Hepatitis B Virus (HBV)
What sample is needed for the Hepatitis B Virus (HBV)?
- The best sample for the viral hepatitis B markers or profile is serum.
- A random sample can be taken. No need for a fasting sample.
What are the Indications for Hepatitis B Virus (HBV)?
- Viral hepatitis B marker is done for:
- The diagnosis of HBV infection.
- The diagnosis of the carrier.
- The diagnosis of chronic hepatitis.
- Screening of blood for transfusion.
How will you define the Hepatitis B Virus (HBV)?
- HBV is also called serum hepatitis or long incubation hepatitis.
- This DNA virus causes viral hepatitis B.
- This is a double-stranded DNA virus, and one strand is incomplete.
How will you discuss the biology of the Hepatitis B Virus (HBV)?
- This virus belongs to the Hepadnaviridae family.
- HBV is found in the blood and body secretions.
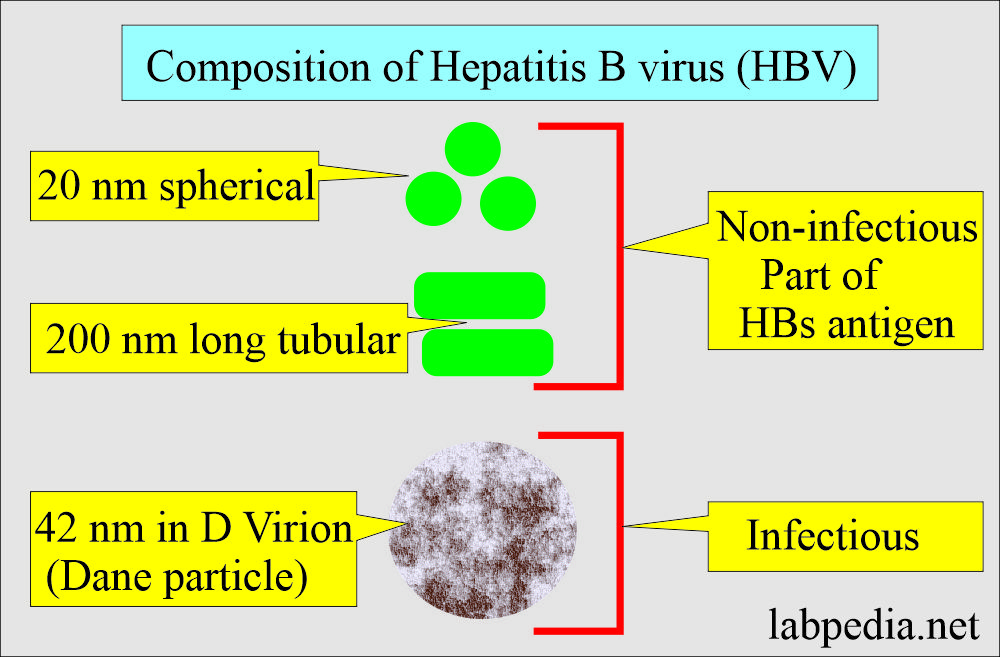
- In the HBs antigen-positive serum, there are three types of particles:
- The most common are spherical, 20 nm in diameter.
- The second particle is 200 nm long and 20 nm in width.
- Dane particles, also called virions, 42 nm spherical, are few in the blood.
- HBsAg particles (sphericle and tubular) are not infectious. While Dane particle is infectious.
How will you describe the Summary of the features of the Hepatitis B virus (HBV)?
