Fibrinogen (Factor 1), Acute Phase Protein
Fibrinogen (Factor 1)
Acute-phase protein (Acute Phase Reactants)
- Acute-phase protein is raised in inflammatory conditions.
- When there is an increase in a protein called positive acute-phase protein.
- In the case of a decrease in the acute phase protein, it is called the negative phase protein.
- The acute phase proteins (positive) are proteins whose concentration increases in the plasma, and after the disease episode is over, it decreases and may become normal.
Fibrinogen (Factor 1)
Sample for Fibrinogen (Factor 1)
- The patient blood is needed to prepare plasma.
- The sample is stable for 8 hours at room temperature.
- It can be stored for several months at -20 °C.
Indications for Fibrinogen (Factor 1)
- For the evaluation of bleeding disorder.
- If there is excessive bruising.
- In case of bleeding from the gums and nose.
- In the case of Bleeding in the GIT and blood in the stool.
- In the case of blood in the urine.
- If there is a rupture of the spleen.
Precautions for Fibrinogen (Factor 1)
- Avoid clot formation.
- Avoid collecting the blood from the heparinized blood vessel.
- Avoid contamination with tissue that contains tissue thromboplastin.
- Avoid contamination with heparin.
- Blood transfusion in the last month may affect the result.
- Diet rich in Omega-3 and Omega-6 fatty acids reduces the level of fibrinogen.
- Oral contraceptives and estrogen increase the level.
- Drugs like anabolic steroids, phenobarbital, streptokinase, valproic acid, and asparaginase.
Pathophysiology of Fibrinogen (Factor 1)
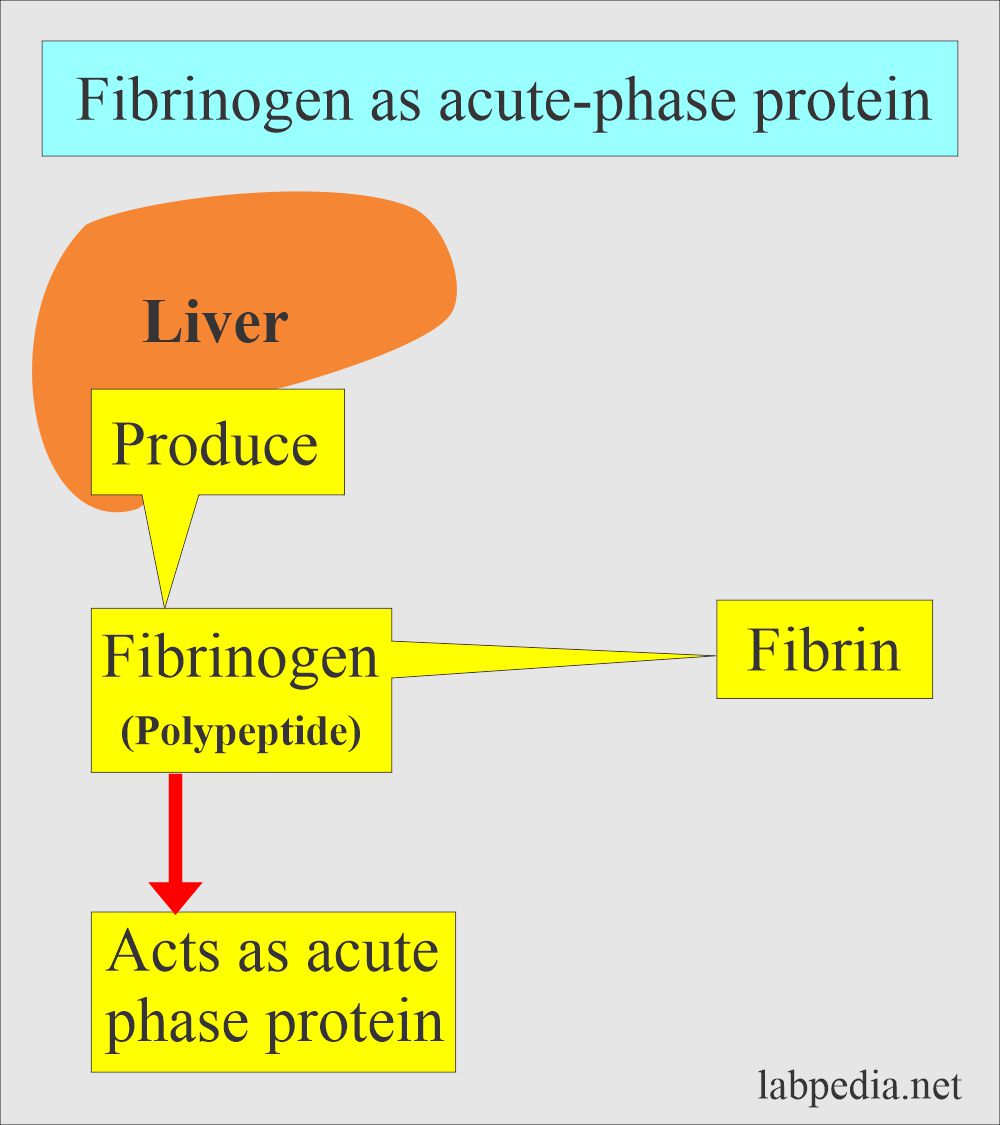
- Fibrinogen (factor 1) is an acute-phase protein.
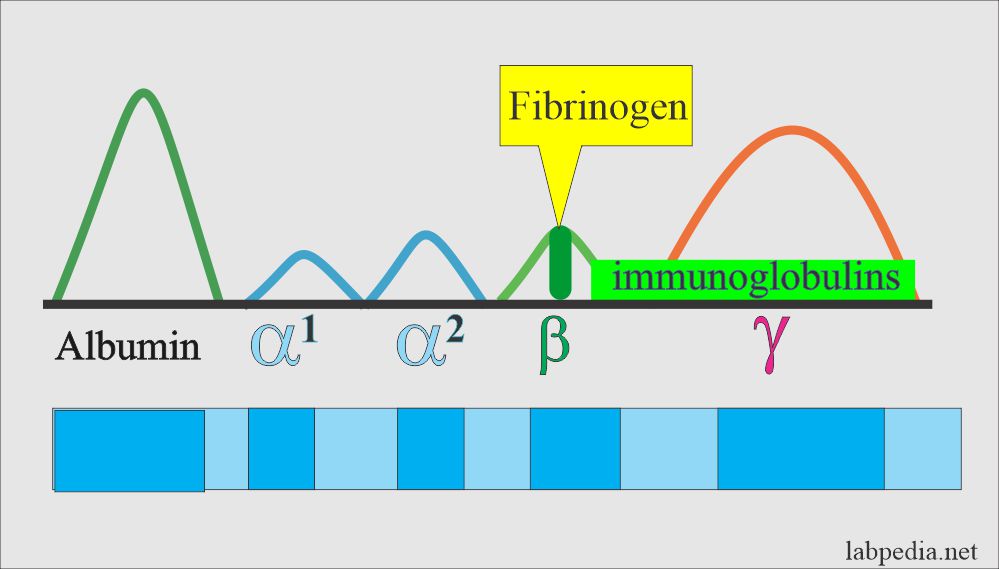
- This is β-globulin and is usually absent from the serum.
- It is a fibrillary group of glycoproteins.
- This consists of three pairs of polypeptide chains.
- It is synthesized in the liver, the major source of coagulation factors.
- Fibrinogen may act as an acute-phase protein.
When fibrinogen is transfused:
- 50% disappear in 48 hours.
- 75% disappear in 6 days.
- Half-life is 3.5 to 4 days. (Another source says 100 to 150 hours).
- This is an essential protein for blood clot formation (30% activity for normal coagulation is required).
