Enteric Fever:- Part 1 – Typhoid Fever (Salmonella typhi), Diagnosis and Treatment
Typhoid Fever (Salmonella typhi)
Typhoid Fever, Enteric Fever (Salmonella typhi)
What Sample is needed to diagnose Typhoid Fever?
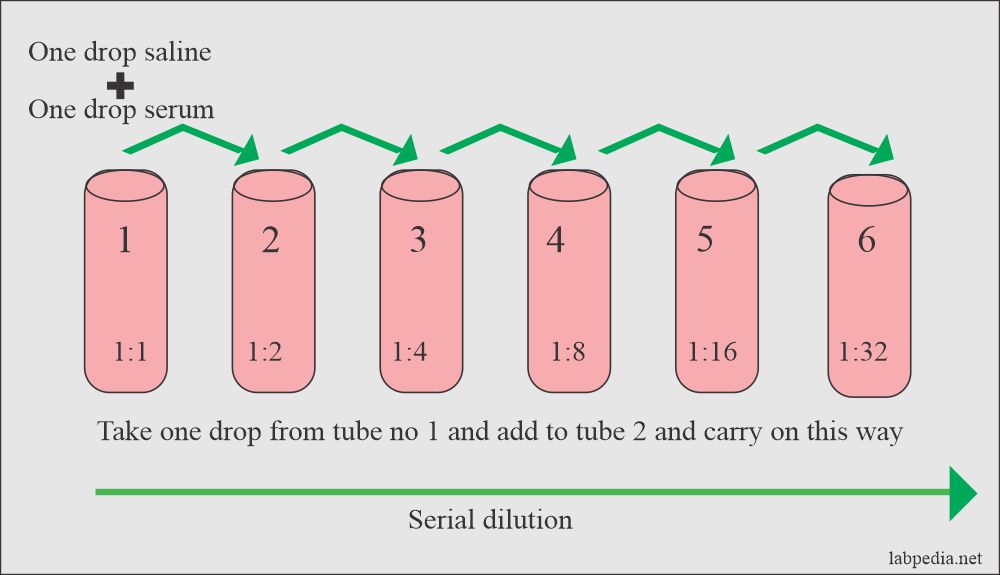
- A widal test can be done on the serum of the patient.
- Feces can be used for the culture.
- A blood culture can be done and is positive in the early stage of the fever.
- Urine may also be needed for the culture.
- In a few cases, a bone marrow sample can be cultured.
What precautions will you take for diagnosis of Typhoid Fever?
- The widal test will be positive after 7 to 10 days of the onset of the fever.
- Culture gives the early result to detect the bacilli.
How will you define Typhoid Fever?
- Typhoid fever is due to infection by Salmonella typhi and Salmonella paratyphi.
- Salmonella typhi is only present in humans; no animal reservoir has been found.
- Typhoid/Enteric fever is a syndrome that is characterized by the following:
- Fever.
- Headache.
- Cough.
- Splenomegaly.
- Leucopenia.
What are important facts about Typhoid Fever?
- Typhoid fever is caused by Salmonella typhi, also called enteric fever.
- Enteric fever is an acute illness characterized by fever, headache, and abdominal discomfort.
- This clinical syndrome is characterized by fever, GIT symptoms, and headache.
- Salmonella infections are divided into:
- Typhoidal infection caused by S.typhi.
- S. paratyphi generally has a less severe illness caused by S. Paratyphi A, B, or C.
- Non-typhoidal infection is most common in the USA, caused by:
- S. Typhimurium.
- S. Enteritidis.
- Salmonella is uncommon in the USA; 70% are acquired abroad.
- Humans are the only source of this infection (S. Typhi and S. paratyphi), and the spread is from person to person or via contaminated foods or water.
Discus Epidemiology of Typhoid Fever?
- Salmonella habitat is an animal gut. Predominantly, animal pathogens can also cause disease in man.
- Foodstuffs from animal sources are important vehicles in the transmission of infection.
- Salmonella is found in humans as well as in chickens and eggs.
- It spreads by eating the chickens and uncooked eggs.
