Leishmaniasis, Cutaneous and visceral leishmaniasis (Oriental Sore and Kala-azar)
Leishmaniasis
Sample for Leishmaniasis
- Prepare a smear from the lesion of the patient.
- Spleen, tissue or aspirate, and (FNA) of lymph nodes.
- Splenic puncture.
- Nasal smears.
- Bone marrow aspirate.
- Culture from the above samples.
- Buffy coat of peripheral blood.
Indications for Leishmaniasis
- This helps in the diagnosis of Cutaneous Leishmaniasis or oriental sore.
- For diagnosis of visceral leishmaniasis.
Definition of Leishmaniasis
- A protozoan of the genus leishmania causes leishmaniasis.
- Leishmania includes many species, which may cause more than one clinical syndrome.
- Leishmania causes three syndromes:
- Visceral leishmaniasis is called Kala-Azar.
- Cutaneous leishmaniasis is localized or widespread.
- Mucosal leishmaniasis.
Pathophysiology of Leishmaniasis
- Leishmaniasis is caused by a protozoan of the genus Leishmania, which causes many syndromes.
- The sandfly transmits cutaneous Leishmania (CL).
- Genus of protozoa comprising parasites of worldwide distribution.
- It is best known in the Middle East and occurs in the Far East. It is not seen in Japan.
- It is seen in various areas of Africa, Central, and South America, the Island of the Caribbean, and occasionally the European side of the Mediterranean area.
- Several species of which are pathogenic to humans. All species are morphologically indistinguishable.
- These are divided into the Clinical syndrome they produce:
- Visceral (Kala-Azar).
- This is a chronic systemic disease associated with the following:
- Leishmania donovani.
- Leishmania infantum.
- Leishmania chagasi.
- This is a chronic systemic disease associated with the following:
- Cutaneous (Localized or widespread).
- Mucocutaneous.
- Visceral (Kala-Azar).
- Leishmania is classified into :
- L. donovani.
- L. tropica.
- L. Mexicana.
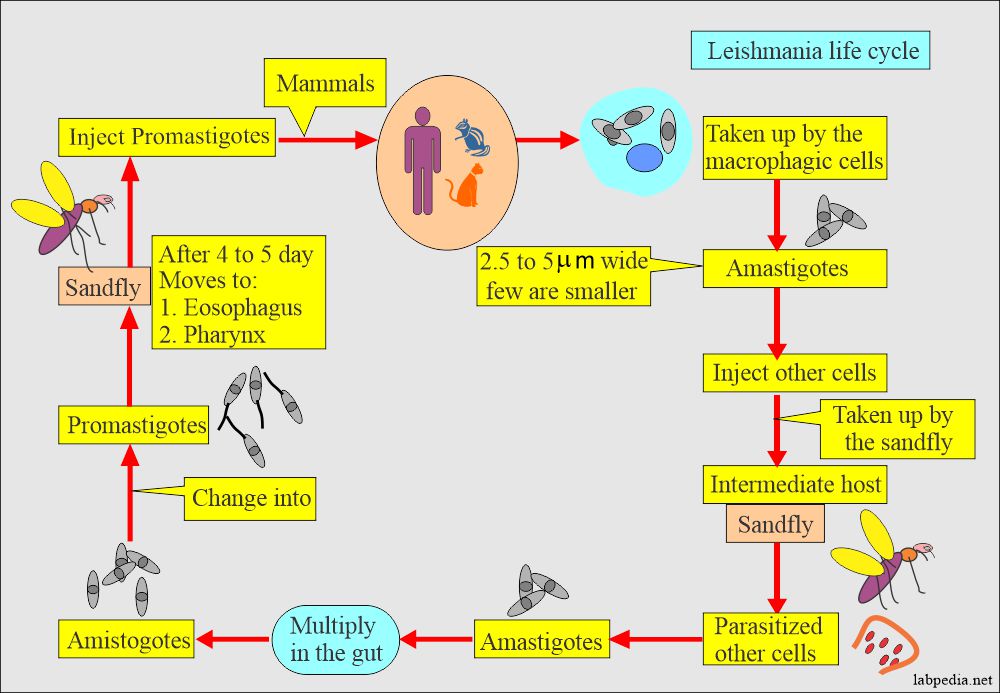
Summary of the Leishmania life cycle:
- Leishmania is zoonotic and carried by rodents, dogs, and foxes transmitted to humans by biting sandflies (Phlebotomus).