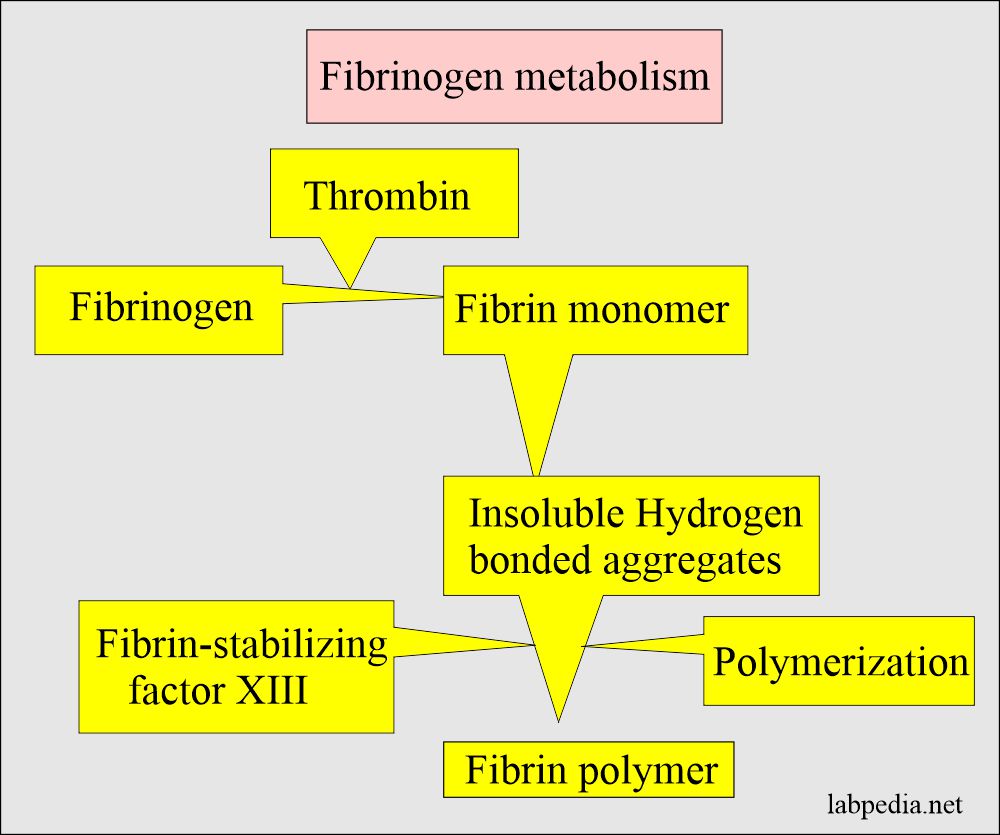
- It is a complex protein with enzymatic action that is converted into fibrin.
- In the clotting process, all the fibrinogen in the plasma is converted to fibrin.
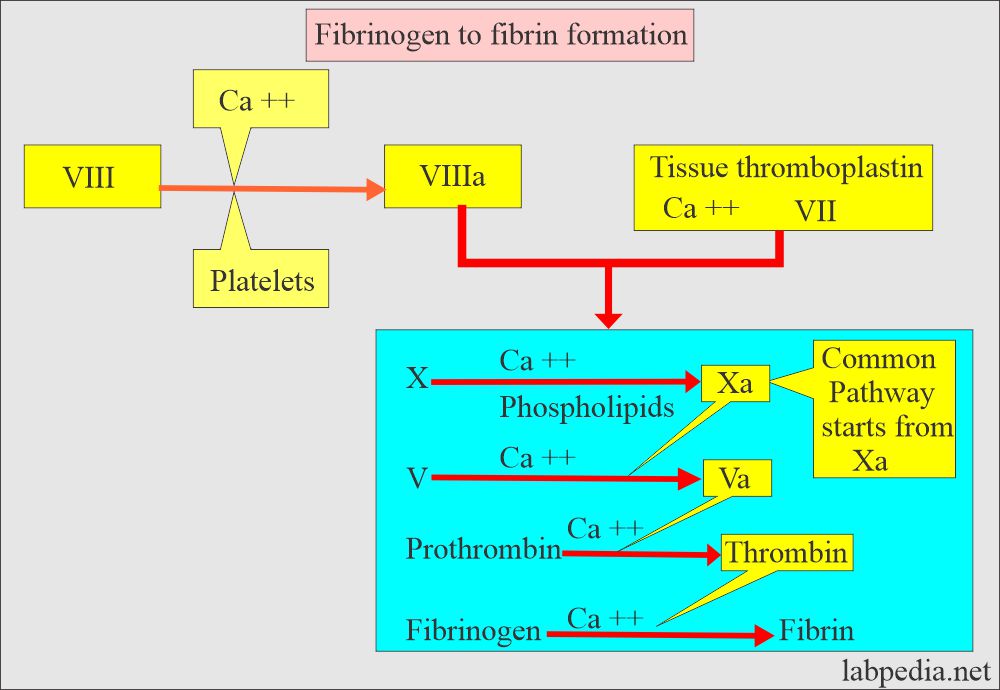
- Conversion of fibrinogen into fibrin is the final step in coagulation, and it takes place under the influence of thrombin.