- It spreads only through close contact with an acutely infected person or chronic carrier.
- Most cases occur through contaminated foods or water.
- This is a global issue, with 13 to 17 million cases and ∼60,000 deaths yearly.
- Children under one year are more prone to develop an infection, and the diseases are more severe.
- There is increasing antibiotic resistance to this disease.
- Enteric fever includes typhoid and paratyphoid fever.
- Paratyphoid fever is generally milder than typhoid fever.
- The Salmonella species cause typhoid fever.
- Salmonella typhi and S.paratyphi differ from the other species because man is the only natural host.
How will you classify Salmonella typhi?
- Salmonella typhi and S. paratyphi differ from the other species because humans are the only natural hosts.
- Salmonella serologically divided into:
- Salmonella typhi.
- Salmonella cholerae-suis.
- Salmonella enteritidis.
- Salmonella differs from the other types because it lives in the gastrointestinal tracts of animals and infects humans when food or water is contaminated with animal feces.
- S.Typhi can grow on ordinary media.
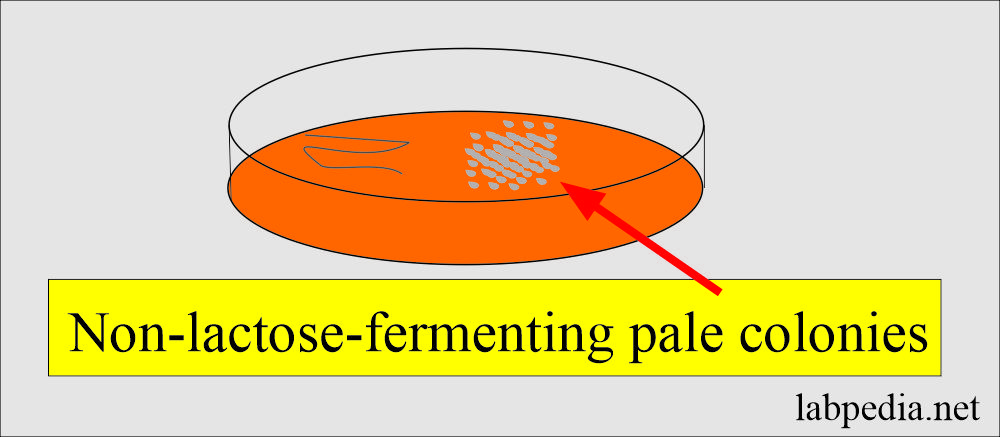
- Culture on the MacConkey agar (or Desoxycholate citrate agar) will see pale, non-lactose fermenter colonies from the feces.
- Colonies on Xylose lysine desoxycholate agar show a red-color colony with a central black area.
- Wilson’s and Blair’s Bismuth sulfite agar shows black metallic colonies due to H2S production.
- S.Typhi are motile due to flagella.
- Generally, salmonellae produce acid and gas from carbohydrates except for S.typhi, which does not produce gas.
How will you describe the microbiology of Salmonella typhi?
- Gram stain negative bacilli (rods). These are seen as single pairs and chains.
- These are motile.
- These are aerobic.
- Non-lactose fermenter.
- Produce H2S gas.
- Colonies are gray and can grow on ordinary media (blood agar).
- Selective media are:
- Culture may be taken from the feces.
- MacConkey agar = pale non-lactose fermenting coloies.
- Desoxycholate citrate agar = pale non-lactose fermenting colonies.
- Xylose-lysine desoxycholate agar = observe for red colonies with a black center.
- Wilson and Blair’s bismuth sulfite agar = observed black metallic colonies due to H2S production.
- Selenite F and tetrathionate broth for enrichment, then subculture to MacConkey agar.
- Their capsules consist of polysaccharides.
- These are motile with flagella.