- Promastigote invades phagocytic cells (macrophages) from the sandfly bite and transforms into nonmotile amastigotes.
- Amastigotes multiply in the macrophagic cells of lympho nodes, spleen, liver, and bone marrow.
Cutaneous leishmaniasis
- Cutaneous leishmaniasis is divided into Old-world and New-world types.
- Leishmania tropica:
- L. Tropica complex consists of the following:
- L. tropica.
- L. major.
- L. aethiopica.
- This complex causes Oriental sore, also called Baghdadi boil, old world cutaneous leishmaniasis, or Delhi ulcer.
- This is transmitted by sandflies belonging to the genus Phlebotomus.
- L. Tropica complex consists of the following:
- Epidemiology:
- These lesions are seen in the Mediterranean littoral, Armenia, Azerbaijan, Uzbekistan, Turkmenistan, Afghanistan, India, Pakistan, and Iran.
- The dog may be the natural host, but it does not look like an effective reservoir for a human.
- Incubation time is 2 months to 3 years.
- Cutaneous leishmaniasis generally causes skin lesions, persisting for months, sometimes years.
- The skin lesions usually develop within several weeks or months after exposure.
- These lesions are usually on the face.
- The lesions typically evolve from dry papules to nodular plaques to ulcerative lesions.
- These ulcers are usually 2 cm in Diameter or more with typical itching.
- These lesion has raised border and central depression, which can be covered by scab or crust.
- Rarely do some lesions persist as nodules.
- These lesions are painless but sometimes may give rise to pain when infected.
- The healing process typically results in atrophic scarring.
- Leishmania Major:
- It produces an acute infection with a duration of 3 to 6 months.
- The lesion primarily occurs on the lower limbs.
- These lesions are moist and tend to ulcerate very early.
- There may be secondary lesions on other sites.
- This disease is seen in Turkmenistan, Uzbekistan, Iran, Kazakhstan, Syria, Israel, Jordan, Africa, Algeria, Sahara, Tunisia, Sudden, Nigeria, Niger, Mali, Senegal, and Kenya.
- Leishmania Mexicana:
- This causes new world cutaneous leishmaniasis
- It causes a Chiclero ulcer or Bay sore.
- It is found in Belize, the Yucatan peninsula, and Guatemala.
- It is endemic in these areas.
- The amastigotes are found in the skin lesion of humans, woodrats, and cats.
- Lesions are usually single, and 40% involve ears.
- This may give rise to the diffuse cutaneous lesion.
- Signs and symptoms:
- The first sign of the infection is a red papule.
- There is itching, which may grow to 2 cm or more in diameter.
- In L. major infection, the papule is covered with serous exudate and ulcerates early.
- In L. tropical, papules are dry and ulcerate only after several months.
- This cutaneous form may be seen as:
- Diffuse cutaneous leishmaniasis may be due to lake cell-mediated immunity.
- Leishmaniasis recideva is due to good antibody and cellular response. In this case, the central lesion heals, and the peripheral area is active.
- Diagnosis of cutaneous leishmania:
- Organisms are diagnosed by direct smear and microscopy.
- Culture will be positive from the lesion.
Mucocutaneous Leishmaniasis:
- It is the least common syndrome, and it occurs in Central and South America.
- It follows after the cutaneous leishmania.
- L. braziliensis causes mucocutaneous leishmaniasis, also called espundia and uta.
- There is the formation of an ulcer on the oral-nasal mucosa.
- This is common in Brazil.
- The cutaneous lesions are multiple and large in size.
- Secondary infection plays a role in the persistence of the large size lesion.
- Signs and symptoms:
- Sometimes it spreads to the mucous membranes.
- The entire nasal mucosa and the hard and soft mucosa are involved.
- The nasal septum will be destroyed.
- But unlike syphilis, the bone is not involved.
- The ulceration leads to the loss of all soft parts of the nose, lips, and palate.
- Death may occur in these patients due to secondary infection.
- A similar disease is also seen in Sudan and Ethiopia.
- Diagnosis of mucocutaneous leishmania:
- Organisms are identified by histologic examination in scrapings or biopsy from the lesion.
- Culture can be done and are positive in 50% of the cases.
- Positive immunofluorescent antibody test.
- PCR gene amplification for Leishmania DNA or culture.