| Parameters | HBV features |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
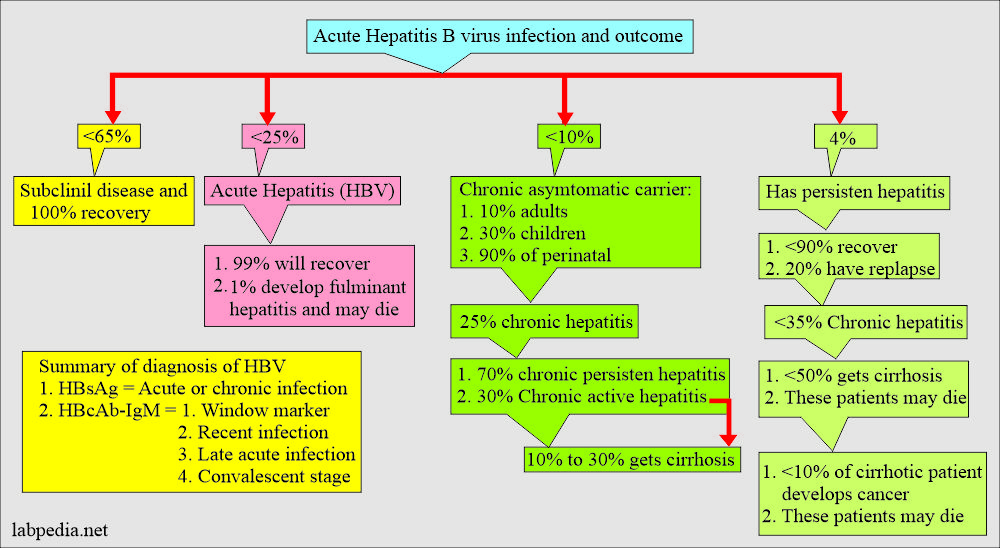
What is the outcome of the Hepatitis B Virus (HBV) disease?
- Acute hepatitis.
- Chronic hepatitis.
- Cirrhosis.
- Liver cell carcinoma.
- This is usually seen in young adults.
How will the Hepatitis B virus (HBV) be transmitted?
- Blood and blood products.
- Contaminated needles can spread it.
- In I/V, drug abusers are seen in about 25% to 30% every year in the USA.
- It is also seen in renal dialysis patients.
- It can spread through sexual contact through the rectum or by sexual intercourse.
- It is quite common in male homosexuals.
- It is less common in heterosexuals.
- It can spread through bodily fluids like infected blood, saliva, and semen through a small skin or mucous membrane break.
- There is an increased risk in renal transplantation patients and patients with leukemia and lymphoma.
- There is transplacental spread.
- Hospital workers are also at risk, roughly 5% of yearly cases in the USA.
- This usually happens by accidental needle prick.
- It is also common among dentists and dental workers.
What are the high-risk groups in Hepatitis B Virus (HBV) infection?
- Multiple Blood transfusion recipients.
- Male homosexuals.
- Dialysis patients.
- Transplant patient.
- I/V drug user.
- Hospital worker because of needle pricks.
- Patient with leukemia and lymphoma.
- During delivery, it can infect the newborn if the mother is a carrier.
- A family member with close contact.
What is the incubation period of the Hepatitis B Virus (HBV)?
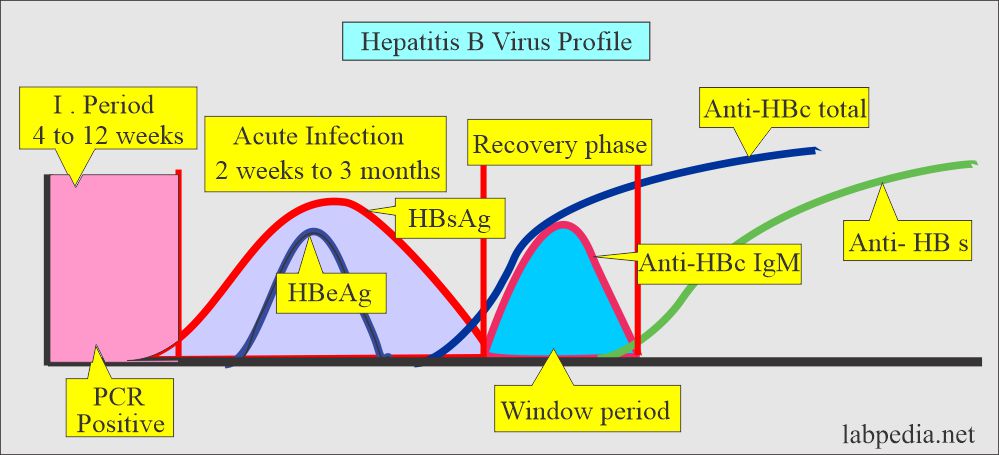
- This incubation lasts from 5 weeks to 6 months (60 to 90 days).
- This virus can cause acute infection and may develop into a chronic disease.
What is the structure of the Hepatitis B Virus (HBV)?
