best sample.
- If delayed, then refrigerate the urine.
- The best volume for the centrifuge is 10 to 12 mL.
Factors that will interfere with the urine analysis:
- Certain foods will color the urine, like:
- Carrots will change their urine color to dark yellow.
- Beets may cause red color urine.
- Rhubarb will change its color to red or brown.
- Asparagus produces a typical urine odor.
- If you keep urine on the table, bacteria will change the urine pH, making it alkaline because of urea-splitting bacteria, and there is the production of ammonia.
- Effect of the food on the urine pH:
- Eating citrus fruits, dairy products, and vegetables makes urine alkaline.
- A high protein diet and some foods (cranberries) make urine acidic.
- A high protein, a fat diet without the intake of carbohydrates also causes ketonuria.
- When radiopaque contrast media is given to the patient will give false-positive urine protein for at least 3 days.
- Females may have contamination from the vaginal secretions and show an increased number of WBCs.
- Traumatic catheterization may cause hematuria and false RBCs in the urine.
- Vaginal secretions contamination may cause false-positive leucocyte esterase.
- False proteinuria is seen when urine is contaminated with vaginal secretions.
- Urine culture gives false-positive results when contaminated with stool, vaginal secretions, and contaminated test tubes or hands and clothes.
Procedure for urine microscopy:
- Centrifuge the Urine; clear supernatant is removed and leaves the uniform volume of sediment, usually 1 mL.
- The recommended time for centrifugation is 5 minutes.
- The standard centrifugation speed recommended is 400 g.
Normal urine analysis sediment
- Normally there is no sediment or very little.
- The following table shows the normal contents of the sediments:
| Normal contents of the urine | Findings in the normal sediments |
| White blood cells | Variable in males and females. Maybe 0 to 5 /HPF |
| Red blood cells | Variable and maybe 0 to 2 /HPF |
| Epithelial cells | Variable in males and females but more in females 1 to 5 /HPF |
| Bacteria | Negative |
| Hyaline cast | 0 to 2 /HPF |
| Abnormal crystals | Not Found |
Microscopic contents
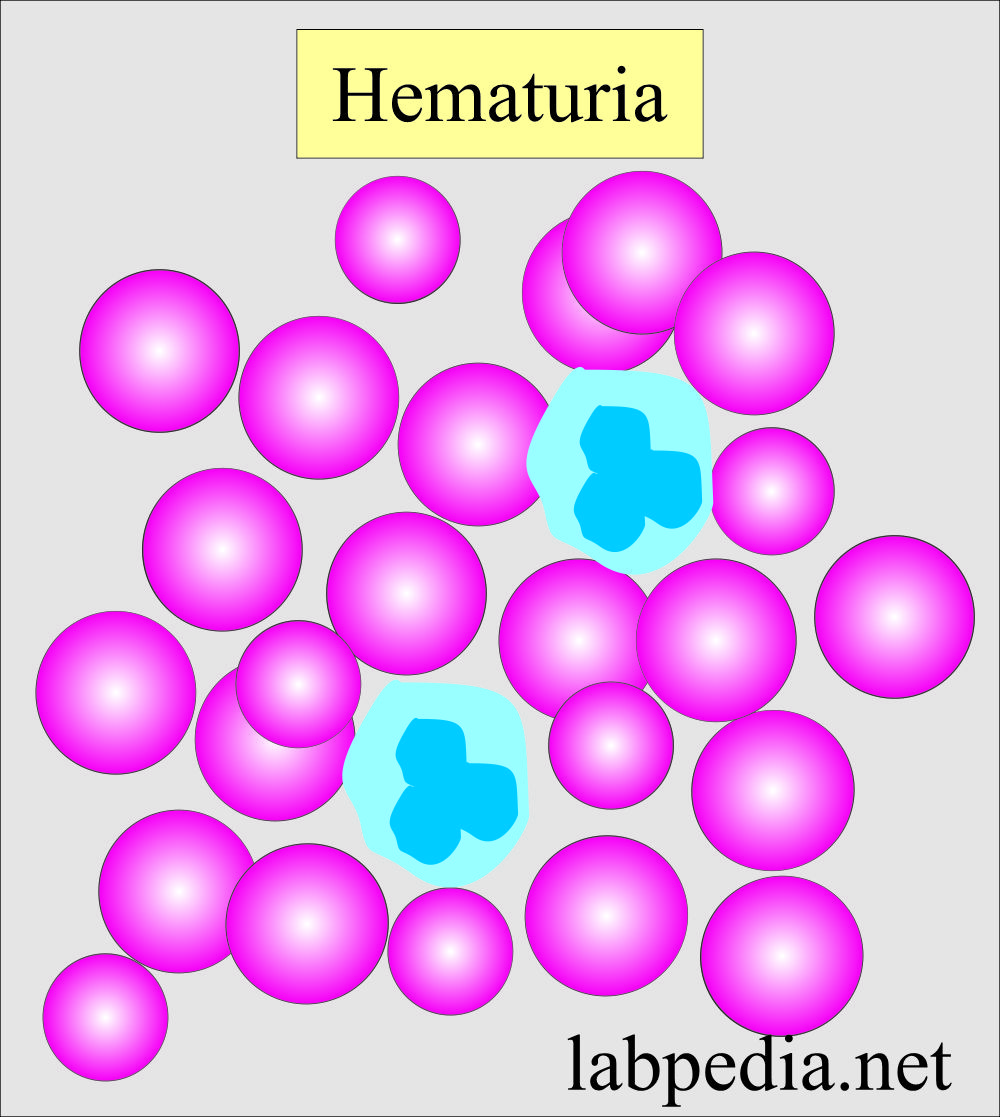
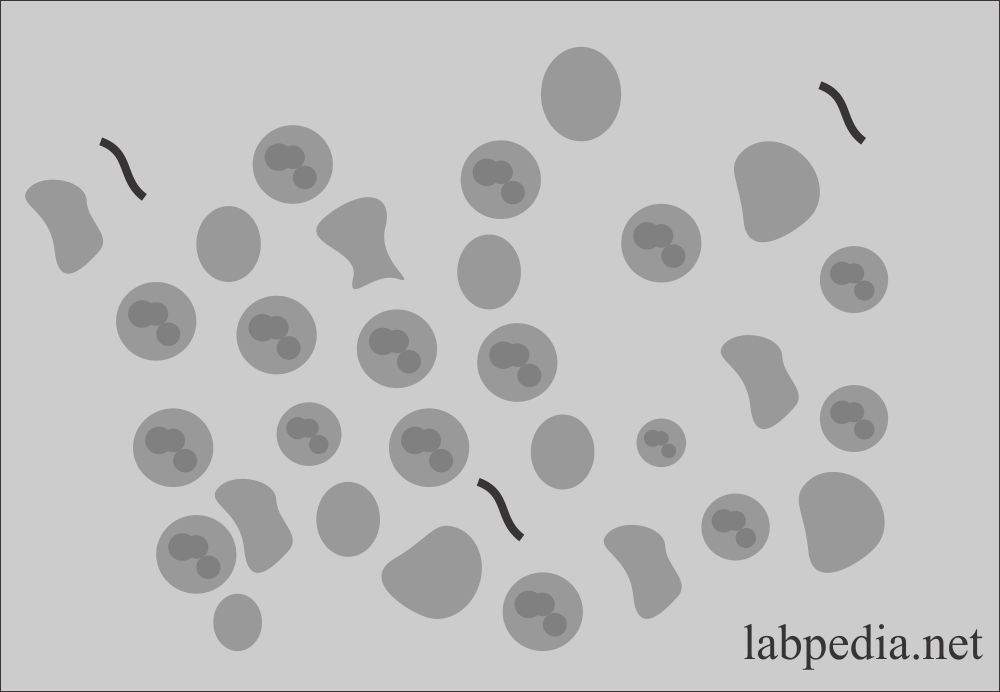
Red blood cells
- The presence of RBC in the urine is called Hematuria.
- RBCs are seen as biconcave, non-nucleated discs measuring 7 µm in diameter.
- The presence of RBC is an indicator of renal disease.
- These are reported in a routine as the average number seen in 10 HPF (x400).
- RBCs swell and lyse rapidly in the diluted urine, releasing their hemoglobin and leaving only the cell membrane; these empty cells are called ghost cells. These can only be seen in reduced light. Otherwise, these are missed.
- RBCs are confused with:
- Yeast.
- Oil droplets.
- Air bubbles.
- How to differentiate RBCs:
- Oil droplets and air bubbles are highly refractile.
- These are seen on a different level than the other sediments.
- RBCs are smaller than WBCs.
- Add acetic acid to the sediment, lyse the RBCs, and leave behind yeast, oil droplets, and air bubbles.
- Or do the supravital staining.
