Fetal Hemoglobin (HbF), Alkali resistant Hemoglobin
Fetal Hemoglobin (HbF)
What Sample is needed for Fetal Hemoglobin (HbF)?
- Hemolysate is prepared from whole blood (EDTA, citrated, or heparinized).
- Avoid hemolysis.
What are the Indications for Fetal Hemoglobin (HbF)?
- Fetal Hb is done to rule out Thalassemia.
- Fetal Hb may be done on pregnant women to evaluate the fetal-maternal hemorrhage.
- HbF may be done in hemolytic anemia, hereditary persistence of fetal hemoglobin, and other hemoglobinopathies.
Discuss the Hemoglobin formation process?
- Normal Hemoglobin synthesis is dependent on three processes.
- There is a need for an adequate iron supply.
- Adequate synthesis of protoporphyrins, which is the precursor for heme.
- Adequate synthesis of globins.
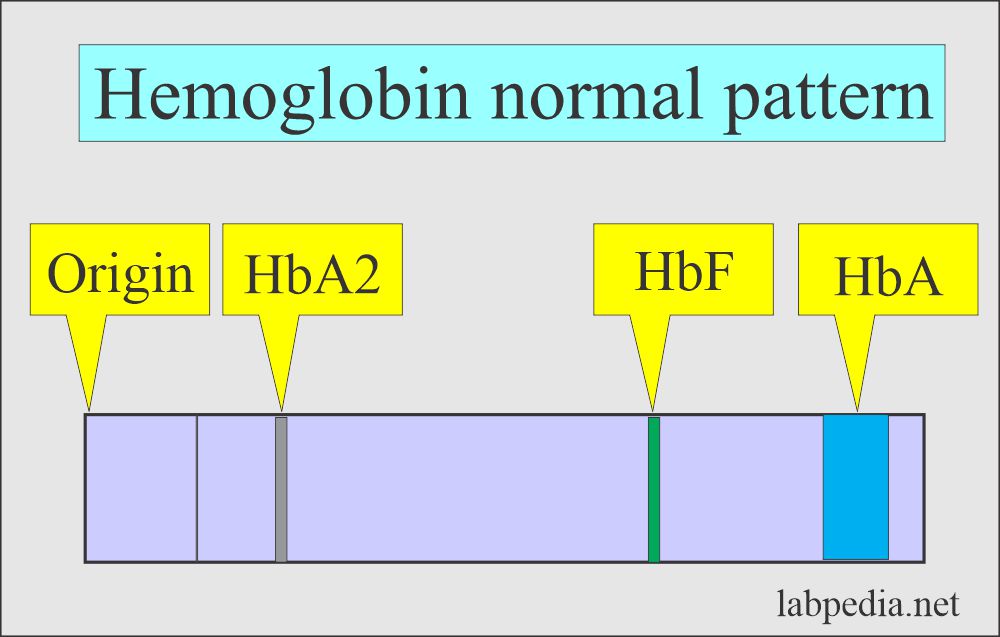
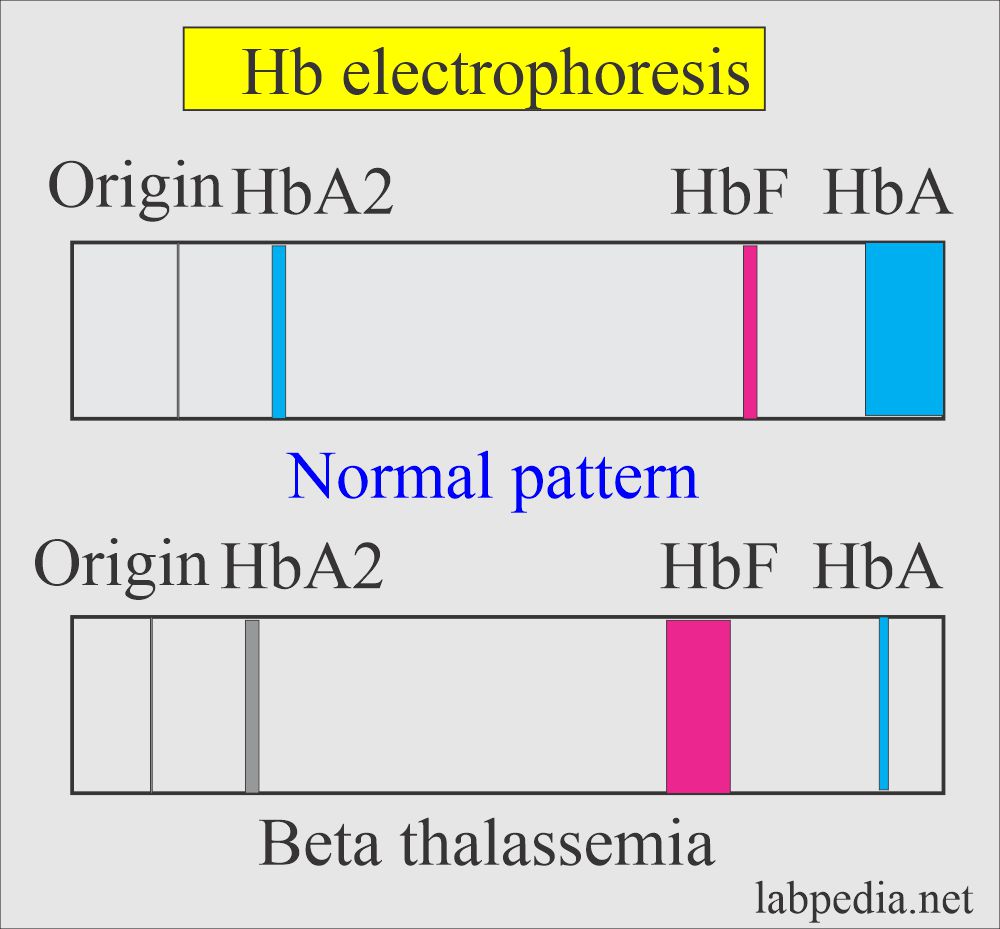
- Hemoglobin seen on electrophoresis shows a very small band of HbF.
- HbF is the normal hemoglobin in fetuses and infants.
How will you Define Fetal Hemoglobin (HbF)?
- It is the main fetal protein carrying oxygen in the fetus during the last 7 months of the fetal uterine life.
- It will persist in the newborn for roughly 2 to 4 months.
- Fetal Hb has more affinity for oxygen than adult Hb, and it helps to give more oxygen to the fetus from the mother’s circulation.
- Fetal Hb will disappear by the 6th month and only persist in thalassemia.
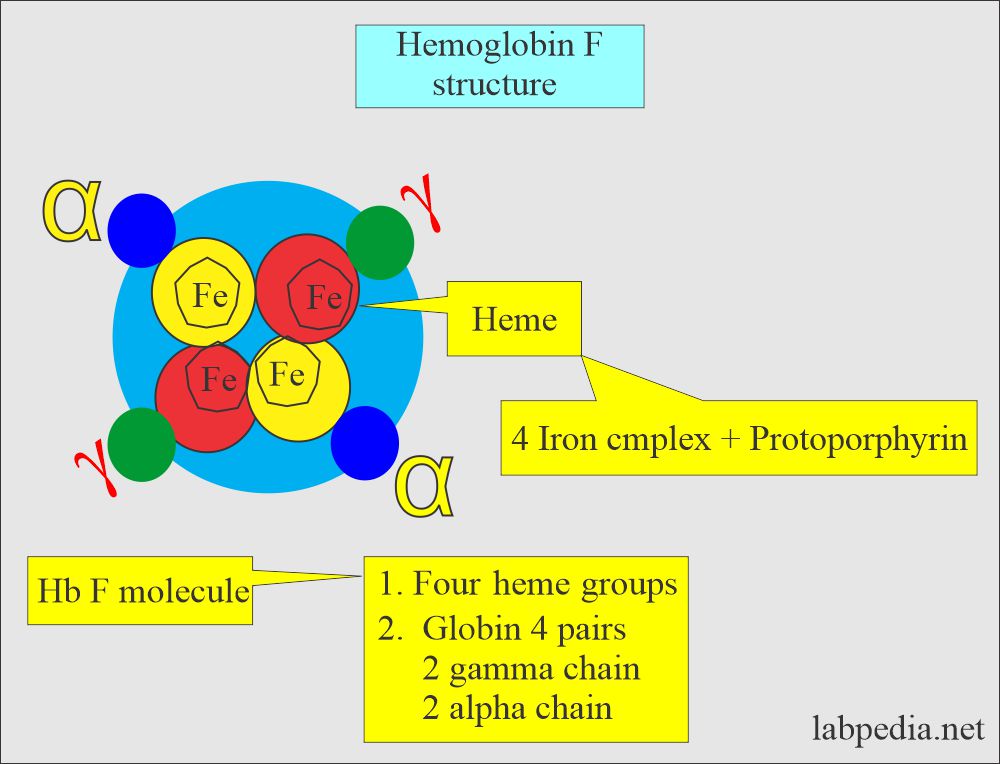
What is the structure of the Fetal hemoglobin?