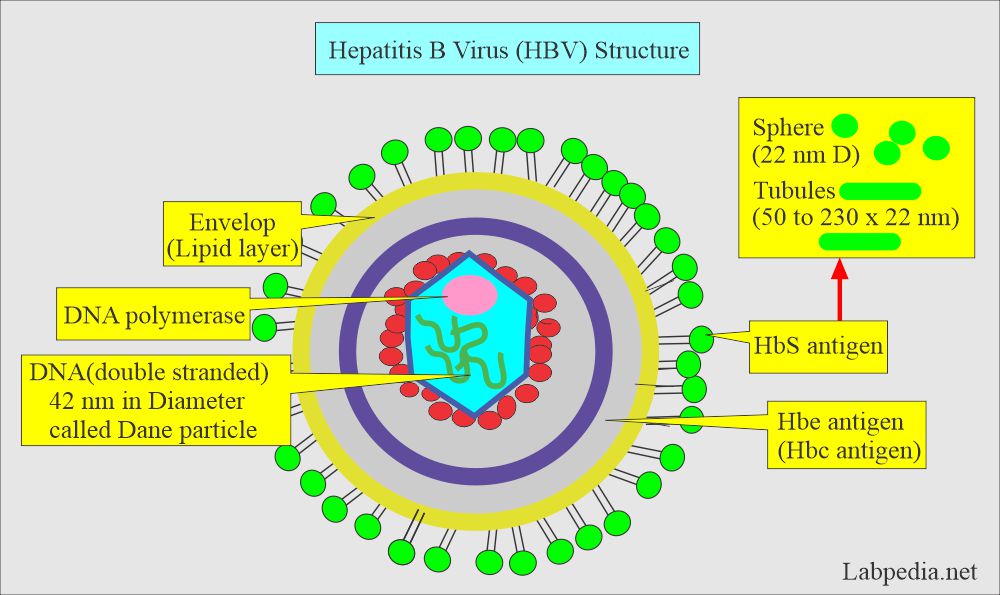
- This is a DNA virus called a Dane particle (Virion).
- It has an inner core surrounded by an outer capsule.
- The outer capsule contains the hepatitis B surface antigen (HBs-Antigen). This is also called the Australian antigen (HBsAg).
- The inner core contains HBV core antigens. One is called HBcAg, and another antigen incorporated into the core antigen is HBeAg.
- The HBcAg is in a very small amount, so it is not detectable, but its Antibody is found in circulation.
What are the Hepatitis B Virus (HBV) antigens and antibodies?
- Dane particle (Virion) has a double-shell structure containing several antigens (antigenic material).
- The outer envelope is called a surface antigen (HBsAg), the Australian antigen.
- The inner core contains HBV-core antigen (HBcAg), and HBV-e antigen (HBeAg).
- Within the core is double-stranded DNA (double-stranded viral deoxyribonucleic acid).
- There is an enzyme called DNA polymerase.
- There are three antigens:
- HBsAg
- HBcAg
- HBeAg
- There are three Antibodies:
- Anti-HBsAb
- Anti-HBcAb
- Anti-HBeAb
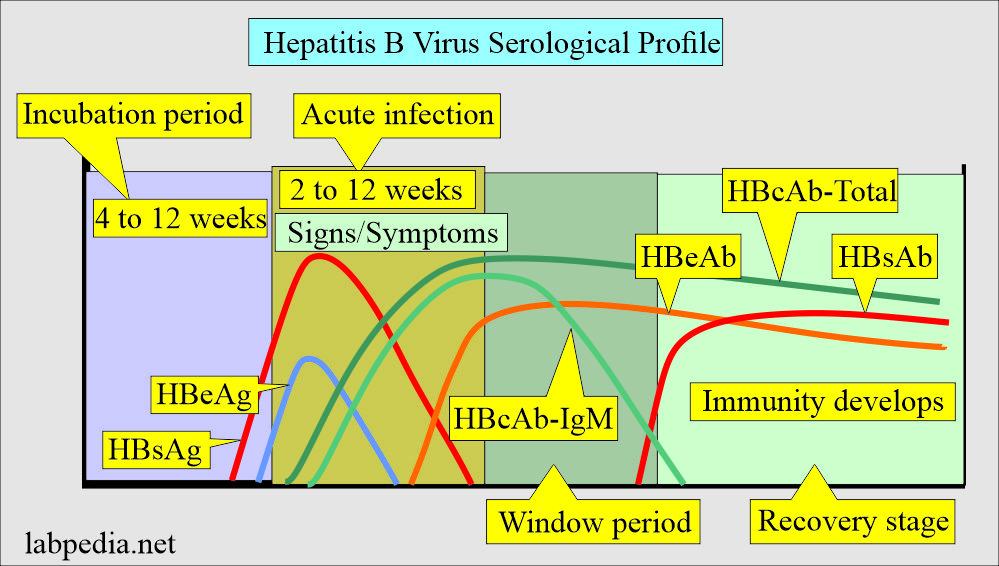
How will you discuss Hepatitis B surface antigen (HBsAg)?