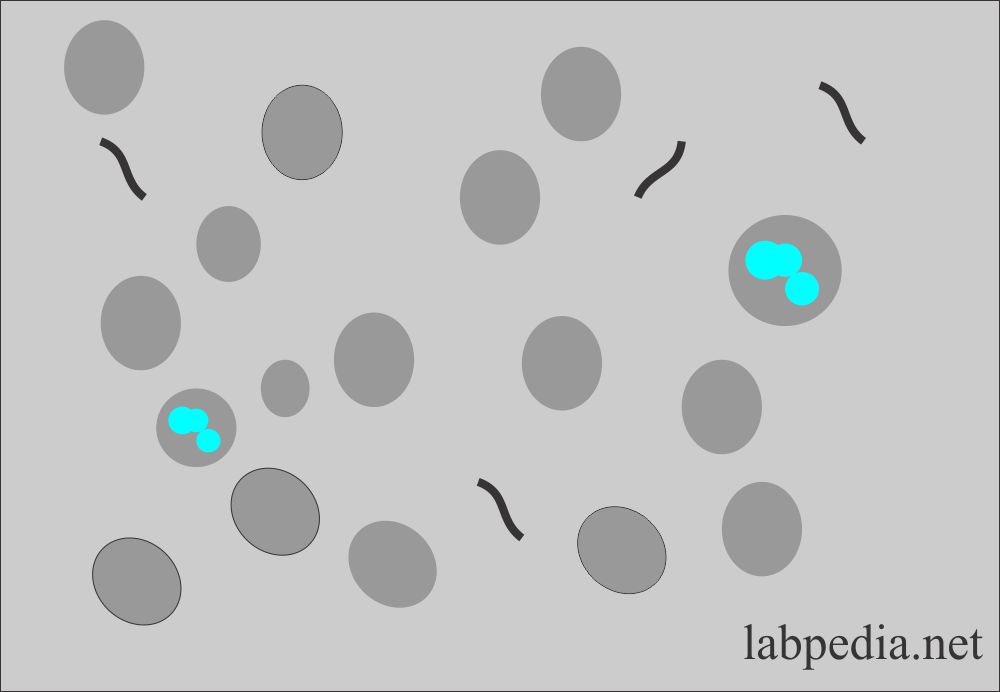
Dysmorphic RBCs:
- These RBCs vary in size, have cellular protrusions, or may be fragmented.
- Wright’s stain can also help to differentiate these RBCs as hypochromic and prominent cellular blebs and protrusion.
- These RBCs are associated with glomerular bleeding.
- These are also seen after strenuous exercise, indicating glomerular RBCs.
Macroscopic hematuria:
- It shows cloudy urine with a red to brown-color.
- This is seen in the following:
- Trauma.
- Acute infection.
- Inflammation.
- Coagulation disorders.
Microscopic hematuria is seen in:
- Glomerular diseases.
- Malignancy of the urinary tract.
- Renal calculi.
- The possibility of menstrual contamination should be considered in females.
Hematuria may be caused by the following:
- Renal disease
- Infections
- Renal stones
- Renal tumors
- Bleeding disorder.
- Anticoagulant therapy.
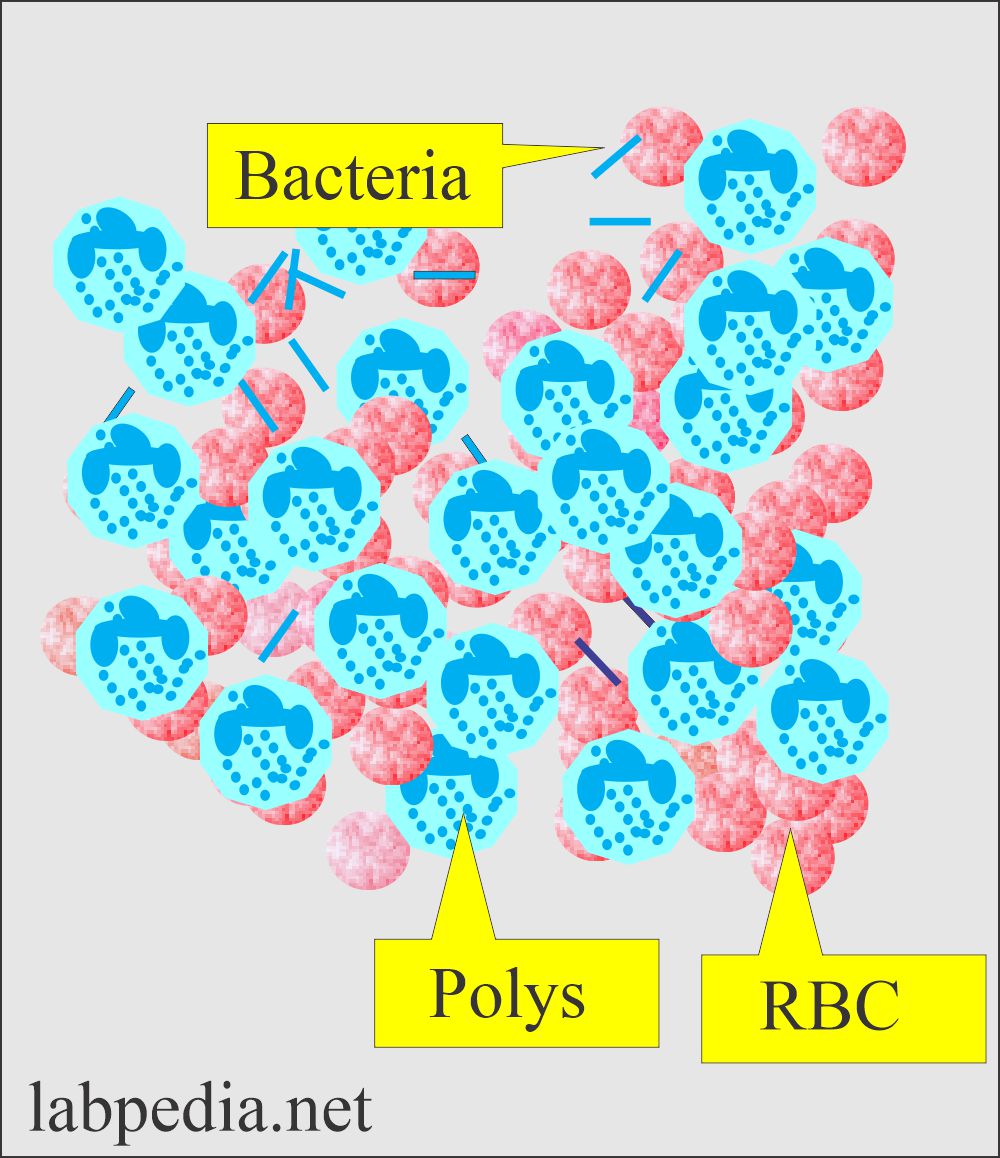
White Blood Cells (WBC), Neutrophils
- WBCs are bigger than the RBCs measuring an average of 12 µm in diameter.
- In the urine sediment, recognizing the WBCs is easy compared to RBCs.
- Neutrophils contain multilobate nuclei and granules in the cytoplasm.
- WBCs can be identified in the high power and reported as the average number in 10 HPF.
Urine analysis: Urine WBCs in the sediment
- Neutrophils lyse rapidly in the dilute alkaline urine and begin to lose nuclear details.
- An increased number of WBCs in the urine is called Pyuria.
- Pyuria may be caused by :
- Bacterial infection of the urinary tract
- Acute pyelonephritis shows casts along with WBCs, proteins, and bacteria.
- Lower urinary tract infection also shows WBCs but a small amount of protein.
Normal WBCs number:
- Normally few Neutrophils are seen.
- Usually 4 to 5 /HPF.
- >30 cells /HPF is considered an infection.
- WBCs clumps are a sign of infection and must be reported
Increased neutrophils are seen in:
- All renal inflammatory diseases.
- Glomerulonephritis.
- Cystitis and urethritis.
- Chronic pyelonephritis.
- Prostatitis.
- Pyogenic infection.
- Acute appendicitis.
- Acute pancreatitis.
- Tuberculosis.
- Urinary bladder tumors.
Nonbacterial increased WBCs are seen in:
- SLE.
- Interstitial nephritis.
- Glomerulonephritis.
- Tumors.
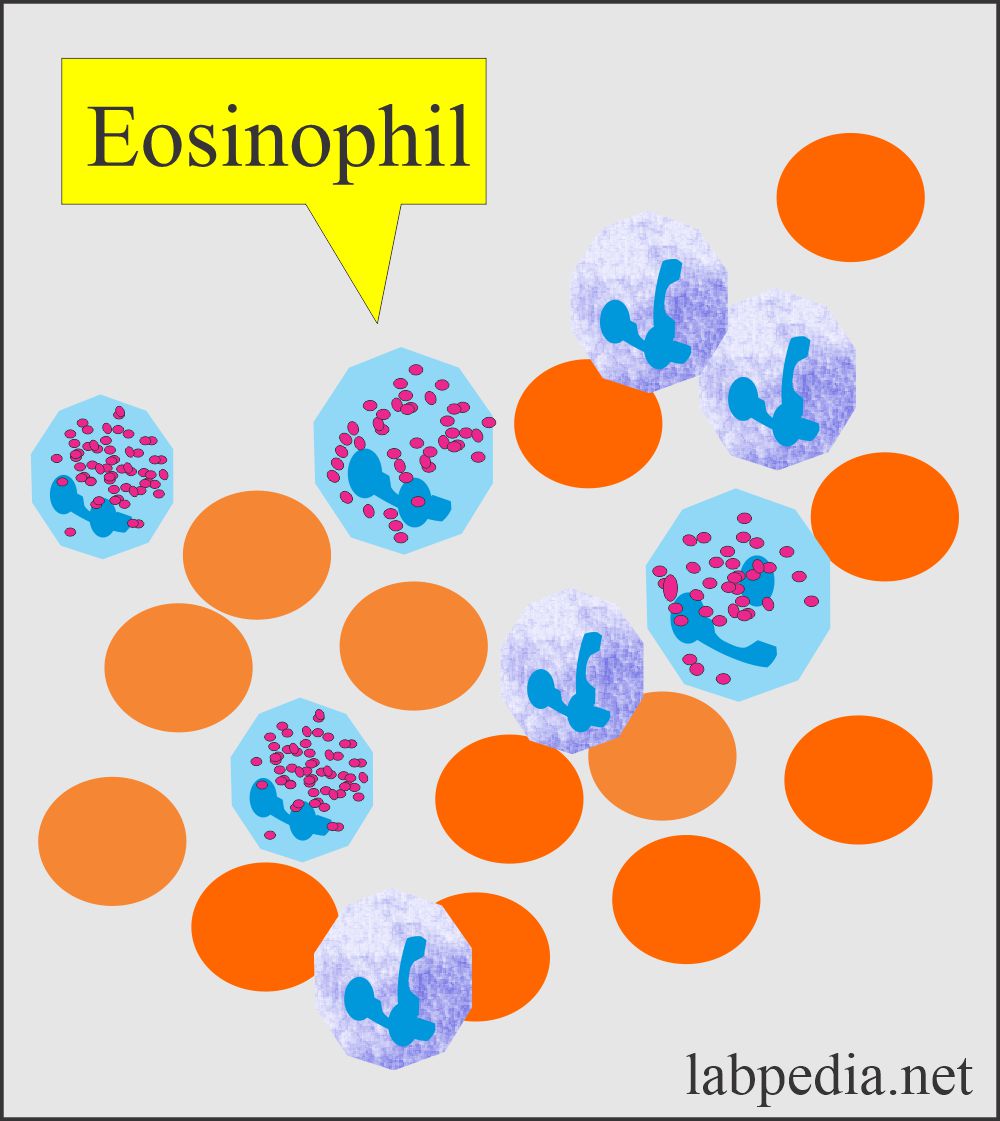
Eosinophils
- Eosinophils usually are not seen in the urine sediment. It may be seen in a few, along with neutrophils.
