Liver Function Tests:- Part 2 – Bilirubin Metabolism, and Jaundice
Bilirubin Metabolism
Sample for Bilirubin
- It is done on the serum of the patient.
- Heparinized plasma can be used.
- A random sample can be taken.
- The serum is stable for 3 days at 1 to 6 °C.
Precautions for Bilirubin Metabolism
- Avoid hemolysis.
- For bilirubin, a fasting sample is preferred.
- Protect serum or plasma from the light.
- Lipemia also falsely increased the value.
Purpose of the test (Indications)
- LFT diagnoses any liver disease.
- LFT has been done for follow-up of the patient on treatment.
- LFT is done routinely in patients on chemotherapy.
- LFT may be advised in a patient with treatment on antituberculous treatment.
What tests are included in routine LFT:
- Bilirubin.
- Bilirubin total
- Bilirubin is direct and indirect.
- SGPT.
- SGOT.
- Alkaline phosphatase
- Total protein.
- Albumin.
Additional liver function test:
- γ – GT (gamma – GT)
- Viral hepatitis profiles like HBV, HCV, HAV, HDV, HEV, etc.,
Steps in the diagnosis of Jaundice:
- Clinical history of the patient and examination.
- Stool examination for ova and parasite.
- Occult blood in the stool is positive for cancers.