- This is part of the common pathway in coagulation.
- The serum is laking fibrinogen.
Fibrinogen (Factor 1) facts:
- The fibrinogen significantly affects RBC sedimentation rates by coating the cells.
- This allows the cells to settle (sediment) faster.
- So increased fibrinogen indicate raised ESR.
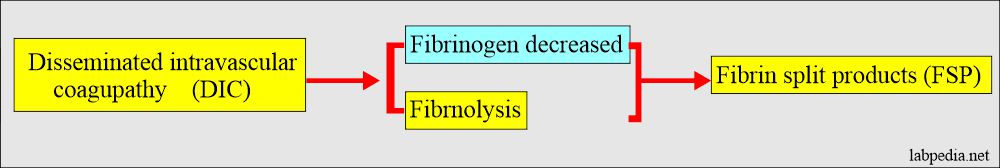
- Disseminated intravascular coagulopathy (DIC): In this case, fibrinogen is decreased.
- Fibrinogen is converted into fibrin under the influence of thrombin and is the final step in coagulation.
- This is raised by inflammation or tissue injury. Fibrinogen plays an important role in the body’s acute reaction in response to trauma or various severe diseases.
- It is a risk factor for coronary heart disease and stroke.
- Fibrinogen is decreased in the DIC.
- Fibrinogen level increases with cigarette smoking.
- There is an influence of genetics.
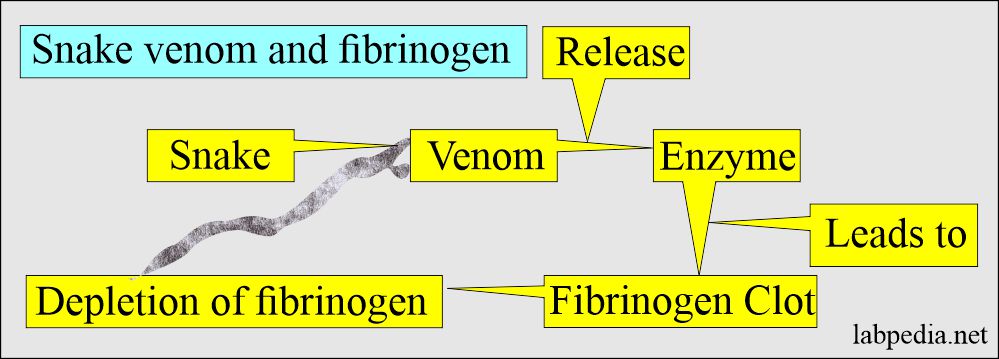
- Snake venom leads to the depletion of fibrinogen.
The normal level of Fibrinogen (Factor 1)
- Source 2
- Newborn = 125 to 300 mg/dL
- Adult = 200 to 400 mg/dL (2 to 4 g/L)
- Source 4
- 200 to 400 mg/dL (2 to 4 g/L)
- Another source
- 175 to 400 mg/dL.
The critical value of Fibrinogen (Factor 1) = <100 mg/dL.
- Another source: Critical value is <60 mg/dL.
An elevated level of Fibrinogen (Factor 1) is seen in the following:
- Acute infections.
- Myocardial infarction and Sudden cardiac death.
- Patients with malignancies.
- Inflammatory conditions like Rheumatoid arthritis and Glomerulonephritis.