- An immunoassay or nucleic acid probe detects HBV surface antigen (HBsAg).
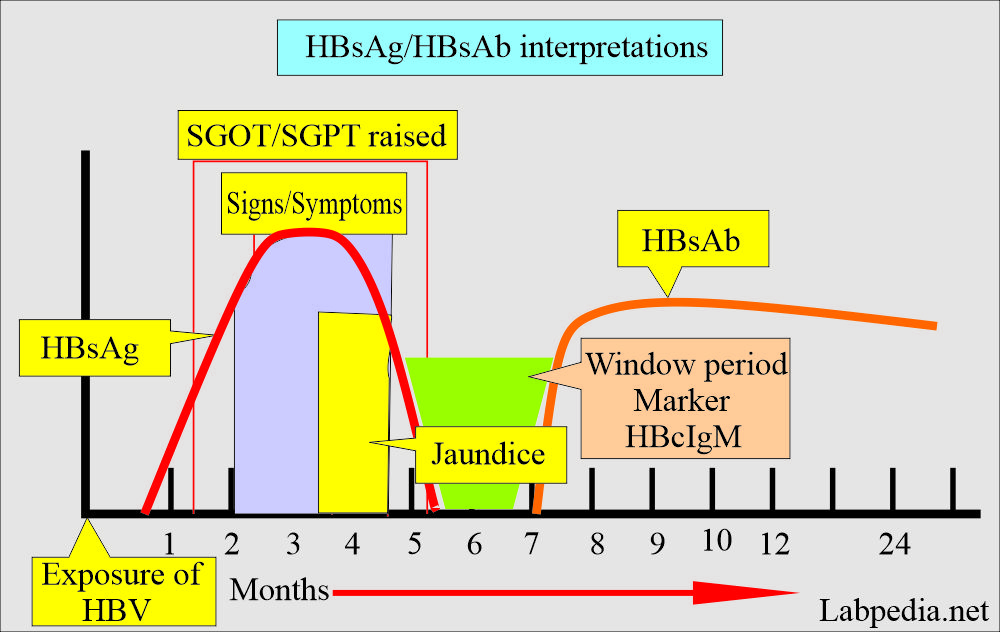
- HBsAg appears first in the blood, so its detection in the blood is a very common test.
- HBsAg rises before clinical signs and symptoms appear and are detectable.
- The peak is during the first week of symptoms.
- It returns to a normal level by the time jaundice subsides.
- If it persists, the patient will be a carrier or develop chronic hepatitis.
How will you interpret HBsAg?
| Parameters | Clinical presentation |
|
|
|
|
|
|
How will you describe Hepatitis B surface antibody (HBsAb)?
- This antibody appears after roughly 4 weeks after the disappearance of HBsAg.
- It indicates the end of the acute phase and the patient’s complete recovery from the infection.
- The patient will develop immunity to HBV infection.
- After vaccination, HBsAb appears.
How will you interpret HBsAb?
| Parameters | Clinical interpretations |
|
|
|
|
|
|
How will you discuss Hepatitis Core antigen (HBcAg)?
- This is not detectable because of the very small quantity, and it is incorporated with HBeAg.
- There are no commercial kits available to detect HBcAg.