- Urine examination:
- The persistent absence of the urobilinogen indicates obstructive jaundice.
- Bilirubinuria is an early sign of viral hepatitis.
- Negative urobilinogen and bilirubin indicate hemolytic anemia.
- Dark urine and clay-colored stool indicate hepatocellular or cholestatic jaundice.
- Advise biochemical tests like LFT, serum albumin, alkaline phosphatase, γ-GT, PT, total proteins, and immunoglobulin quantitation.
- Hematological work-up like CBC, reticulocytes, and Coomb’s test.
- Serological tests include ANA, Mitochondrial antibody, IgG, IgA, IgM, hepatitis viral profile, and AFP.
- Radiology include X-Rays, plain X-Ray abdomen, USG, and CT scan.
- Special tests like α1-antitrypsin, amylase, ceruloplasmin, iron, and IBC.
- Needle biopsy or FNA.
Functions of the liver:
- The liver is a multifunctional organ involved in various functions like excretory, synthesis, detoxification, storage, and metabolism.
- It can store (storage function):
- Amino Acids.
- Carbohydrates.
- Lipids.
- Vitamins.
- Minerals.
- It can synthesize (metabolic function):
- Protein, like albumin, alpha, and beta globulins.
- Coagulation factors.
- Transport proteins.
- Bile acids from cholesterol.
- The liver is the site for detoxification of:
- Drugs.
- Toxins.
- Its major function is Conjugation:
- bilirubin combines with glucuronic acid as:
- Bilirubin Monoglucuronide.
- Bilirubin diglucuronide.
- bilirubin combines with glucuronic acid as:
- The liver has an excretory function:
- Excrete bilirubin into bile.
- Bile acid is excreted into the bile.
- The liver is also the site of catabolism of:
- Thyroid hormone.
- Steroids hormones.
- Few other hormones as well.
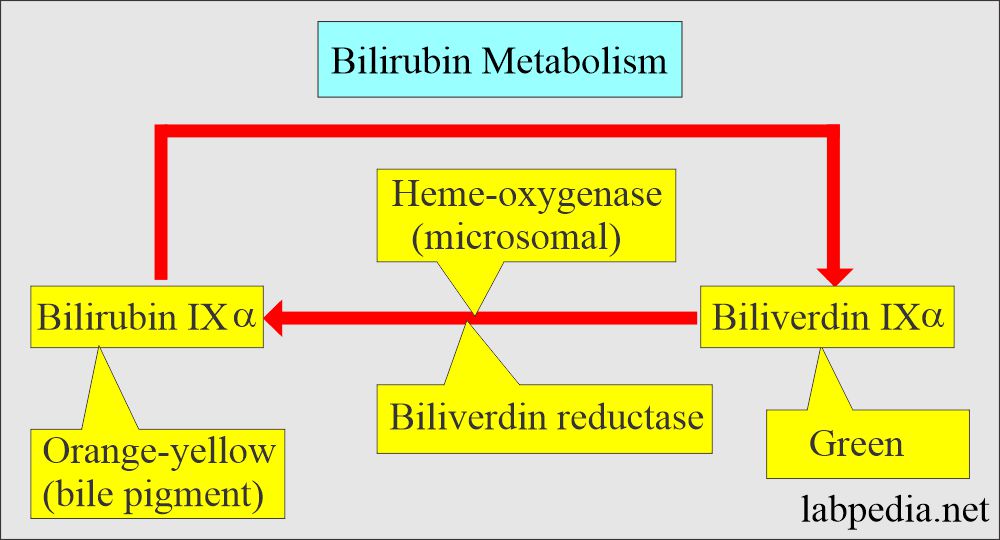
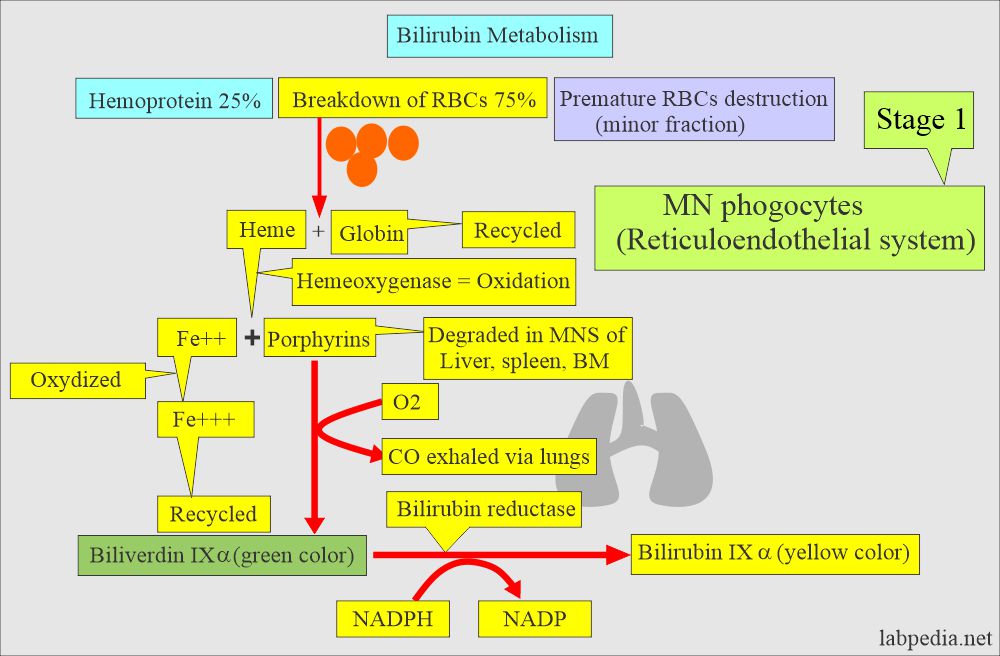
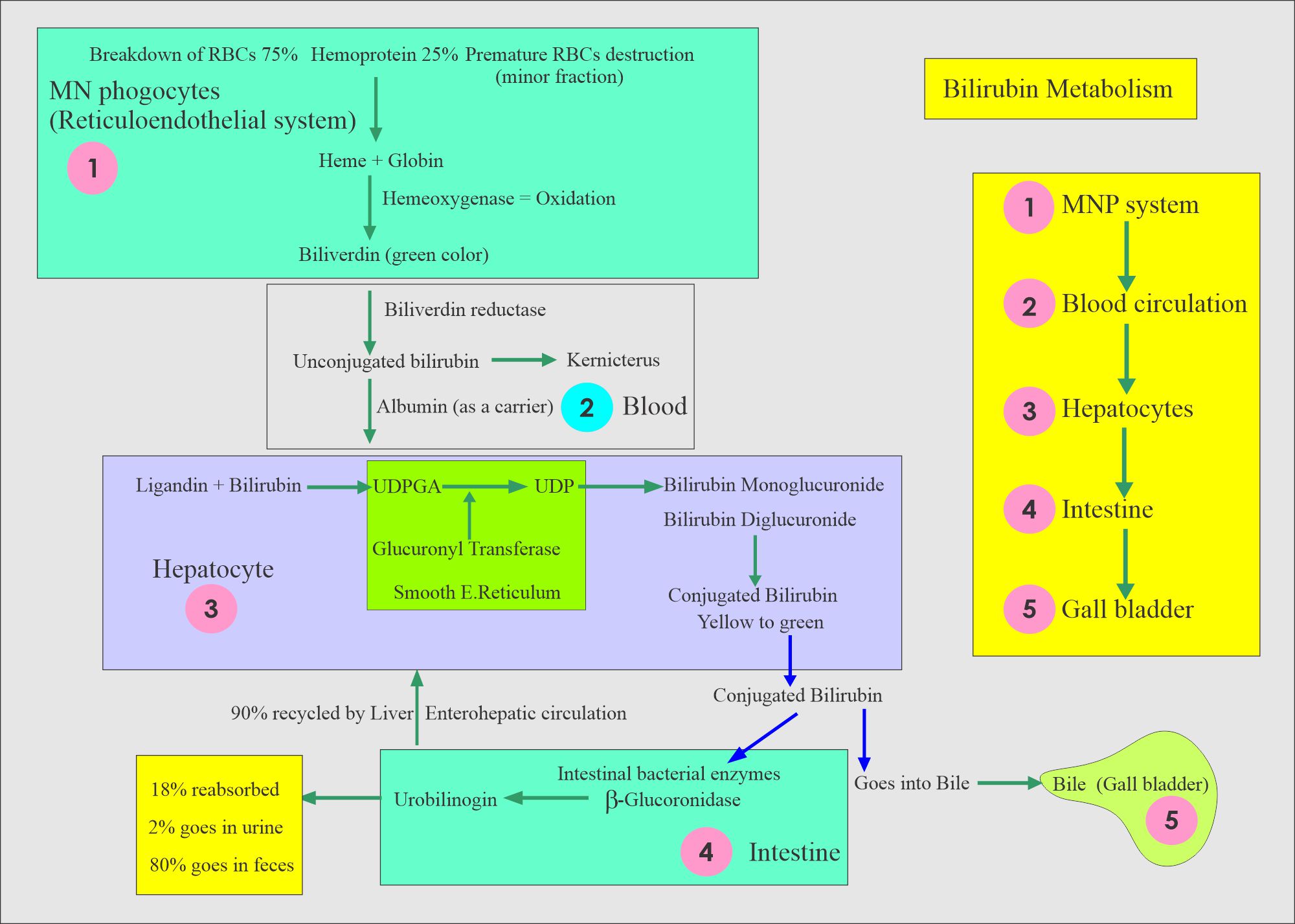
Bilirubin metabolism (How bilirubin forms):
Changes in the mononuclear phagocytic system:
- The breakdown of the RBCs is a major source for the formation of Globin and heme.
- Heme changes into Biliverdin and releases iron recycled to form RBCs in the bone marrow.
- Biliverdin forms the unconjugated bilirubin, which is fat-soluble.
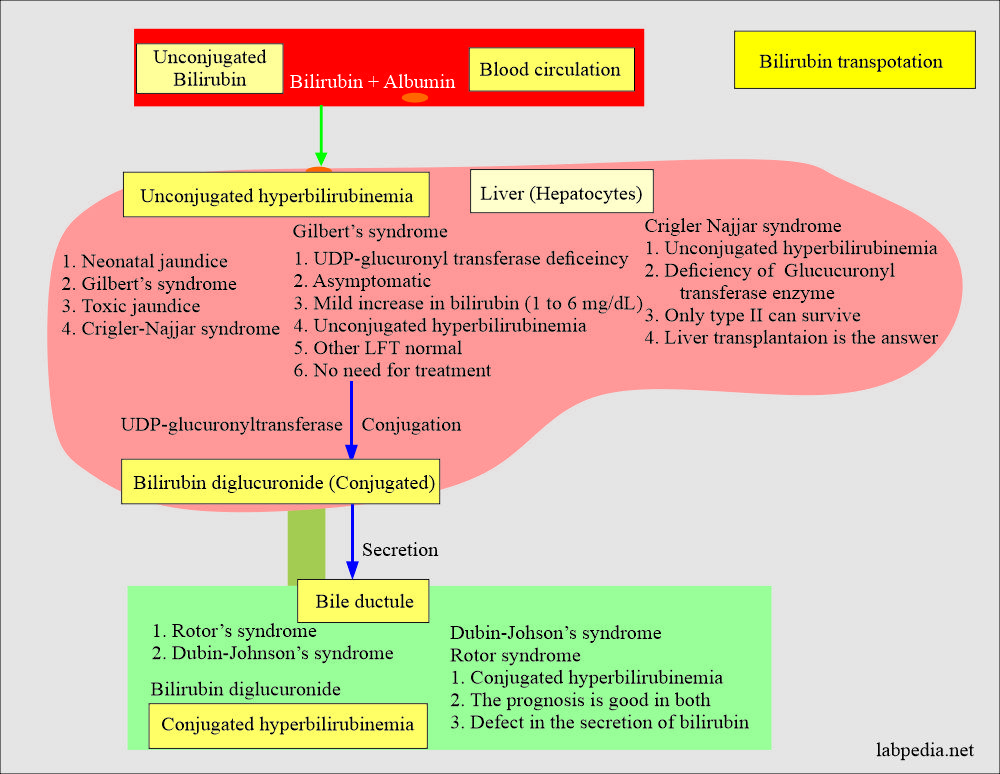
Changes in the liver cells:
- Unconjugated bilirubin is in the presence of glucoronyl transferase enzyme conjugated with glucuronic acid.