- In the case of traumatic injury.
- Patient with a stroke.
- In pregnancy.
- People who are cigarette smokers.
- Patients with peripheral artery disease.
- This is raised in acute and chronic inflammation.
- Older age.
- Diabetes mellitus.
A high level of fibrinogen is associated with an increased risk of:
- Coronary heart disease.
- Myocardial infarction.
- Stroke.
- Peripheral arterial disease.
Reduced level of fibrinogen is seen in:
- Patients with severe liver diseases.
- Consumptive coagulopathy like DIC.
- Malnourished patients.
- In case of a large volume of blood transfusion.
Afibrinogenemia (Congenital):
- This is rare and usually inherited as an autosomal recessive trait (congenital absence).
- If the parents do not show the disease, they can still affect children.
- When 2 carriers of autosomal recessive positive parents have children, each child has a:
- 25% chance to be affected.
- 50% chance to be an unaffected carrier.
- 25% chance to be unaffected and not a carrier.
- There is a severe lake of fibrinogen, and blood will not clot.
- Signs and symptoms of Afibrinogenemia :
- In the case of afibrinogenemia, if the fibrinogen level is <0.1 g/L, it will have bleeding abnormality from mild to severe.
- This disease is present from birth.
- The first symptom is bleeding from the umbilical cord, which will not stop and is difficult to stop.
- There may be gastrointestinal bleeding.
- There may be nose bleeding (epistaxis) or bleeding from the oral mucosa.
- There may be bleeding episodes, bruises, and poor wound healing.
- Females may have excessive menstruation.
- There may be spontaneous abortion.
- There may be CNS hemorrhage.
- Evidence of bleeding in the joints.
- Diagnosis Afibrinogenemia:
- The following tests are advised:
- Prothrombin time (PT). It is abnormal.
- Activated partial thromboplastin time (APTT) is abnormal.
- Bleeding time (BT) is prolonged in 1/3 of the cases.
- Fibrinogen level in the blood. Plasma fibrinogen is absent.
- Reptilase time.
- Thrombin time.
- Prolonged bleeding tests time and fibrinogen level <0.1 g/L, indicating afibrinogenemia.
Congenital hypofibrinogenemia:
- It is an inherited autosomal dominant abnormality.
- Plasma fibrinogen is mildly decreased and is usually <80 mg/dL.
- Bleeding time (BT) and coagulation time (CT) are normal.
- Blood clots are small and small.
Dysfibrinogenemia:
- It is rarely inherited (autosomal dominant) or acquired heterogeneous groups of diseases.
- There is abnormal fibrinogen due to a structural abnormality which results in an abnormal function.
- This may be:
- Congenital or Inherited, there is an increased risk of bleeding, thrombosis, or both in the same patient or family.
- Some of the patients are asymptomatic.
- The prognosis is good. The event of thrombosis and bleeding is mild.
- Acquired fibrinogen is dysfunctional due to autoimmune diseases, liver diseases, plasma cell dyscrasia, or cancers.
- There is more bleeding than thrombosis.
- The prognosis is worse because of liver disease.
- Congenital or Inherited, there is an increased risk of bleeding, thrombosis, or both in the same patient or family.
Signs and symptoms of dysfibrinogenemia:
- This leads to relatively mild hemorrhage in the case of congenital cause.
- >50% of the cases have no bleeding disorders.
- 20% to 25% of cases have mild to moderate bleeding, thrombosis, or both.
- Few of these may tend to thrombosis in case of acquired cause.
- Diagnosis of dysfibrinogenemia:
- Prothrombin time (PT) is prolonged.
- Activated partial thromboplastin (APTT) is also prolonged.
- Thrombin time (TT) is the most sensitive test for dysfibrinogenemia in the case of bleeding tendency and may not be prolonged in the case of a tendency for thrombosis.
- Reptilase time is prolonged.
Value for the layman:
- This is advised when there is a history of bleeding or bruises.
- If the patient has epistaxis.
Questions and answers:
Question 1: What will happen to fibrinogen in case of snake bite?
Question 2: What is the critical value of the fibrinogen?