- On wet preparation, eosinophils are difficult to recognize except for the presence of 2 or 3 lobes.
- The supravital stain detects these.
- Use Wright’s stain or a special stain for eosinophils like Methylene-blue and eosin-Y in methanol.
- Eosinophils may be seen in:
- Drug-induced interstitial nephritis (hypersensitivity), e.g., penicillin and its derivatives.
- Acute genitourinary diseases like tubulointerstitial disease.
- These are also seen in renal transplantation rejection.
Procedure to see eosinophils:
- Centrifuge the urine; concentrated sediments are needed to stain it.
- Or prepare the smear with a cytospin centrifuge.
- The best stains are Hansel’s stains, but you can use Wright’s stains.
- >1% eosinophils are a significant number.
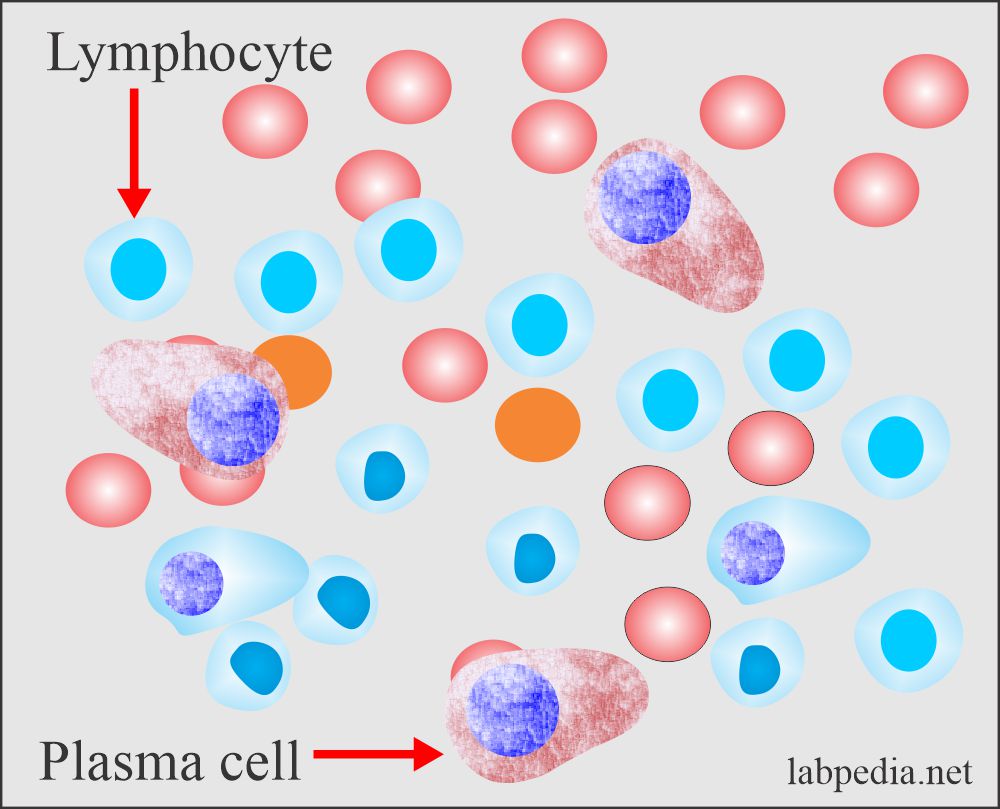
Lymphocytes
- Normal urine may contain a few small lymphocytes which are not recognized.
- Wright’s stain can recognize them.
- An increased number of lymphocytes is seen in the following:
- The first few weeks of renal transplantation are a sign of rejection.
- Many lymphocytes and plasma cells show renal transplantation rejection and acute renal allograft rejection.
Monocytes, Histiocytes, and Macrophages
- These cells are difficult to recognize in wet preparation. Normally there are monocytes, macrophagic cells, and histiocytes.
- Lymphocytes are smaller than WBCs and may resemble RBCs.
- Monocytes, histiocytes, and macrophages are large cells and are vacuolated with inclusions.
- Recognizing these cells needs a special stain (Wright’s and Papanicolaou’s stain).
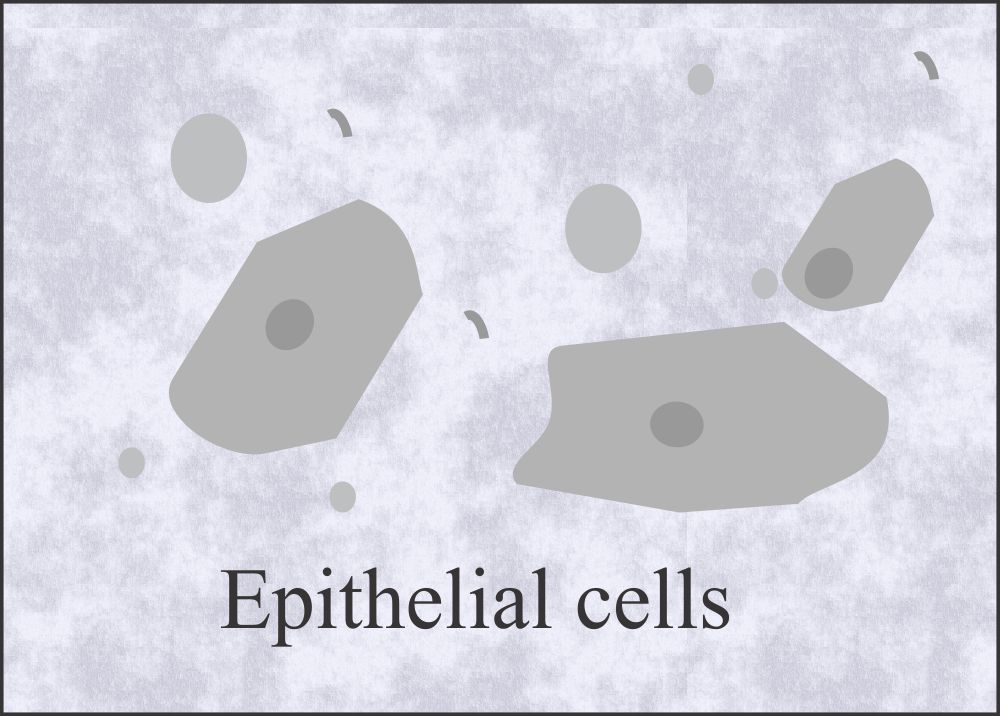
Epithelial cells
- Mainly these cells are shed from the urethra and urinary bladder.
- Few renal epithelial cells are seen normally in the sediment.
- Epithelial cells are the following types :
- Squamous epithelial cells
- Transitional epithelial cells
- Renal epithelial cells.
Squamous epithelial cells
- These cells line the female urethra, trigone, and male urethra.
- These cells also line the vagina, and in the female, these are the source of contamination.
- Origin: These squamous epithelial cells take origin from the vagina, female urethra, and lower portion of the male urethra.
- These represent normal sloughing and have no pathologic significance.
- Midstream clean catch will have less number of these cells.
- These cells have little significance but are helpful for focusing on the microscope.
- Morphology:
- These cells are large, containing abundant irregular cytoplasm and a prominent nucleus, which may be around the size of an RBC.
- The squamous epithelial cells are reported as follows:
- Rare
- Few.
- Moderate.
- Many.