- There is the formation of monoglucuronide and diglucuronide (conjugated bilirubin).
- Conjugated bilirubin enters the enterohepatic circulation.
- Bilirubin 95% is excreted into bile in the form of:
- Glucuronide.
- ∼90% is diglucuronide.
- ∼10% is monoglucuronide.
- Glucosides.
- Xylosides.
- Glucuronide.
Changes in the intestine:
- Bilirubin is hydrolyzed by the catalytic action of β-glucuronidase from the liver, intestinal epithelial cells, and bacteria.
- The unconjugated bilirubin is reduced by the anaerobic intestinal bacterial flora to form a group of three colorless tetrapyrroles called urobilinogen:
- Stercobilinogen.
- Mesobilinogen.
- Urobilinogen, 20%, reabsorbed from the intestine and entered the enterohepatic circulation.
Bilirubin excretion in the urine:
- When bile reaches the duodenum, it is acted by the intestinal bacteria, which will convert most of the bilirubin into urobilinogen.
- Most urobilinogen is lost in the stool, but part is absorbed into blood circulation.
- In the blood, urobilinogen goes to the liver (Enterohepatic circulation) and is excreted by the hepatic cells.
- Some of this urobilinogen is excreted by the kidneys and excreted in the urine.
- Conjugated bilirubin, like urobilinogen, is partially excreted by the kidneys in case the serum level is raised.
- Unconjugated bilirubin can not pass through the glomeruli, so it does not appear in the urine.
- In case of an increased level of unconjugated bilirubin, there is an increase in the conjugated bilirubin, which will enter the bile duct, The intestine, and more urobilinogen is produced.
- This additional urobilinogen is absorbed into the blood circulation and appears in the urine.
- Urobilinogen is found in the urine when there is increased production of unconjugated bilirubin.
The extrahepatic fate of bilirubin:
- Water-soluble bilirubin is stored in the gallbladder and released into the intestine.
- Through enterohepatic circulation excreted in the feces and in the urine.
- In the urine is excreted as urobilinogen.
- In the stool as stercobilinogen.
- The three urobilinogen in the lower intestinal tracts produce bile pigments:
- Stercobilin.
- Mesobilin
- Urobilin.
- These are orange-brown and are major pigments of the stool.
Definition of Jaundice
- This is defined as the yellow discoloration of the skin and sclera because of the deposition of bile pigments.
- It appears when the serum bilirubin level is above 2 mg/dl.
- Bilirubin is a yellow pigment, and it is biotransformed in the liver and then excreted in the bile, urine, and stool.
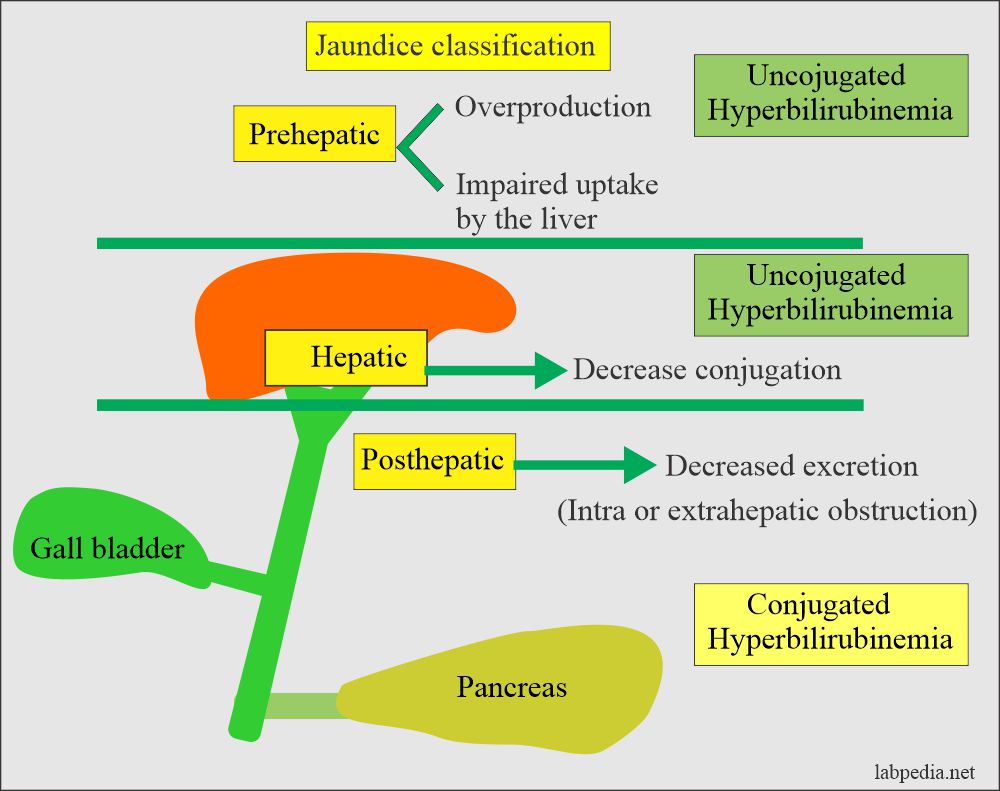
Jaundice may be classified as:
On the basis of etiology:
- Pre-hepatic.