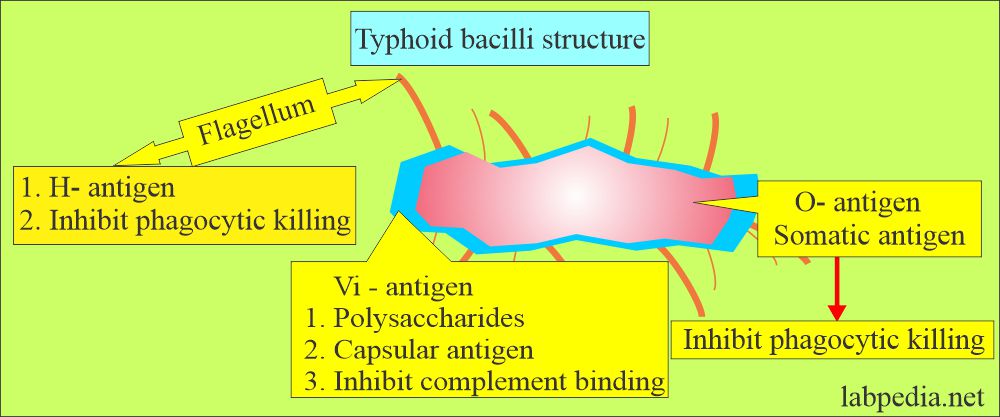
What are the Salmonella antigens (Virulence factors)?
- There are three types of antigens:
- O – antigen (somatic) is present in the body of bacteria. It is an endotoxin and provides antigenic variation.
- This resists alcohol extraction and is thermostable.
- H – An antigen (flagellar) is present in the flagella of the bacteria.
- It provides antigenic variation and motility.
- Flagella antigen undergoes variation by gene rearrangement.
- Vi-antigen (capsular or envelope) is the most superficial of the somatic antigen of S. Typhi. Vi means virulence.
- This polysaccharide capsule surrounds the O antigen, thus protecting the bacteria from an antibody attack on the O antigen.
- This aids in resistance to antibodies and complement.
- There are three respective antibodies:
- Anti-O antibody.
- Anti-H antibody.
- Anti-V antibody.
How will you describe the mode of spread of typhoid fever?
- Contaminated food (including meat).
- Contaminated water supply.
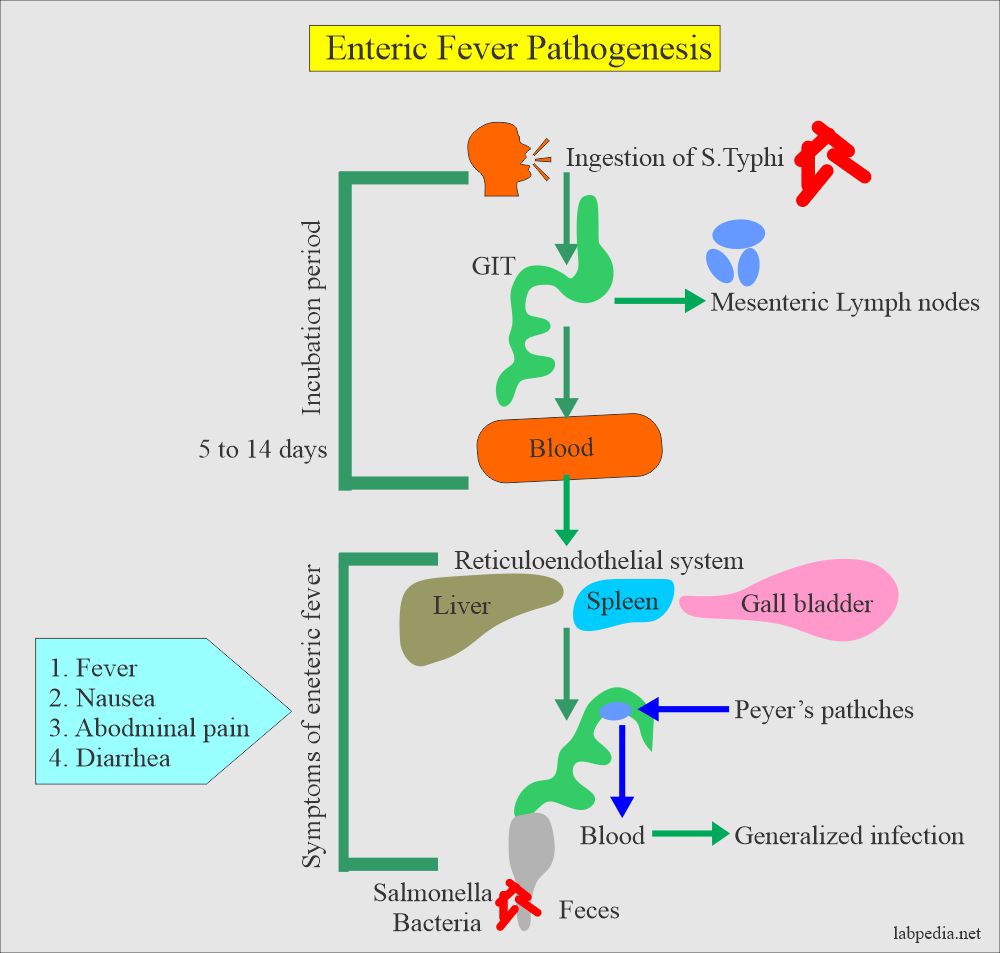
What is the incubation period of typhoid fever (Salmonella typhi)?