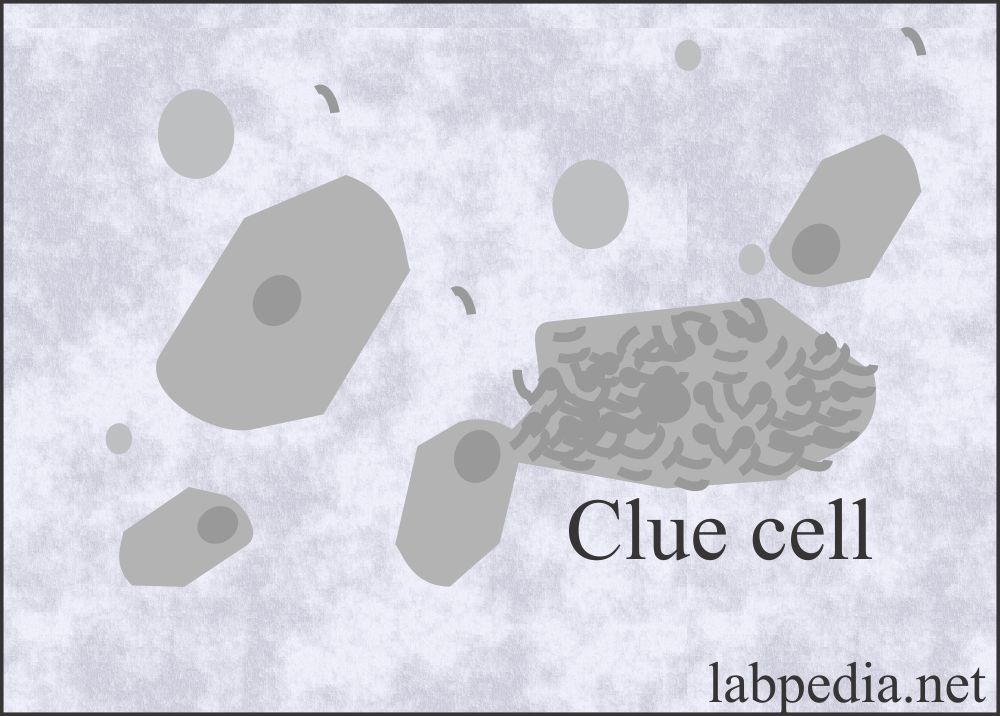
Clue cells
- These are a special type of squamous cell and take their origin from the vagina. These are covered by coccobacilli (Gardnerella vaginalis) and indicate bacterial vaginitis.
- A small number of clue cells may be present in the urine sediment.
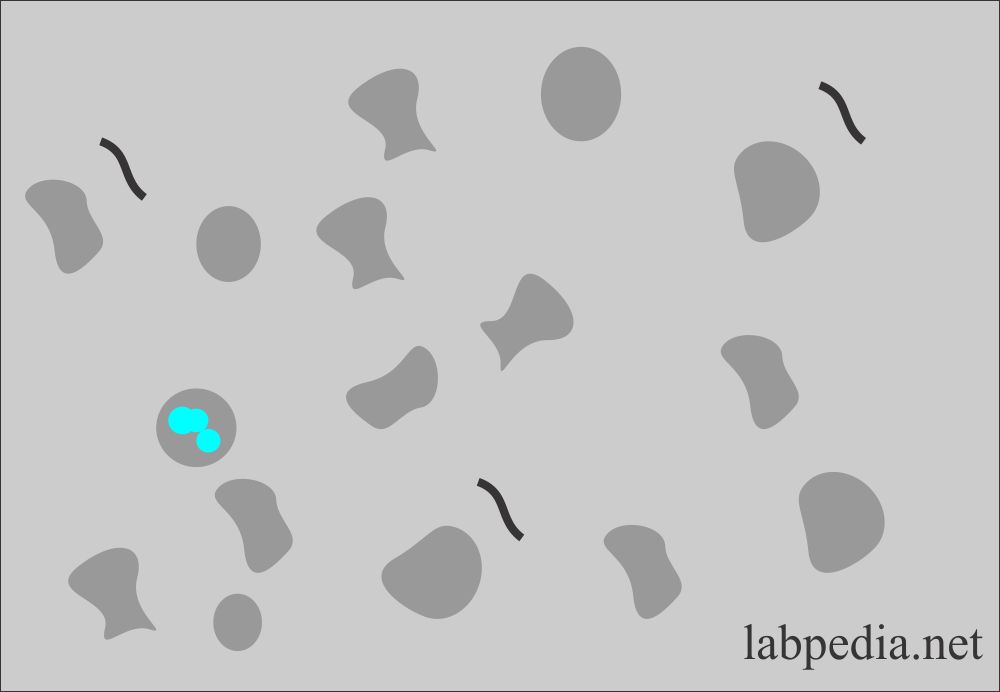
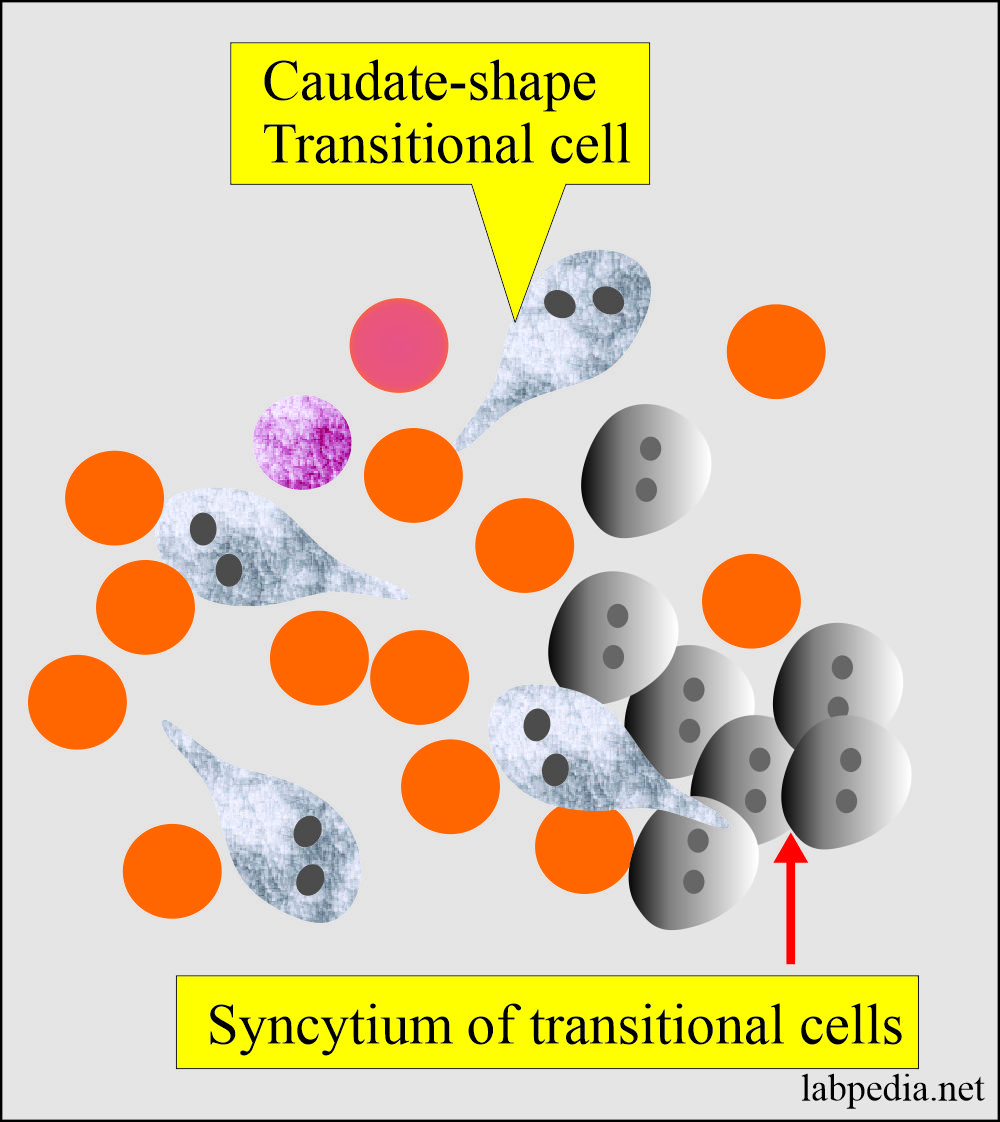
Transitional Epithelial cells
- These are stratified epithelial lining of the urinary tract system, starting from the kidney’s pelvis to the urinary bladder base in the female and proximal part of the male urethra.
- Morphology:
- These are smaller than the squamous epithelial cells.
- These have various shapes, like spherical, polyhedral, and caudate forms.
- All forms have a distinct central nucleus.
- These cells take origin from the lining of the renal pelvis, calyces, ureter, urinary bladder, and upper part of the urethra.
- Reporting of the Transitional cells:
- Normal urine may contain few transitional cells.
- Rare.
- Few.
- Moderate.
- Many.
- Renal cells exfoliate more in:
- Inflammatory process and infection.
- Malignancies.
- After radiation and these cells become large in size and have multiple nuclei.
- After catheterization or washing of the urinary bladder.
- These cells need special stains.
- An increase in the number of transitional epithelial cells with abnormalities like vacuoles in the cytoplasm and irregular nuclei may suggest malignancy or viral infection; such cases need cytological examination.