- Hepatic.
- Posthepatic.
Physiological classification:
- Unconjugated hyperbilirubinemia (indirect bilirubin).
- Conjugated hyperbilirubinemia (indirect bilirubin).
Unconjugated hyperbilirubinemia:
Causes of unconjugated hyperbilirubinemia:
- Increased production:
- Hemolysis (hemolytic disease of the newborn).
- Hereditary.
- Acquired.
- Ineffective erythropoiesis.
- Increased turnover, like in neonates.
- Physiologic jaundice of the newborn.
- Decreased delivery:
- Congestive heart failure.
- Portacaval shunt.
- Decreased uptake by the hepatocytes:
- Drugs.
- Gilbert’s syndrome.
- Sepsis.
- Fasting.
- Decreased storage of unconjugated bilirubin:
- Fever.
- Competitive inhibition.
- Decreased conjugation:
- Physiologic jaundice, e.g., Neonatal jaundice.
- Drugs.
- Hereditary like Crigler-Najjar syndrome.
- Complete enzyme deficiency, Type 1
- Partial enzyme deficiency, Type 2
- Hepatocellular dysfunction.
- Gilbert’s syndrome.
Conjugated Hyperbilirubinemia:
- Decreased secretion into bile canaliculi:
- Hepatitis.
- Cholestasis (Intrahepatic).
- Dubin – Johnson syndrome.
- Rotor syndrome.
- Decreased drainage or excretion.
- Extrahepatic obstruction:
- Stones.
- Carcinoma.
- Stricture.
- Atresia.
- Sclerosing cholangitis.
- Intrahepatic obstruction:
- Drugs.
- Primary biliary cirrhosis.
- Tumors.
- Granulomas.
- Idiopathic neonatal hepatitis (cholestatic jaundice).
- Extrahepatic obstruction:
Features and characteristics of the various type of jaundice:
| Tests | Pre Hepatic | Hepatic | Post-hepatic |
|---|---|---|---|
| Bilirubin Total | Raised | Raised | Raised |
| Bilirubin Conj. | Raised | Raised | raised |
| SGPT | Normal | Raised markedly ++++ | Normal or slightly raised |
| SGOT | Normal | Raised markedly ++++ | Normal or slightly raised |
| Alk.Phosphatase | Normal | Slightly raised + | Markedly raised ++++ |
- The following table differentiates between Pre Hepatic, Hepatic, and Post Hepatic Jaundice.
Causes of Jaundice:
| Type of Jaundice | Causes |
|---|---|
| Pre hepatic | Hemolysis |
| Hemolytic disease of the newborn | |
| Hepatocellular | viral hepatitis |
| Alcohol | |
| Advanced chronic liver disease | |
| Gilbert’s syndrome | |
| Post-hepatic (Obstructive) | common bile duct gallstones |
| pancreatic tumor | |
| Ca of the extrahepatic duct |
Hepatorenal failure:
- There is progressive renal failure in patients with severe end-stage liver disease (acute liver failure).
- There is no obvious cause of renal disease.
- The renal biopsy is essentially normal.
Questions and answers:
Question 1: What is the value of GGT?
Question 2: What is the role of bacteria on bilirubin in the intestine?