- It is 5 to 14 days and sometimes is longer (1 to 3 weeks after exposure and includes fever, headache, and abdominal pain).
- The incubation period for salmonella gastroenteritis is 6 to 72 hours.
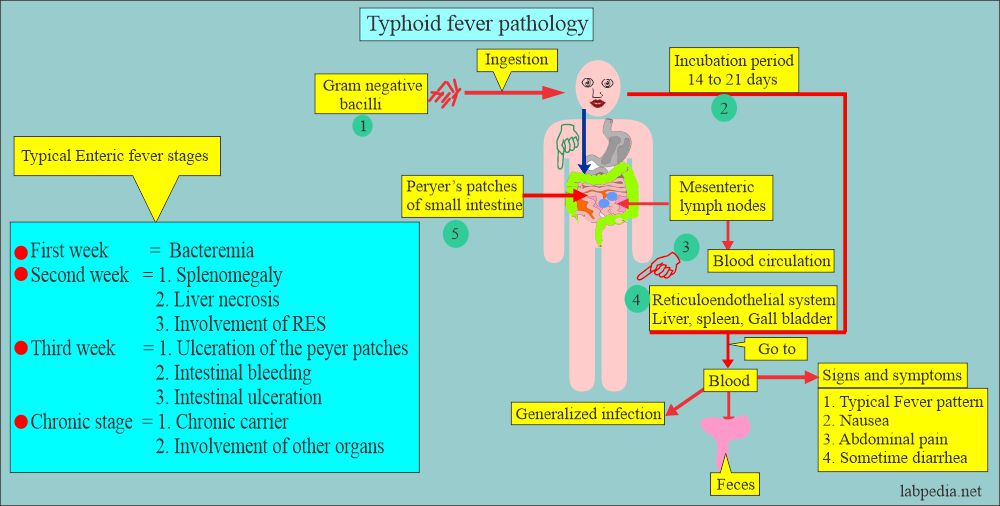
How will you discuss the Pathology of typhoid fever?
- There are three types of disease:
- Enteric fever.
- Gastroenteritis.
- Septicemia.