Visceral leishmaniasis (Kala-Azar)
Leishmania donovani:
- Three types of Leishmania Donovani complex cause it:
- L. Donovani donovani.
- L. Donovoni chagasi.
- L. Donovani infantum.
- It causes visceral leishmaniasis, called Kala-azar or black disease, Dumdum fever.
- This occurs in India, Burma, Bangladesh, Thailand, and Sumatra.
- Also seen in the Central African Republic, Sudan, Kenya, Gambia, Gabon, Northern Uganda, and Niger.
- This was seen in China, but now it is controlled.
- Vector is Phlebotomus sandflies.
- In some cases, L.tropica has been found, in a few cases in India and veterans from the Gulf war.
- The causative agent is a parasite of the reticuloendothelial system.
- This is not confined to the reticuloendothelial cells of the subcutaneous tissue and mucous membranes but may be found throughout the body.
- Signs and symptoms of Kala-azar:
- The Visceral leishmaniasis (also known as Kala-Azar).
- No skin lesions are seen, rarely except a papule at the site of the bite.
- Fever.
- Weight loss (cachexia, wasting).
- Hepatosplenomegaly (usually, the spleen is more prominent than the liver).
- It returns to normal after the treatment.
- Bone marrow, when involved, give rise to:
- Pancytopenia, i.e., anemia (normocytic and normochromic), leukopenia, and sometimes thrombocytopenia.
- TLC is usually below 4000/cmm and is between 2000 to 3000/cmm.
- There is a monocytosis.
- High total protein level and a low albumin level, with hypergammaglobulinemia.
- Lymphadenopathy may be noted in some geographic regions, such as Sudan.