- Adult hemoglobin A1 (HbA1) consists of α2 β2 chains is 95% to 97%.
- Adult hemoglobin A2 (HbA2) consists of α2 δ2 chains of 2% to 3%.
- Fetal hemoglobin (HbF) consists of α2 γ2 chains of 1% to 2%.
- In adults, Hb A2 and HbF are present in trace amounts.
| Type of hemoglobin | Structure of the hemoglobin |
|
|
|
|
|
|
How much is the affinity of fetal hemoglobin to oxygen?
- HbF has a greater affinity to bind with oxygen than adult hemoglobin and gives better oxygen to the developing fetus from the mother’s blood circulation.
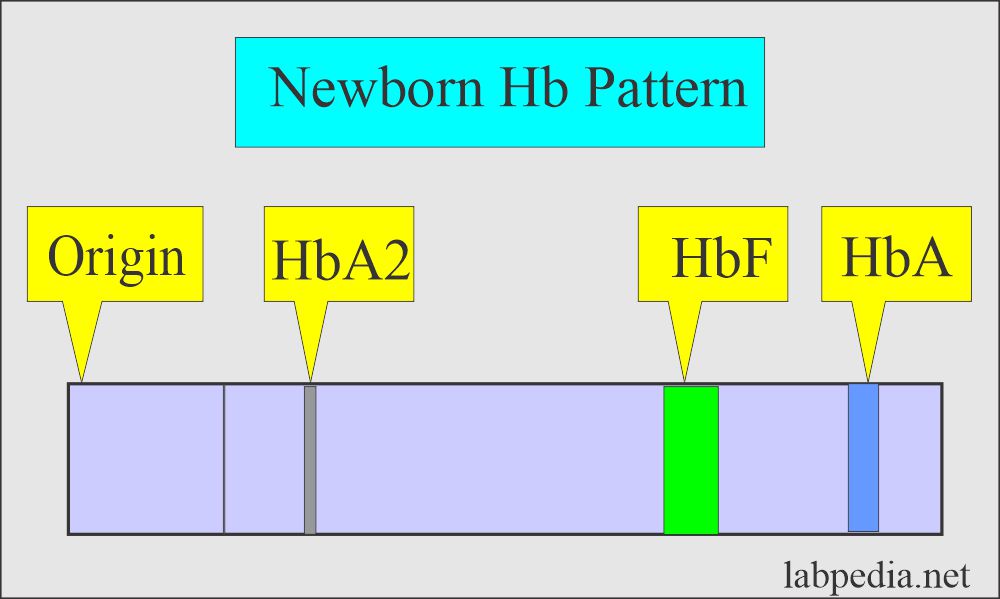
- HbF is the major Hb present during gestation.
- HbF makes up 50% to 90% of Hb in newborns.
- The rest of the Hb in the newborn is HbA1 and HbA2.
- HbF is replaced by adult Hb (HbA) at 6 to 12 months. This will be less than 1% of the adult.
- In the normal situation in an infant’s first year, this HbF is replaced by HbA1 and HbA2.
- If HbF persists over 5% after 6 months, then that is a sign of abnormality.
- HbF is resistant to alkali denaturation, so this technique is useful for screening the patient.
- Electrophoresis is more reliable for confirming the HbF by alkali denaturation test and more helpful at a higher level of HbF.
How will you explain Feto-maternal hemorrhage?
- Fetal Hb may be present in mother circulation because of fetal-maternal hemorrhage, which causes leakage of the cells into the maternal circulation.
- Increased Feto-maternal hemorrhage may be seen in:
- Trauma to the mother.
- Placental abruption (a serious complication of the pregnancy). This is the early separation of the placenta.
- Fetal Hydrops.
- Placental tumor.
- Amniocentesis in the third trimester.
How does the Leakage of the fetal RBCs take place?
- Massive fetal-maternal hemorrhage may be the cause of 1 out of 50 stillbirths.