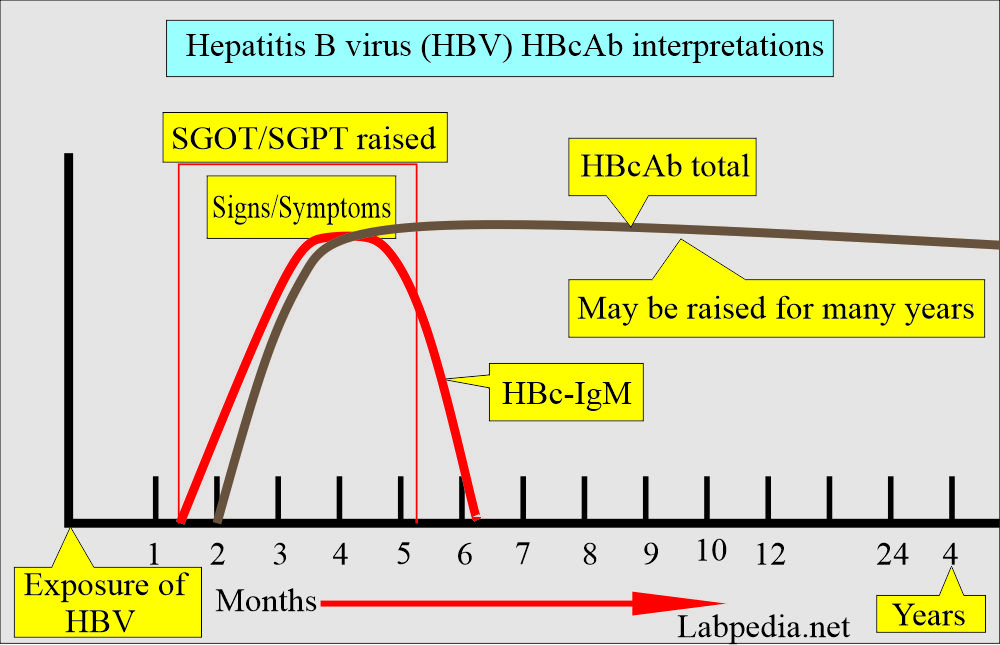
How will you describe Hepatitis B Core Antibody (HBcAb)?
- There are kits available for HBc-IgM and total HBcAb (HBc-IgM and IgG)
- This antibody appears after one month of infection.
- This will be HBcAb-IgM type in acute infection and later replaced by HBcAb-IgG type.
- HBc-IgM is detected in active acute or recent acute HBV infection.
- HBc-IgM rises during active acute infection of HBV and will remain in the convalescent stage.
- It will be seen when HBsAg disappears, and HBsAb appears (window period).
- It is also called a “core window” marker.
- This antibody persists in circulation for several years.
- This antibody will be present in chronic hepatitis cases.
- In the window period, when HBsAg is negative, and there is still no HBsAb, then HBc-antibody is present in the patient.
- It is not detected in the early weeks or months of the recovery phase.
- HBcAb total has been elevated for many years and gives positive results in the:
- Late-stage active acute infection.
- Convalescent stage.
- Chronic stage (chronic infections).
- Recovery early stage.
- HBcAb total may be found with HBsAg.
How will you interpret HBcAb?
| Parameters | HBcIgM | HBcAb total |
|
|
|
|
|
|
|
|
|
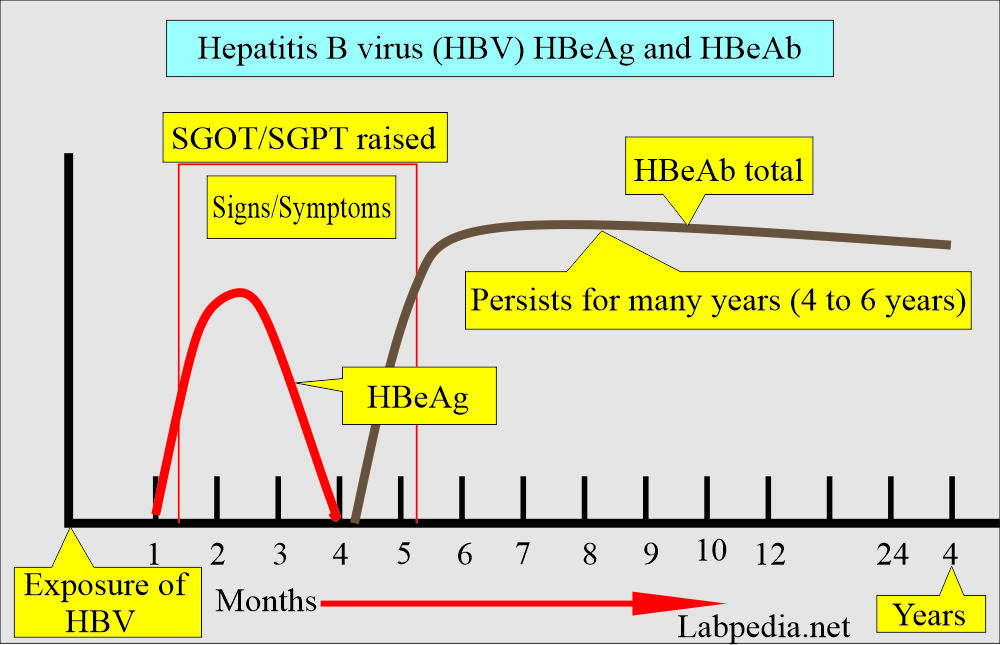
How will you discuss Hepatitis Be antigen (HBeAg)?