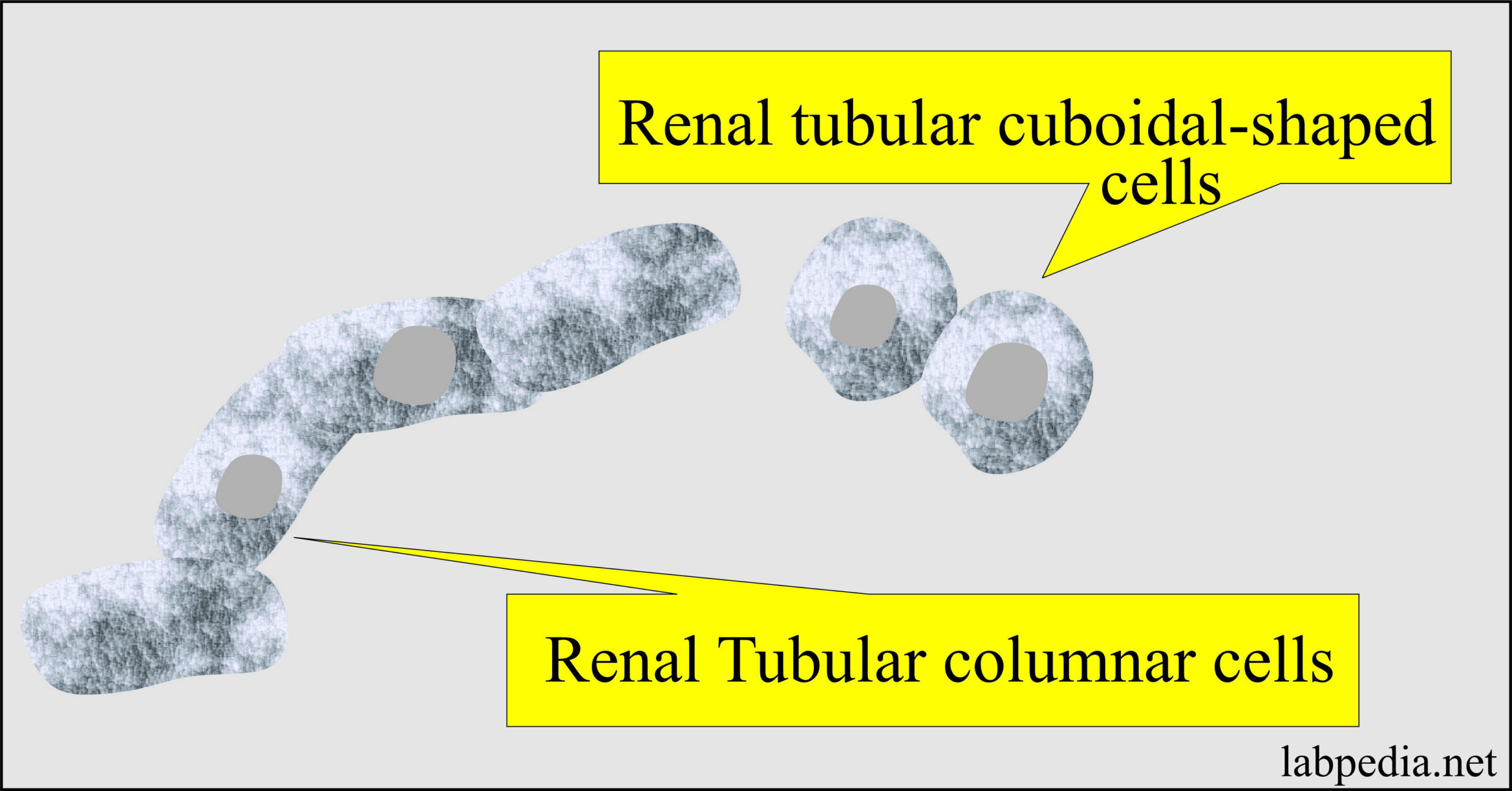
Renal Tubular Epithelial cells
- These cells line the proximal to distal convoluted tubules, small and large collecting ducts.
- Proximal convoluted tubular cells are rectangular, coarsely granular cytoplasm.
- Collecting duct cells are cuboidal to columnar, finely granular, and not larger than WBCs.
- Normally a few cells may be found in the urine sediment.
- An increased number is significant, indicating renal disease.
- The function of renal tubular cells:
- The main function of these cells is reabsorption.
- In hemoglobinuria, these cells contain yellow-brown hemosiderin pigments.
- In the case of bilirubin, the color of these cells is deep yellow.
- The critical number is more than 15 cells/10 HPF. When >2 cells are found, then refer to cytologic examination.
- Significance:
- When present in groups, it indicates severe renal damage.
- Acute tubular necrosis.
- It is seen in heavy metal poisoning.
- Drug-induced toxicity.
- Hemoglobin and myoglobin toxicity.
- Viral infections like HBV.
- Pyelonephritis.
- Viral infections.
- Allergic reactions.
- Acute allogenic Rejection phenomenon.
- Malignant infiltration.
- These are not easily identified in the centrifuged material. It needs special stains.
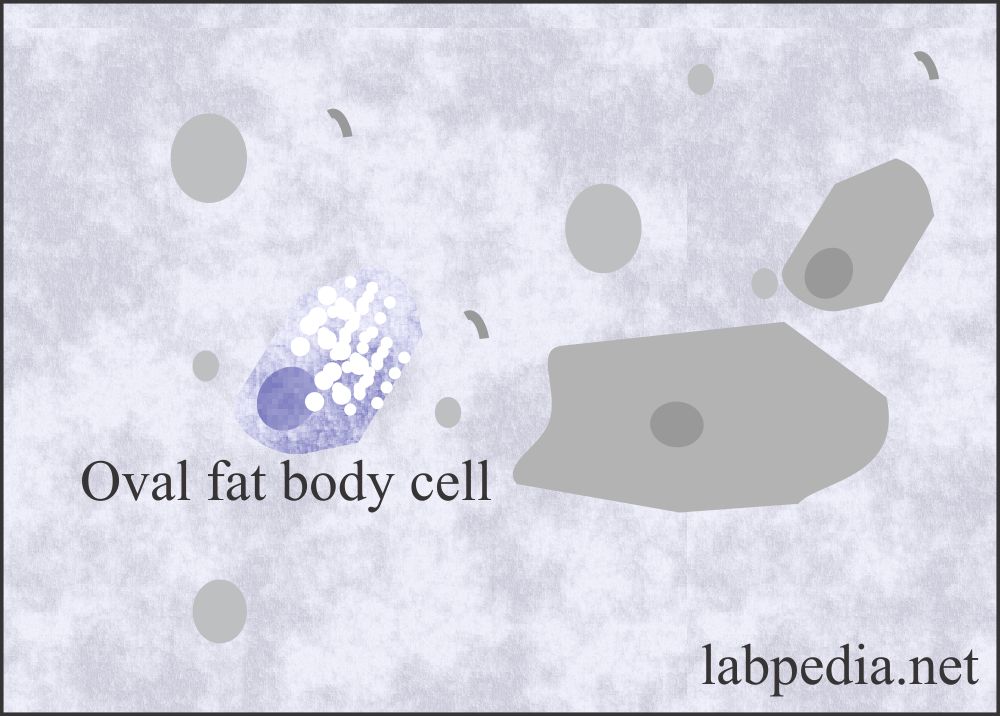
Fat Globules and Fat Bodies
- Tubular cells absorb the fat, which is present in the glomerular filtrate.
- These cells containing the fats are refractile, and the nucleus is difficult to see. These fat-containing renal tubular cells are called fat oval bodies.
- The special stain Sudan black III or oil red O fat stain can see these fat oval bodies. These are seen in the polarized microscope.
- These are seen along with fat globules or droplets.
- These fat droplets consist of triglycerides, neutral fat, and cholesterol.
- The fat stain will stain triglycerides and neutral fat and give orange-red color.
- The presence of fat in the urine is called lipiduria. This is usually seen in the case of damage to glomeruli in nephrotic syndrome.
- Special stain Sudan 111 or oil red O is needed.
- Lipiduria is seen in:
- Advanced diabetes mellitus.
- Severe tubular necrosis.
- Nephrotic syndrome.
- Lupus disease.
- In mercury poisoning.
- Ethylene glycol poisoning.
- In trauma where the bone marrow fats leak from the long bone.
- Lipid storage disease where there are large fat-laden histiocytes. These are differentiated from fat oval bodies by their large size.
Spermatozoa
- The spermatozoa are oval, slightly tapered heads and long flagellate-like tails.
- Urine is toxic to sperms, so they are nonmotile in the urine.
- There should be a lab protocol when reporting spermatozoa in the urine, particularly female urine. There may be legal consequences.
- These may be seen in males and females following intercourse (coitus).
- Spermatozoa in the urine is significant in infertility cases and sexual abuse.
- In males may be seen after a nocturnal emission or ejaculation.
- Also seen in diseases of the genital tract.
- Their presence in the urine is of significance in the case of retrograde ejaculation, where the sperms go into the urinary bladder instead of the urethra.
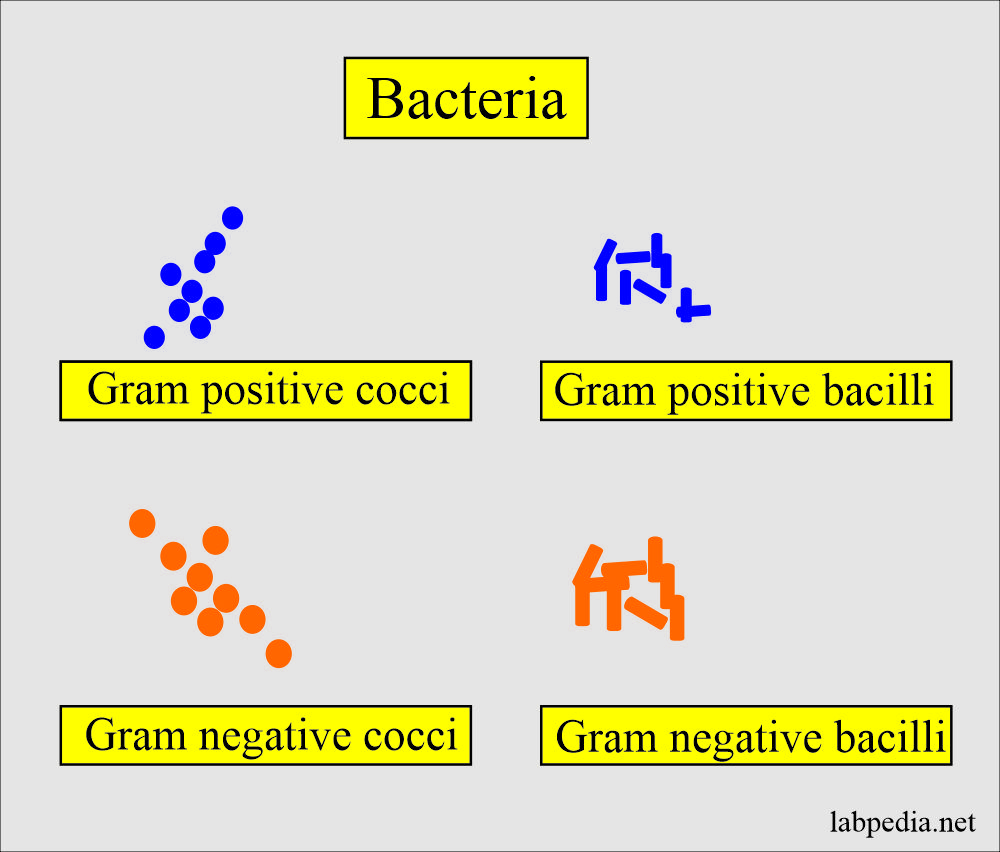
Bacteria
- Normally, few bacteria are present unless you collect the urine in strict sterile conditions.