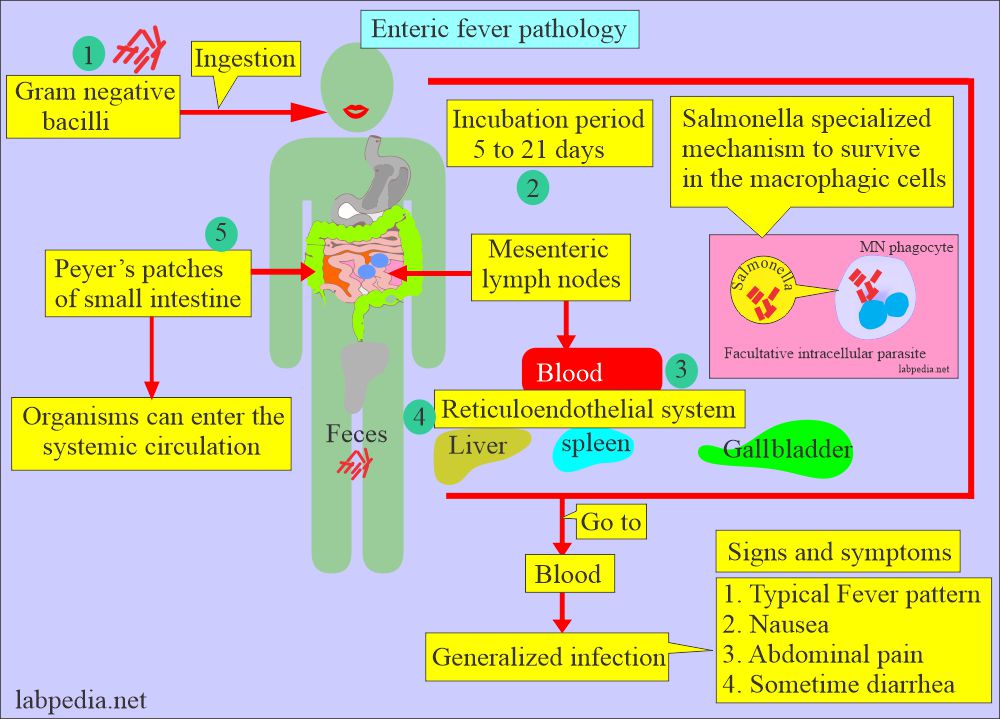
- This organism crosses the intestinal epithelium (invades the regional lymph nodes) and multiplies in the macrophagic cells of Peyer’s patches, mesenteric lymph nodes, and spleen.
- The Peyer’s patches are inflamed and may ulcerate.
- Bacteremia occurs, and the infection spreads to the lungs, gallbladder, kidneys, and CNS.
- Finally, these bacteria settle in various organs.
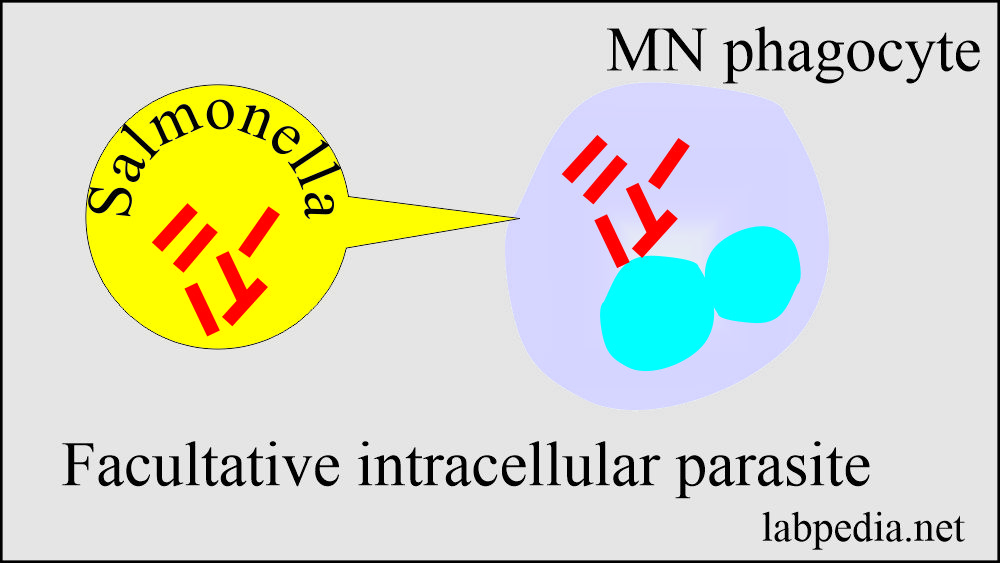
- During this invasion, these bacteria are phagocytosed by the monocytes (mononuclear phagocytes) and can survive intracellularly, so these are called facultative intracellular parasites.
- S.typhi and S. paratyphi A, B, and C cause enteric fever.