- Leakage of fetal RBC may start after the mid-first trimester.
- Near the final term, 50% of the mothers show fetal RBC.
- Total blood loss in this way is 2 ml or less in 96% to 98 %.
- Increased Risk of fetal-maternal hemorrhage is due to the integrity of placental circulation.
- Risk factors for Feto-maternal hemorrhage are:
- Maternal trauma.
- Placental abortion.
- Placental tumors.
- Third-trimester amniocentesis.
- Hydrops fetalis.
- Twin.
- Pale fetal organs (thin, pale, loose, and dry skin).
How will you do the Lab diagnosis of fetal hemoglobin (HbF)?
- The following methods can diagnose HbF:
- Acid elution stain.
- Flow cytometry.
- Chromatography.
- Electrophoresis.
- Alkali denaturation method.
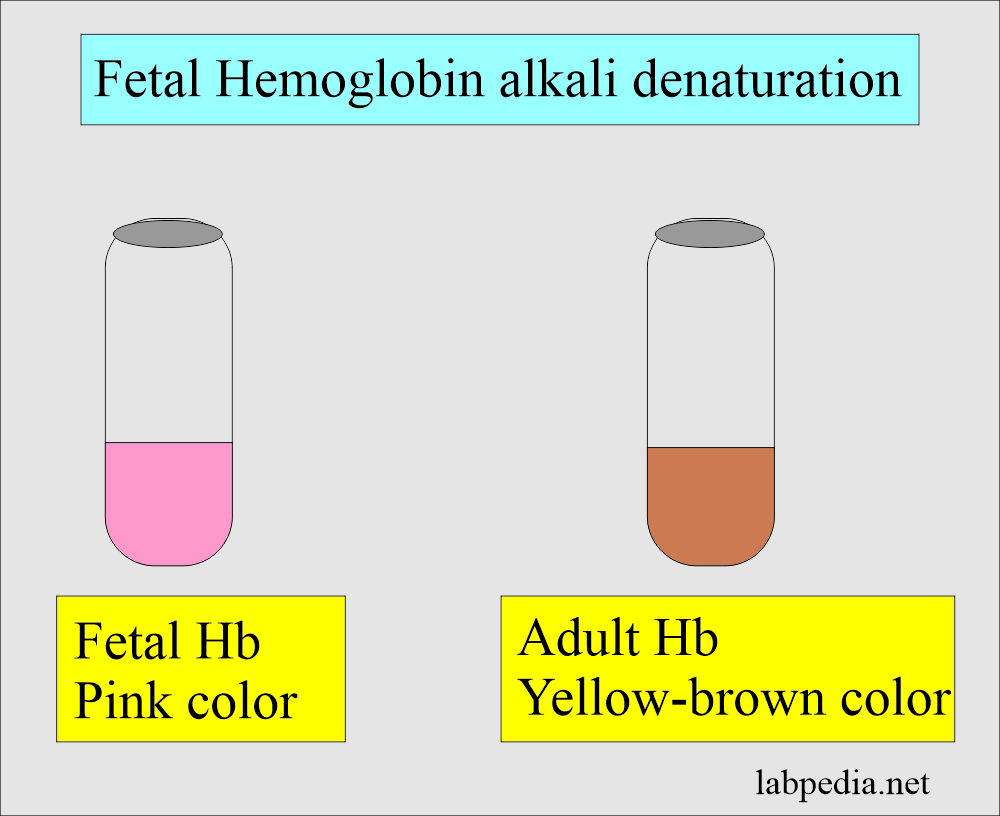
How will you describe the procedure for the alkali denaturation method for Fetal hemoglobin (HbF)?