- There are bacteria due to contamination from the vaginal secretions, urethra, genitalia, or the container.
- These bacteria multiply if the urine is left at room temperature and give a nitrite test positive and may result in pH 8, which indicates an unacceptable specimen.
- If urine is kept at room temperature in the lab, bacteria can multiply.
- When bacteria are seen in the urine, they should be reported per high power as:
- Few.
- Moderate.
- Many.
- When reporting bacteria, then you should see the WBCs in the urine.
Urine bacteria causing urinary infection:
| Type of bacteria causing infection | % of urinary tract infections |
| E.Coli | 72% |
| Klebsiella | 16% |
| Proteus | 5% |
| Staphylococcus | 5% |
| Pseudomonas | 1% |
| Streptococcus faecalis | 1% |
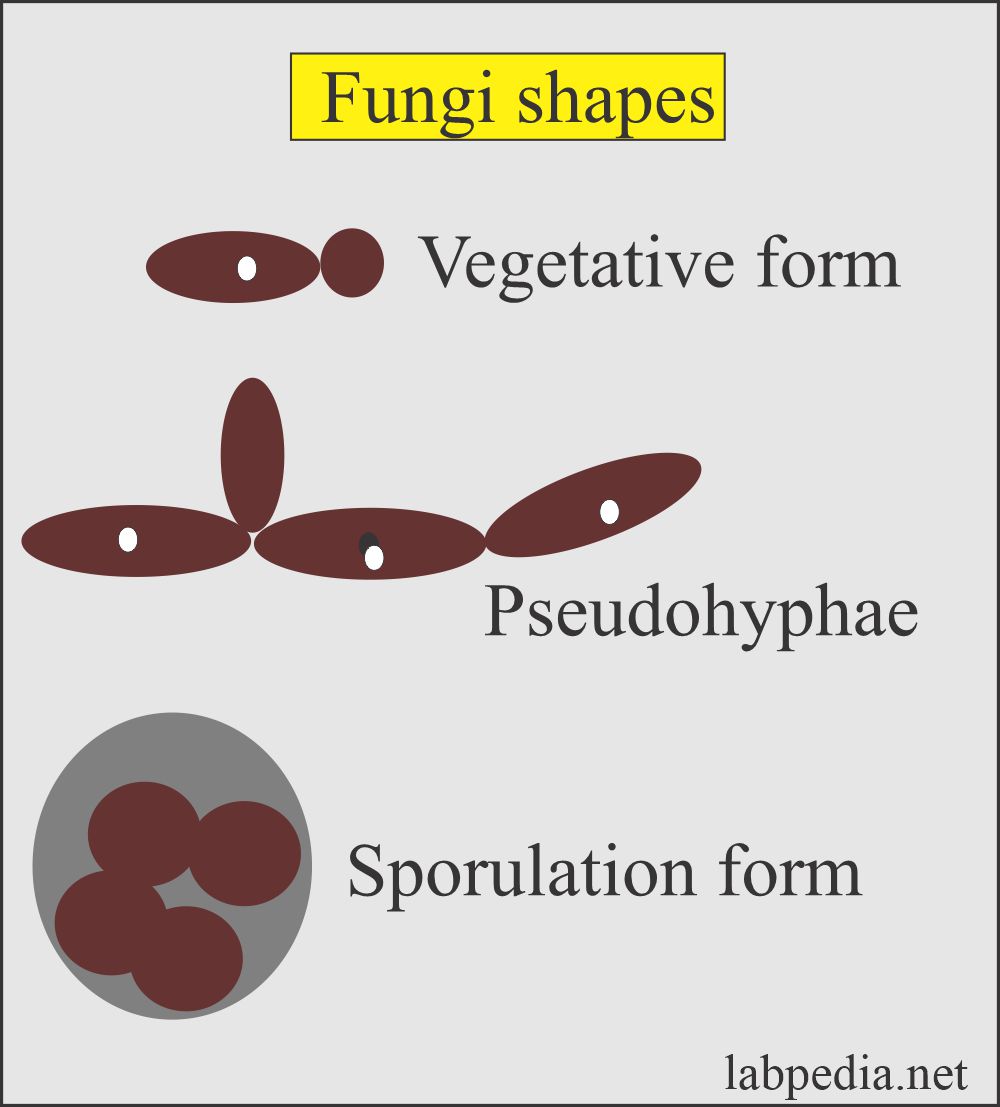
Yeast
- The most common yeast is candida in the urine.
- This may be vaginal contamination due to vaginal infection.
- This yeast, primarily candida, is seen in:
- The patients with diabetes. Because sugar is used as a source of energy for yeast growth.
- These are also seen in immunocompromised patients.
- Female with vaginal moniliasis.
- The infection is suspected when the presence of WBCs accompanies candida.
- Structure of yeast:
- These may be seen as small, refractile oval structures that may be laking buds.
- These are strongly gram-positive.
- Wright’s stain differentiates yeast from the RBCs.
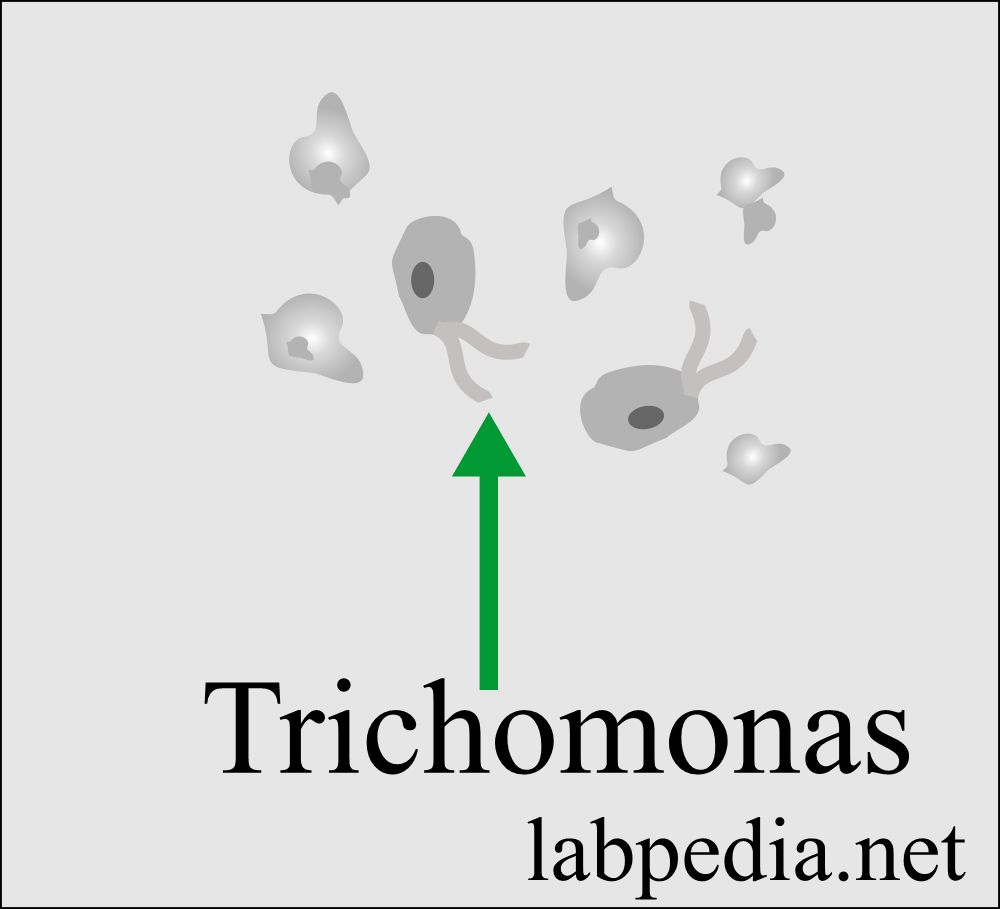
Trichomonas (parasites)
- This protozoan is the common cause of vaginal infection called Trichomonas vaginitis caused by Trichomonas vaginalis.
- Trichomonas is a sexually transmitted disease and causes inflammation in the female.
- While the infection of the male urethra and prostate is asymptomatic.
- Structure of Trichomonas:
- Trichomonas is a pear-shaped flagellate with an undulating membrane.
- It is easily identified in a wet preparation and the urine sediment by its rapid darting movement under the microscope.
- It is challenging to identify when these are not moving because they resemble WBCs or transitional cells.
- The trichomonas are reported /HPF:
- Rare.
- Few.
- Moderate.