- These bacteria cause gastroenteritis, food poisoning, and a few special species that may cause septicemia.
- Rarely, salmonella may cause osteomyelitis, septic arthritis, and other purulent lesions.
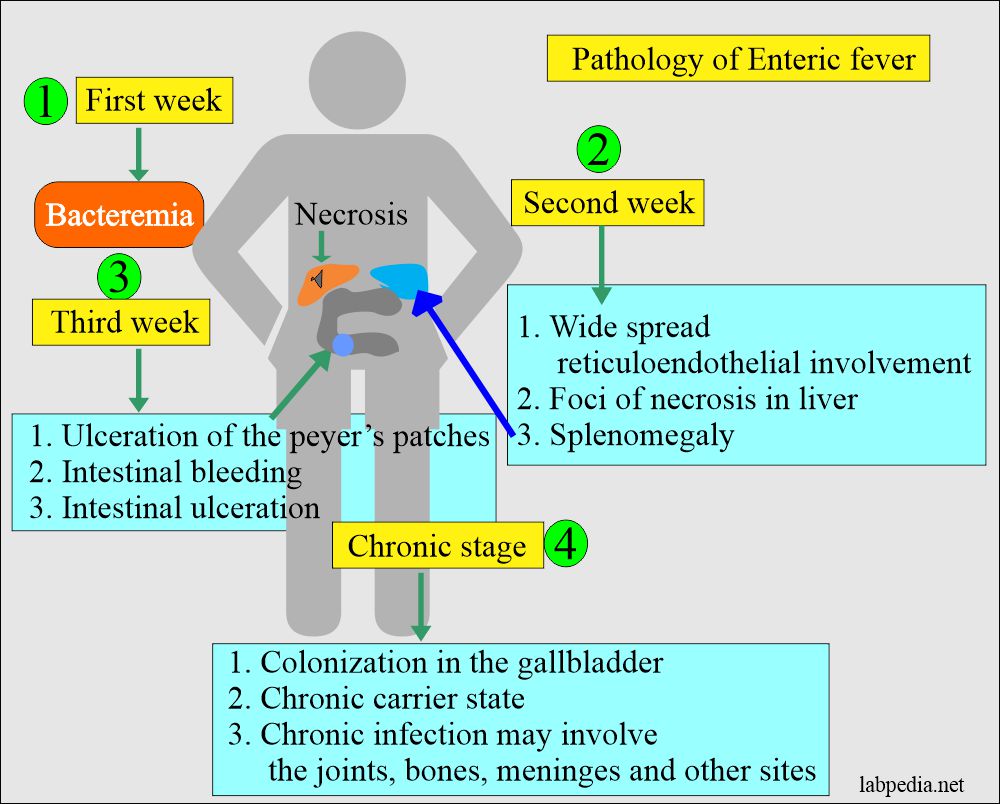
What are the stages of salmonella (Enteric fever)?
The involvement by the salmonella bacteria is in stages.
- In the first week, there is bacteremia.
- Splenomegaly in the second week, widespread reticuloendothelial system involvement, and foci of necrosis in the liver.
- In the third week, peyer patches are ulcerated with intestinal ulcers and bleeding.
- Lastly, these bacteria colonize the gallbladder, leading to a chronic carrier state.
- Chronic infection may lead to infection of the joints, bones, meninges, and other sites.
What are the stages of Typhoid fever (Enteric fever)?