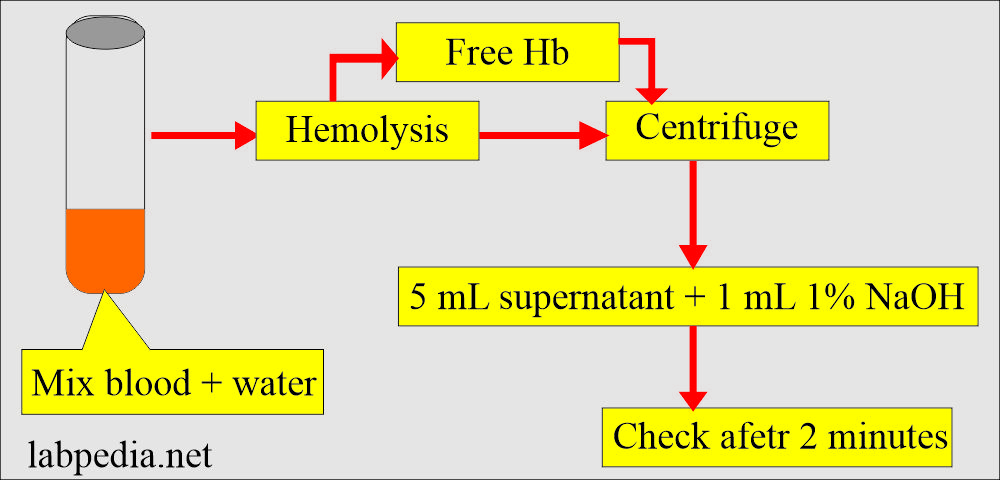
- Fetal hemoglobin is more resistant to strong alkalis than other hemoglobins.
- Mix blood with a small amount of distal water, leading to hemolysis.
- Due to hemolysis, there will be the release of free hemoglobin.
- Now, centrifuge the sample for several minutes.
- Mix 5 mL of supernatant (pink in color) with 1 mL of 1% NaOH.
- Result:
- Check the color after 2 minutes:
- Fetal hemoglobin (HbF) will be pink.
- Adult hemoglobin (HbA) will be yellow-brown because it is less stable and will convert into hematin.
- Check the color after 2 minutes:
Normal Fetal hemoglobin (HbF)
Source 1
| Age | %Hb F |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Source 2 Fetal HbF
- <1% of RBCs
Source 4 Fetal HbF
- Newborn = 60% to 90%.
- By 6 months = 2%.
- Adult = 0 to 2%.
Another source of Fetal Hemoglobin (Hb F)
| Age in days of the fetus/newborn | HbF % |
| 0 to 10 days | 56 to 87 |
| 11 to 20 days | 55 to 83 |
| 21 to 30 days | 51 to 76 |
| 31 to 40 days | 46 to 70 |
| 41 to 50 days | 38 to 62 |
| 51 to 60 days | 31 to 54 |
| 61 to 70 days | 24 to 44 |
| 71 to 80 days | 17 to 34 |
| 81 to 90 days | 12 to 28 |
| 91 to 100 days | 8 to 24 |
| 101 to 110 days | 7 to 18 |
| 111 to 120 days | 5 to 15 |
| 121 to 130 days | 4 to 10 |
| 131 to 140 days | <6.1 |
| 141 to 364 days | <4.1 |
| One year and above | <2.1 |
What are the conditions where there is increased Fetal hemoglobin (HbF)?
- Hereditary causes.
- Homozygous beta-thalassemia (20% to 100% HbF).
- Heterozygous beta-thalassemia (up to 5% HbF).
- Hereditary persistence of HbF (Homozygous 100 % and in heterozygous is 15% to 35 %).
- Sickle cell anemia (≤ 30 % HbF).
- Acquired causes (up to 10% HbF).
- Pernicious anemia.
- Refractory normoblastic anemia.
- Pure red aplasia.
- Aplastic anemia.
- Sideroblastic anemia.
- Pregnancy and molar pregnancy.
- Juvenile chronic myeloid leukemia.
- Hyperthyroidism.
- Erythroleukemia.
- Chronic renal diseases.
- Leakage of fetal RBC into maternal circulation ( FMH ).
Thalassemia and Fetal Hemoglobin (HbF)
- There is no Thalassemia hemoglobin. Actually, this is a complex group of genetic abnormalities of globin chain synthesis.
- Thalassemia is divided into two main groups.
- α-thalassemia.
- β-thalassemia.
- There are three major clinical groups:
- Thalassemia major shows HbF 40% to 90%. It is associated with severe and often life-threatening clinical manifestations.
- Thalassemia minor shows HbF 5% to 10 %. It has mild clinical manifestations.
- Thalassemia with other hemoglobinopathies.
- The continuous production of HbF leads to severe anemia and death.
Question and answers:
Question 1: What is the importance of the HbF?
Question 2: What is the structure of the fetal Hb?

Great I enjoyed for reading.
Thanks.
Hello, thank you for an interesting article! could you please write where I can read more about this?
You can read District laboratory practice in Tropical countries by Monica Cheesbrough.