- HBeAg is not usually advised when diagnosing HBV infection.
- HBeAg is a marker of infectivity and continued replication of the HBV infection.
- HBeAg without the appearance of the HBeAb will indicate greater potential for spreading the infection to other people.
- HBeAg disappeared shortly before the HBsAg disappeared.
- HBeAg appears immediately after the appearance of HBsAg.
- HBeAg indicates early and acute disease.
- HBeAg positive in chronic hepatitis patients is a sign of a bad prognosis.
- The persistence of HBeAg indicates the development of chronic hepatitis.
How will you interpret HBeAg?
| Parameters | HBeAg |
|
|
|
|
|
|
How will you discuss the hepatitis Be antibody (HBeAb)?
- The appearance of HBeAb is a sign of recovery.
- HBeAb appears after the HBeAg’s disappearance or 1 to 2 weeks later.
- HBeAb appearance indicates that HBV infection is over and infectivity for other people is less common.
- This antibody shows the end of the acute phase.
- The presence of HBeAb indicates less infectivity.
How will you summarize HBeAb interpretations?
| Parameters | HBeAb |
|
|
|
|
|
|
How will you describe Clinical presentations of the Hepatitis B Virus?
- There is variation in the symptoms from mild to severe.
- It is fatal in about 1% to 3% of patients.
- 30% to 40% of patients develop acute hepatitis.
- Most of the children and 50% of the adults are asymptomatic.
- Infants are almost always asymptomatic, and most children do not develop jaundice.
- The symptoms are insidious.
- The prodromal period often shows :
- Fever.
- Malaise.
- Myalgia.
- The patient may have nausea and vomiting.
- There is weight loss.
- The acute period with jaundice lasts about one month.
- The patient will have jaundice and dark-colored urine.
- <1.5% may develop fulminant hepatitis.
- Chronicity decreases with age.
- 85% are seen in neonates.
- 25 to 50% of children.
- 6 to 10% of adults.
- These patients are at high risk for liver cell carcinoma.
- Pregnant ladies may get an infection during 3rd trimester or early postpartum or HBV carrier, frequently transmitting HBV infection to their babies after birth.
- When a mother is HBsAg and HBeAg positive, it will transmit the infection to babies from 12.5% to 40%, which may be as high as 70% to 90%.
- In one of the studies, when PCR is negative but routine HBsAg and HBeAg are positive, fewer infants get infected.
- Without treatment, 80% to 90% of babies become chronic carriers of HBsAg. These babies are prone to develop a risk of fatal cirrhosis or liver cell carcinoma.
- If newborns are given vaccines and immunoglobulin, the risk of chronic carrier state will be reduced.