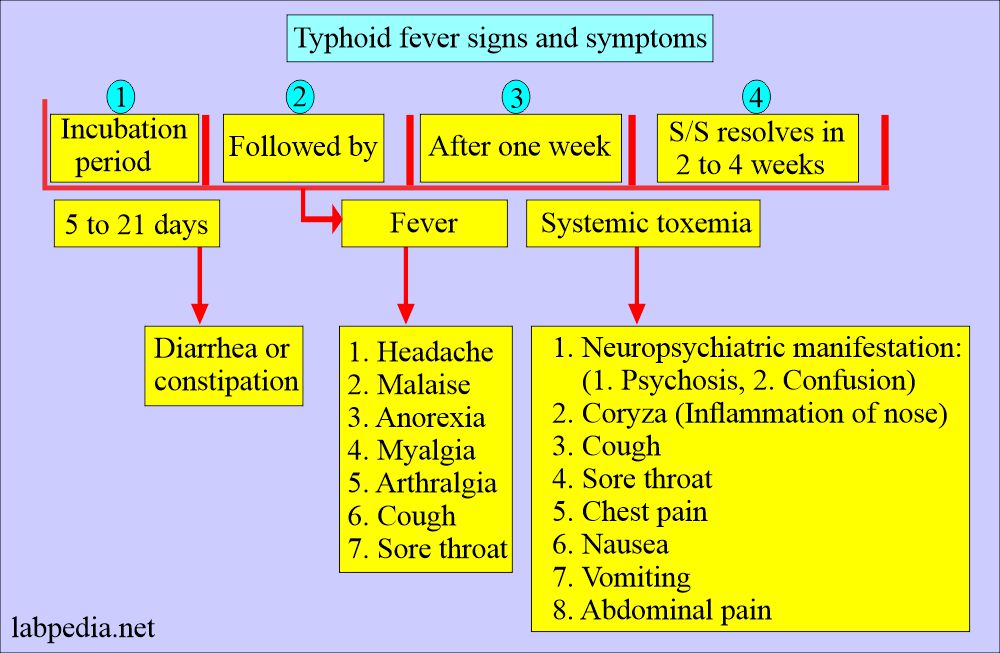
- The onset of illness is insidious and non-specific, with intermittent fever, headache, and abdominal pain.
- Salmonella causes four types of diseases:
- Typhoid fever.
- Sepsis.
- Gastroenteritis (diarrhea).
- Carrier state.
- The incubation time is 7 to 14 days ( and the range is 3 to 60 days).
- The relapse occurs in 5% to 10% of the untreated cases.
- Salmonella infection is more common in children less than ten years of age.
1. Prodromal stage:
- Malaise, headache, cough, sore throat, abdominal pain, and constipation.
- Diarrhea is a late symptom, usually in the third week of illness.
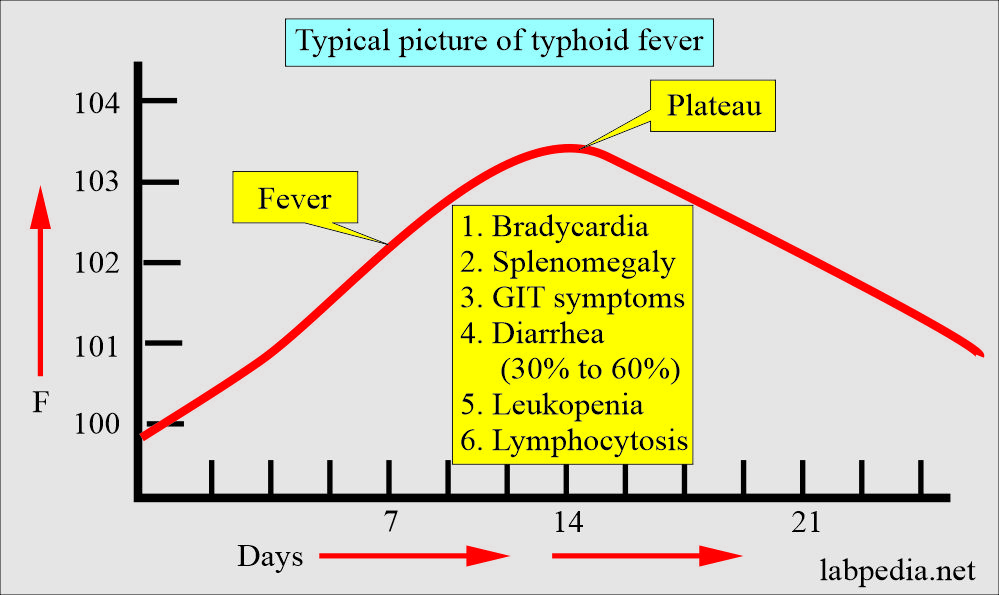
- Fever: It is constant and ascends in a stepwise pattern.