- Many.
- These protozoa reside in the prostate and vagina.
- Wet preparation from the vagina or urethra by direct swab preparation can diagnose it.
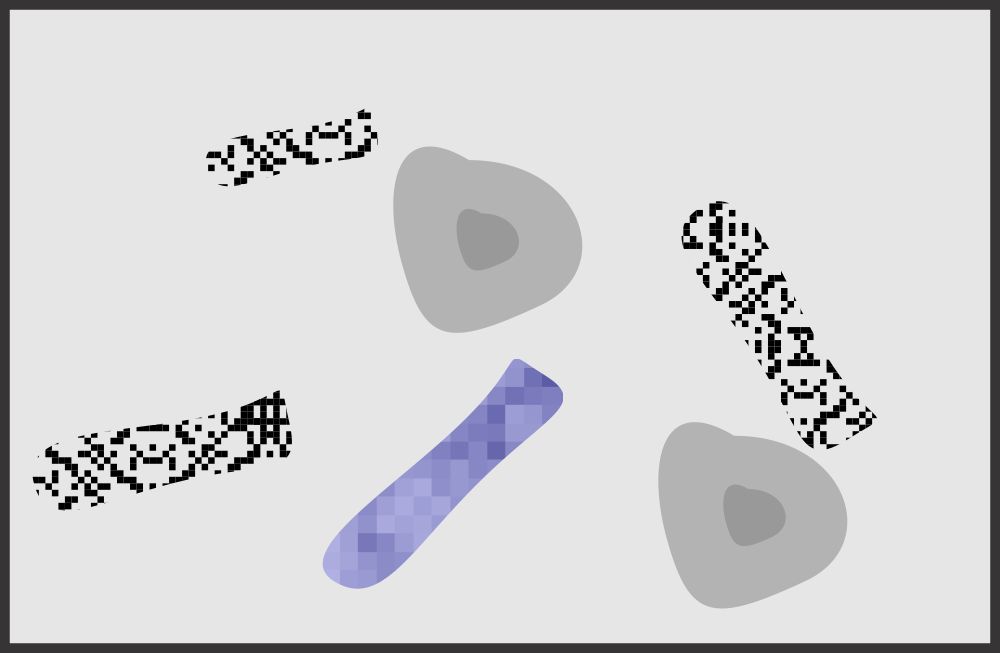
Casts
Formation of the cast:
- These casts are precipitated proteins in the tubules. It forms in the lumen of distal convoluted tubules and collecting ducts.
- Their shape is representative of the tubular lumen with parallel sides and mostly rounded ends.
- The shape and content of the cast depend upon:
- The material is present in the filtrate at the time of formation.
- Length of time, it remains in the tubules.
- Any other components present in the filtrate at the time of formation, like bacteria, granules, pigments, and crystals, may become embedded in or attached to the cast matrix.
- The casts dissolve easily in the dilute alkaline urine.
Composition of the cast:
- The major component is the Tamm-Horsfall protein. This protein is produced from the renal tubular epithelium and upper collecting ducts.
- Other proteins are albumin and immunoglobulins.
- These proteins gels under the following conditions:
- Urine flow stasis.
- The acidity of the urine.
- In the presence of Na+ and Ca++.
- Protein glycosylation is also important.
- The width of the cast depends on where the cast is formed.
- These casts lead to blockage of the urinary outflow in the tubules.
- Reporting:
- These are screened under low power and are usually seen at the edges of the coverslip.
- It also needs low light because the cast refractive index is low.
- After identifying under the low light, go to high-power magnification and report cast number / 10 HPF.
- There are the following types of casts seen in the urine:
- Hyaline cast
- Cellular cast
- Waxy cast
- Granular cast
- Pigmented cast (maybe hemoglobin, myoglobin, bilirubin, and drugs casts)
- Fatty cast
- Inclusion cast
Hyaline casts
- Hyaline casts are the most common casts.
- This cast mainly consists of Tamm-Horsfall protein. These are colorless in unstained sediments, and the refractive index is like urine.
- These can be easily seen in phase microscopy.
- Or stain with Sternheimer-Malbin, which produces the pink color of these casts.
- These are of the least importance.
- Normal:
- There may be <2 / PHF seen in a normal person (0 to 2 /HPF are normal).
- These may be seen without any significant proteinuria.
- These are seen in acidic urine and absent in alkaline urine.
- Normally Hyaline casts are seen in the following:
- After severe exercise.
- Dehydration.
- Emotional stress.
- Heat exposure.
- Pathologically hyaline casts are seen in:
- Acute glomerulonephritis.
- Chronic renal disease.
- Pyelonephritis.
- Congestive heart failure.
- > 20 / PHF is seen in moderate or severe renal disease.
Granular casts
- Structure:
- Granulat cast appears homogenous, coarsely granular, colorless, and very dense.
- These casts consist of a breakdown of cells, and plasma protein aggregates (fibrinogen, immune complexes, and globulin in the Tamm-Horsfall matrix).
- Normal:
- Few may be seen in a normal person or after vigorous exercise.
- Occasional 0 to 2 /HPF.
- Granular casts are seen in:
- Acute tubular necrosis.
- Pyelonephritis.
- Advanced glomerulonephritis.
- Malignant nephrosclerosis.
- The increased number indicates severe renal disease.
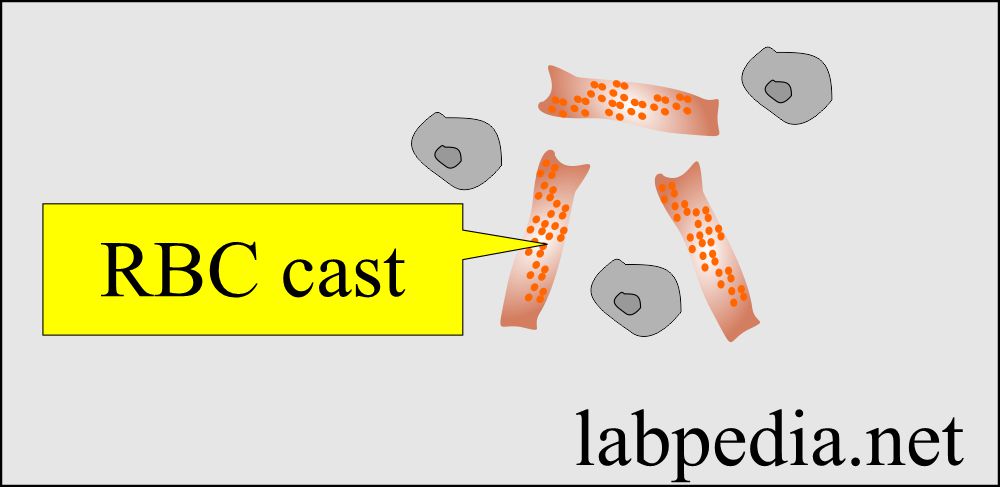
- Presence of cells in the cast:
- Red cells in the cast indicate a glomerular injury.
- The presence of epithelial cells indicates renal tubular injury.
- The presence of WBC indicates infection or interstitial injury.
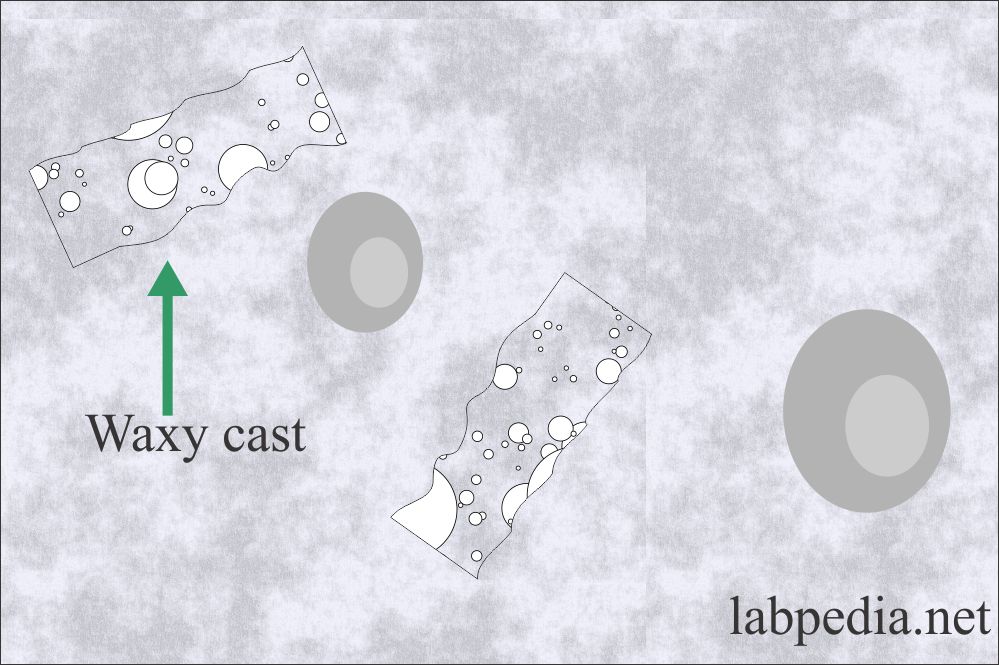
Waxy casts
- These are not seen normally in the urine.
- Structure and formation
- Waxy casts formed from the degeneration of the granular cast.
- These casts are larger than the other casts and are waxy and granular in appearance.
- These are broader than other casts and called broadcast or broad renal failure casts.
- These are like the hyaline cast, but these are more refractile and sharper outlines.
- These are also called renal failure casts.
- Their presence indicates severe pathology.
- Waxy casts are seen in:
- Chronic renal disease.
- Severe renal failure.