- HIV-coinfected patients may have atypical manifestations, such as gastrointestinal and other organ systems involvement.
- Kala-azar means black (kala) fever (Azar). These are severe (advanced) cases of visceral leishmaniasis.
- Kala-azar or severe visceral leishmaniasis untreated is typically fatal due to:
- Directly from the disease.
- Indirectly from complications, such as hemorrhage or secondary bacterial infection.
- If untreated, the mortality rate may reach 100% within two years (WHO).
- Kala-azar or severe visceral leishmaniasis untreated is typically fatal due to:
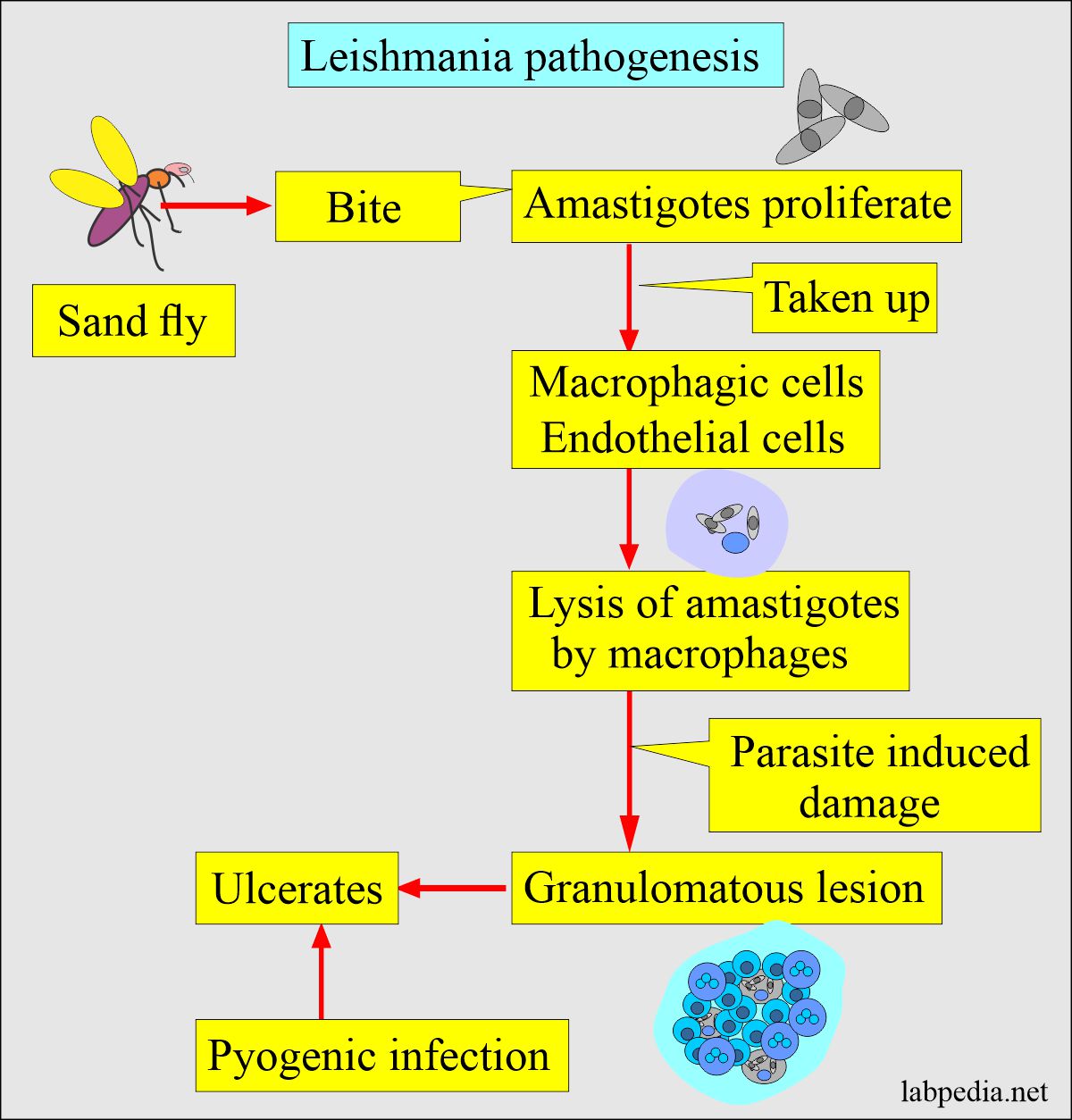
- Pathogenesis of the lesion:
- The fly, when biting the host, then amastigotes proliferate.
- These are taken up by the macrophages and the endothelium of the small capillaries.
- Macrophagic cells cause the lysis of amastigotes.
- The organism infects the mononuclear cells of the reticuloendothelial system.
- The incubation period varies from 2 weeks to more than 2 years and is mostly 3 to 8 months.
- A chronic granulomatous reaction leads to local nodule formation due to parasite-induced damage.
- This may ulcerate, and there is the possibility of pyogenic infection.
Mode of the spread of Leishmania:
1. Leishmania spreads through the bite of the female sandfly (Phlebotomus).
2. Human is a natural source of a reservoir. Other reservoirs are dogs, wild canines, rodents, and humans.
Laboratory Diagnosis of Leishmaniasis:
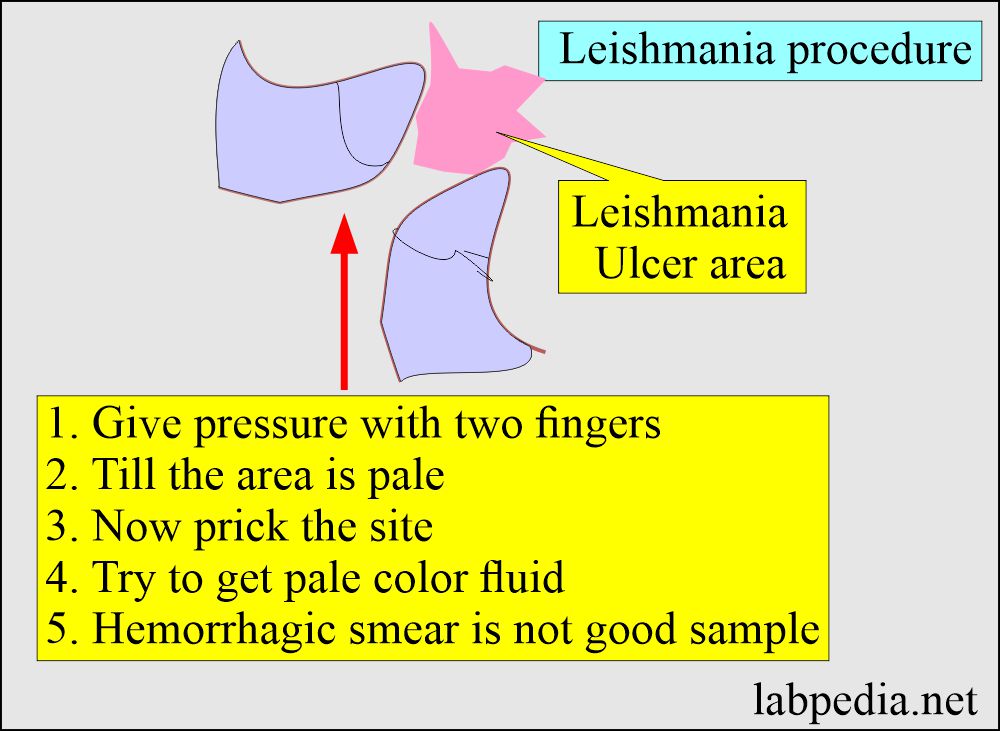
Procedure how to make smear for cutaneous leishmaniasis:
- If the ulcer is on the arm or feet, then first try to put pressure to stop the blood supply to that area.