How will you differentiate HAV and HBV?
| Presentation | HBV | HAV |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
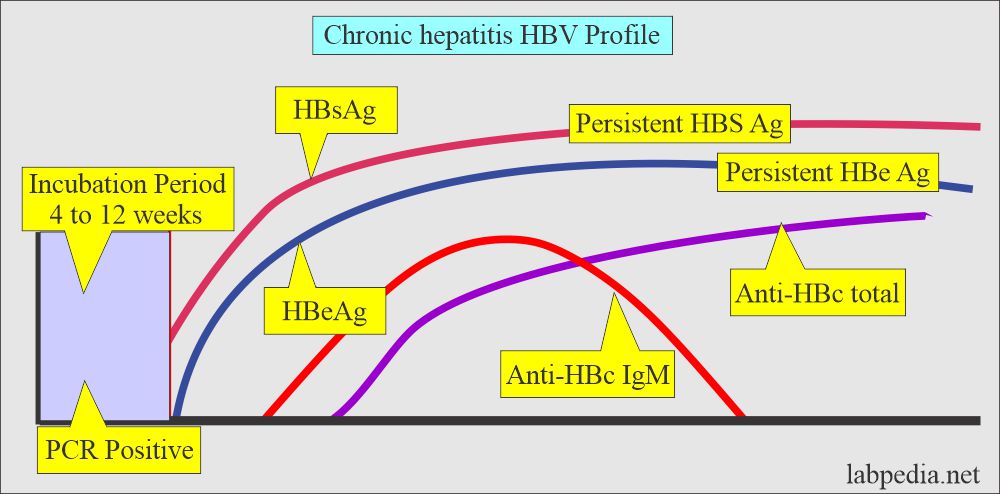
How will you discuss Chronic viral hepatitis due to HBV or (Chronic carrier)?
- Chronic hepatitis is defined when >6 months surface antigen (HBsAg) is present with normal liver function tests and normal microscopic findings on the liver biopsy.
- 2 to 10 % develop chronic disease.
- Chronic hepatitis is divided into:
- Chronic persistent hepatitis where abnormal liver function tests, relatively normal microscopic findings on liver biopsy. This condition is seen in 6% of the patients.
- Chronic active hepatitis where abnormal liver function tests and abnormal microscopic findings on liver biopsy. This condition may be seen in 3% of the patients.
- These patients may develop cirrhosis.
- Cirrhotic patients have more chances of cancer, which almost increased 500 times.
- Lab findings are:
- HBsAg positive.
- HbcAb-IgG (Total) is positive.
- HBeAg positive indicates a highly infective stage and poor prognosis.
What is the significance of various hepatitis B virus (HBV) markers?
Acute infection
- HBsAg positive.
- HbcAb- IgM positive.
What are the recovery stage parameters?
- HBsAg is negative.
- HBsAb is positive.
What are the markers for the Window period?
- HBsAg is negative.
- HBsAb is negative.
- HBcAb-IgM will be positive.
How will you determine HB Viral load?
- PCR qualitative for the HBV genome.
- PCR quantitative by HBV DNA by RNA probe.
How will you interpret HBV antigens and antibodies?
| HBV Ag/AB | Appears | Disappears | Significance |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you interpret various stages of HBV infection?
| Test | Acute | Chronic | Recovery | Carrier | Window period | Vaccination |
|---|---|---|---|---|---|---|
| HBsAg | positive | positive | negative/positive | positive | negative | negative |
| Anti-IgM HBc | positive | neg/pos | negative | negative | positive | negative |
| Anti-IgG HBc | negative | positive | positive | positive | neg/pos | positive |
| HBeAg | positive | neg/pos | negative | negative | negative | negative |
| Anti-HBeAb | negative | positive | positive | positive | pos/neg | negative |
| Anti-HBs Ab | negative | negative | positive | negative | negative | positive |
| PCR | positive | positive | negative | negative | positive | negative |
How will you summarize the serological profile of HBV infection?
| Serological profile | Clinical presentation |
|
|
|
|
|
|
|
|
How will you treat the Hepatitis B Virus (HBV)?
- In the case of fulminant hepatitis, liver transplantation is needed.
- Treatment of chronic HBV infection is indicated when HBV-DNA >2000 IU/L and serum SGPT is raised.
- Antiviral medications are Lamivudine (Epivir), Adefovir (Hepsera), Telbivudine (Tyzeka), and Entecavir (Baraclude).
- Interferon alpha-2 is used mainly for young patients.
How will you prevent the spread of Hepatitis B Virus (HBV) infection?
- Vaccination is the method of choice.
- This should be given at birth to infants born to carrier mothers.
Questions and answers:
Question 1: What is the best marker for the window period?
Question 2: What is the best marker for the acute hepatitis B infection?

Excellent
Thanks for the comments.
Good detailing about the HBV. Appreciable .
Thanks.