- Renal amyloidosis.
- These are rare in acute renal disease.
- Malignant hypertension.
- Renal amyloidosis.
- Diabetic nephropathy.
- Renal allograft rejection.
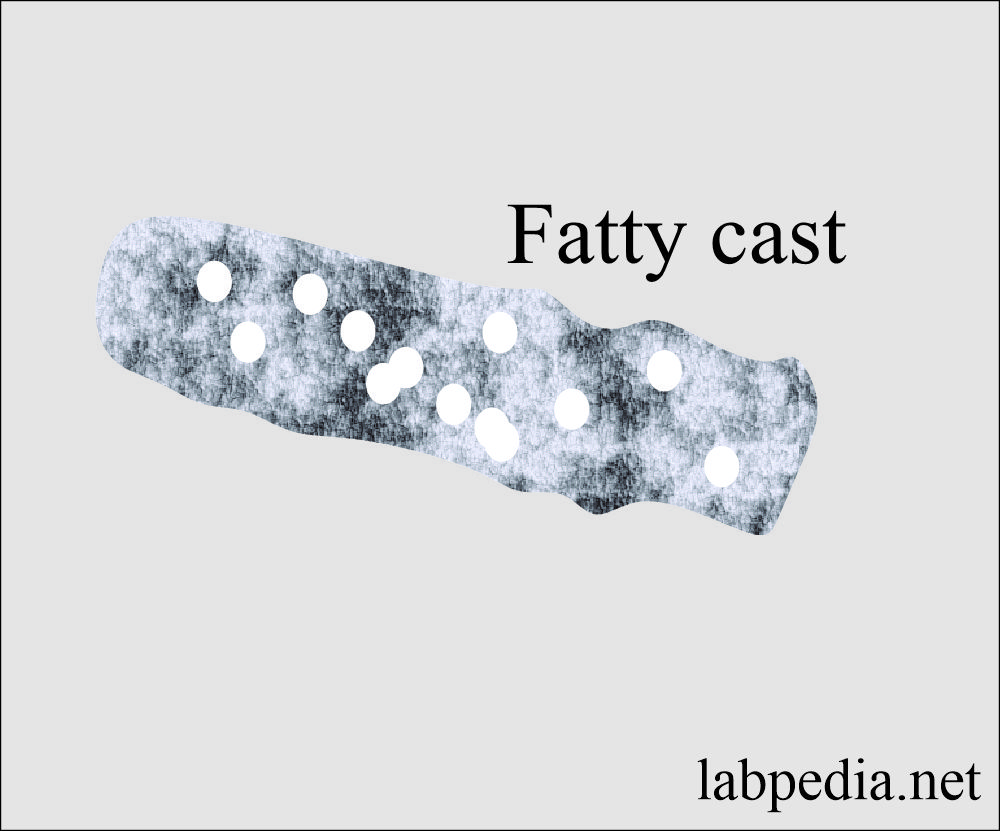
Fatty casts
- Formation:
- Fat casts are formed from the fat droplets’ attachment and degenerating fat oval bodies embedded in the protein matrix.
- Fatty casts are highly refractile and contain yellow-brown fat droplets or fat oval bodies.
- These also indicate serious renal disease.
- These are seen in the following:
- Nephrotic syndrome.
- Chronic glomerulonephritis.
- Severe diabetes mellitus.
- Toxic nephrosis due to mercury poisoning and ethylene glycol.
- SLE.
- Toxic renal poisoning.
Red Blood Cell cast
- Fresh RBCs cast retain their brown pigments and consist of RBCs in a tubular cast matrix.
- These casts indicate intraparenchymal bleeding.
- These are the hallmark of glomerulonephritis.
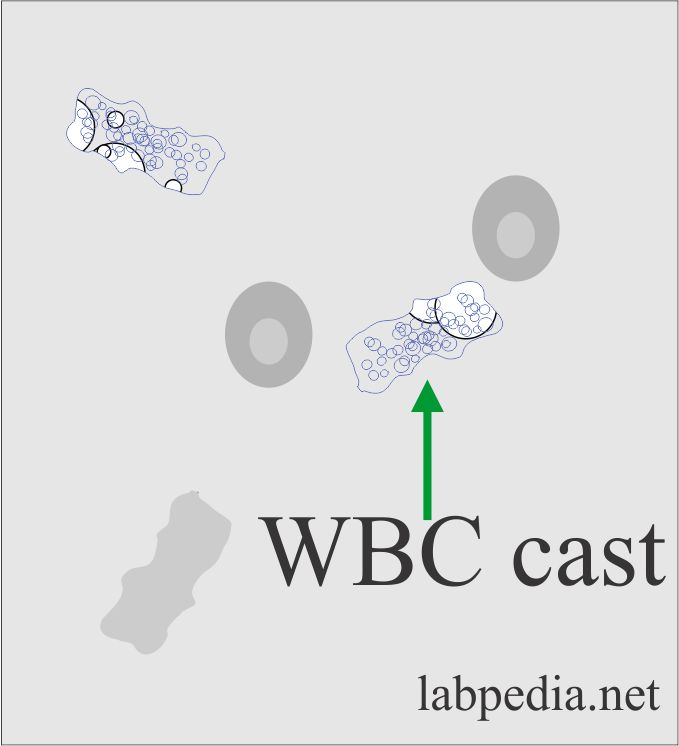
White Blood Cell cast
- There are WBCs in a protein matrix.
- These take origin from kidney tubules.
- WBC casts are seen in the following:
- These are characteristics of pyelonephritis.
- Interstitial nephritis.
- Tubulointerstitial infection.
- These are used fully to distinguish from lower urinary tract infections.
- Normal:
- Not seen normally.
Tubular Cell Cast
- There are few tubular cells in a hyaline matrix of dense aggregates of shed tubular cells.
- These are seen in concentrated urine.
- Tubular cell sloughing occurs in acute tubular necrosis.
Table: The type of cast and its association with various diseases:
| Type of cast | Clinical disease association |
| Hyaline | After strenuous exercise |
| RBC | Glomerular disease |
| WBC | Tubular diseases |
| Granular | Tubulointerstitial diseases |
| Waxy | Severe chronic renal disease |
| Fatty | Diabetic nephropathy |
Casts in the urine and their etiology:
| Nature of the cast | Physical appearance | Possible reason |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
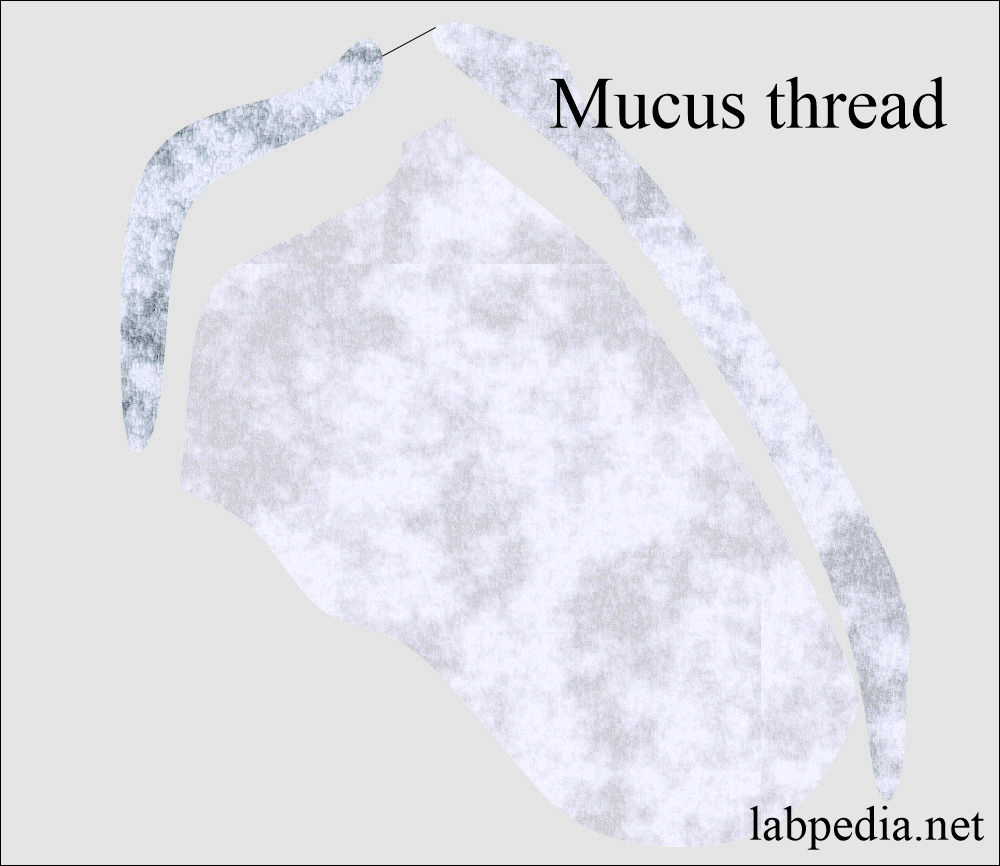
Mucous threads
- Mucus is a protein produced by the glands and the lower genitourinary tract’s epithelial and renal tubular cells.
- The main components of the mucus are the Tamm Horsfall protein.
- These may be mistaken for hyaline casts.
- These are long threads, undefined edges, and pointed or irregular ends.
- Mucus has a low refractive index.
- Mucus threads are reported as:
- Rare.
- Few.
- Moderate.
- Many or abundant.
- It has no clinical significance in males as well as females.
Questions and answers:
Question 1: What is the significance of the trichomonas in the urine?
Question 2: What is the significance of RBC cast?
Please see more details in urine analysis part 1.