- Now prick and try to get yellow color material or serum-like material.
- Make a smear from this material.
- Another method is to take a sample like Fine needle aspiration (Author’s personal experience ).
- The FNA method is done at the periphery of the ulcer and gets a good sample most of the time.
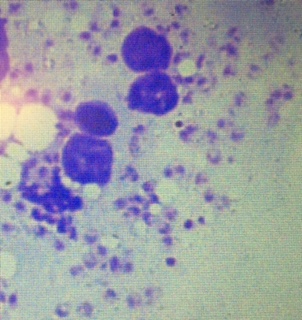
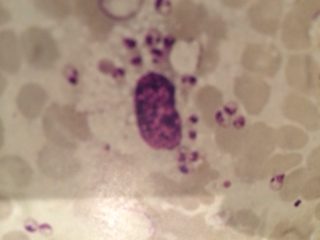
Result of cutaneous smears:
- In a good smear, you will see a lot of LT bodies in the histiocytes and outside on the smear.
- Also, can find a single separate LT body
Find amastigotes from the various areas:
- L. tropica is diagnosed by making the smear from the deeper area of the skin lesion.
- These smears are stained with Giemsa (or Wright’s) stains. Typical amastigotes are seen.
- Material aspirated from the bone marrow (64% to 86% positive), spleen (95 to 98% positive), or enlarged lymph nodes (roughly 64% positive).
- Make a smear from the nasal secretion in case of a mucocutaneous lesion.
- From the buffy coat of peripheral blood (67% to 99% positive).
- The culture of aspirates or peripheral blood.
- Can find the Leishmania antibody using the known parasitic antigen.
- Leishmania amastigotes (LT body) are seen in the monocytes, and a few are seen as single in the smear.
- Serological tests:
- Serological tests are in the form of ELIZA, IFA, CIE, direct agglutination, and IHA.
- ELIZA and indirect fluorescent antibody assay.
- PCR of the tissue or WBC buffy coat has been used in NIH.
- There is a marked increase in serum globulin (IgG) with decreased albumin and reversed A/G ratio.
- Culture: Incubate at 26°C from the lesion, which will take up to 4 weeks.
- Hematological tests:
- ESR is raised due to increased serum globulin.
- There is anemia and leucopenia.
- There is thrombocytopenia due to hypersplenism and decreased bone marrow proliferation.
- There may be proteinuria and hematuria.
- In chronic cases may see amyloidosis.
Treatment of Leishmaniasis:
- The best drug is Sodium stibogluconate (antimony sodium gluconate (Pentostam).
- Pentostam 20 mg/Kg body weight is injected I/V or I/M for 20 days for cutaneous leishmaniasis.
- This dose can be repeated in the resistant cases at 10 days intervals.
- A maximum of three courses can be given.
- Pentostam 20 mg/Kg body weight is injected I/V or I/M for 20 days for cutaneous leishmaniasis.
- Another drug is:
- Meglumine antimonate (Glucantime).
- Initial 50 mg/Kg body weight given for 10 to 12 days for cutaneous leishmaniasis.
- For mucocutaneous, give treatment for 15 days and repeat after 15 to 20 days if healing is not complete.
- Pentamidine.
- Oral Ketoconazole 400 mg daily for 4 to 8 weeks effectively treating longstanding cutaneous leishmaniasis.
- Steroids
- Meglumine antimonate (Glucantime).
Question 1: What is the best way to get a good smear from the skin.
Question 2: What is Kala-Azar.


very nice ………
Thanks. Please see the link.
https://labpedia.net/leishmaniasis-cutaneous-and-visceral/