- It rises in the first week, peaks in the second week, and then decreases in the third week.
- 7 to 10 days: There is Paek, and patients are sicker.
- Early diarrhea.
- Abdominal distension and cramps.
- Patients improve after 7 to 10 days.
- Untreated cases recover in about four weeks.
- Symptoms disappear with antibiotics within 3 to 4 days.
- Relapse may occur after two weeks.
2. The gastroenteritis stage:
- The incubation period is 8 to 24 hours.
- There are nausea and vomiting.
- There is abdominal pain.
- There is diarrhea.
- Stools are loose, have moderate volume, and do not contain blood.
- Diarrhea is self-limited and may last for 3 to 7 days.
- There may be a fever.
- Pregnant ladies who get an enteric fever are more prone to abortion.
- This is a self-limiting disease, and recovery is usually within a week.
- Sometimes, S/S may mimic appendicitis or inflammatory bowel disease.
What are the Signs and Symptoms of typhoid fever?
- In the early stage, there is abdominal tenderness.
- Hepatosplenomegaly.
- Scanty maculopapular rash (rose spot).
What are the Complications of Typhoid Fever (Salmonella typhi)?
- There are complications without treatment or even after the treatment, usually after the third week of the disease, like:
- Meningitis.
- Typhoid abscess is rare, and it may occur in various organs.
- Lobar pneumonia.
- Myocarditis.
- Osteomyelitis.
- Intesitinal hemorrage.
- Intestinal perforation.
- By the 4th week of the illness, the patients gradually improve, but 30% of the patients will die in developing countries.
- 10% of the untreated cases will have relapses.
- 1% to 2% of the cases in the USA have mortality.
- There may be:
- Relapse.
- Intestinal Perforation.
- Hemorrhage in the GIT.
- Myocarditis.
- The lungs may show a pneumonia picture.
- Rarely periostitis.
- Most pregnancies end up in abortion.
- There may be bacteremia.
- When salmonella enters the bloodstream, sepsis infects the lungs, brain, and bone.
- Late complications:
- Intestinal hemorrhage may occur in 20% of cases, usually during the 2nd or 3rd week.
- It is less common in treated cases.
- Intestinal perforation occurs in 3% of untreated patients.
- Relapse occurs in one-fifth of the patients.
- Secondary suppurative lesions are seen in the lung (pneumonia), parotid gland (parotitis), and furunculosis.
- Laboratory findings due to complications are:
- Increased levels of LDH, Alkaline phosphatase, and SGOt enzyme.
- There is increased CPK in some of the patients.
- Abnormal liver function tests.
How will you define the Carrier state of enteric fever (Typhoid fever) patient?
- Roughly 30% of the patients become carriers due to persistent gallbladder infection.
- After the clinical recovery, 5% to 10% of the patients will continue to excrete S. typhi for several months, which is the convalescent carrier.
- 1% to 4% of the patients continue to carry the organisms for >1 year; this is a chronic stage.
- These people have no active disease and are symptom-free.
- The bacteria from the gallbladder are constantly discharged into the intestine and ultimately go out in the feces.
- The carrier may have cholecystitis and gallstones.
- It is difficult to eradicate the carrier of S. Typhi from the gall bladder.
- Antibiotics are effective in some of the carriers.
- In most cases, bacteria persist and give rise to long-term permanent carriers.
- Some carriers require surgical removal of the gall bladder to cure them.
- Important: Everybody should wash their hands when they come out of the toilet/washroom.
- Pregnant ladies end up with abortions due to enteric fever.
How will you diagnose enteric fever (typhoid fever)?
- CBC shows:
- Low TLC, leucopenia.
- 4000 to 6000/cmm in the first two weeks.
- 3000 to 5000/cmm during the next two weeks.
- >10,000/cmm may suggest perforation or suppuration.
- ESR is usually decreased.
- There is normocytic anemia. In case of bleeding, this may become hypochromic and microcytic anemia.
- Culture of blood, bone marrow, intestinal secretion, feces, and urine can be done.
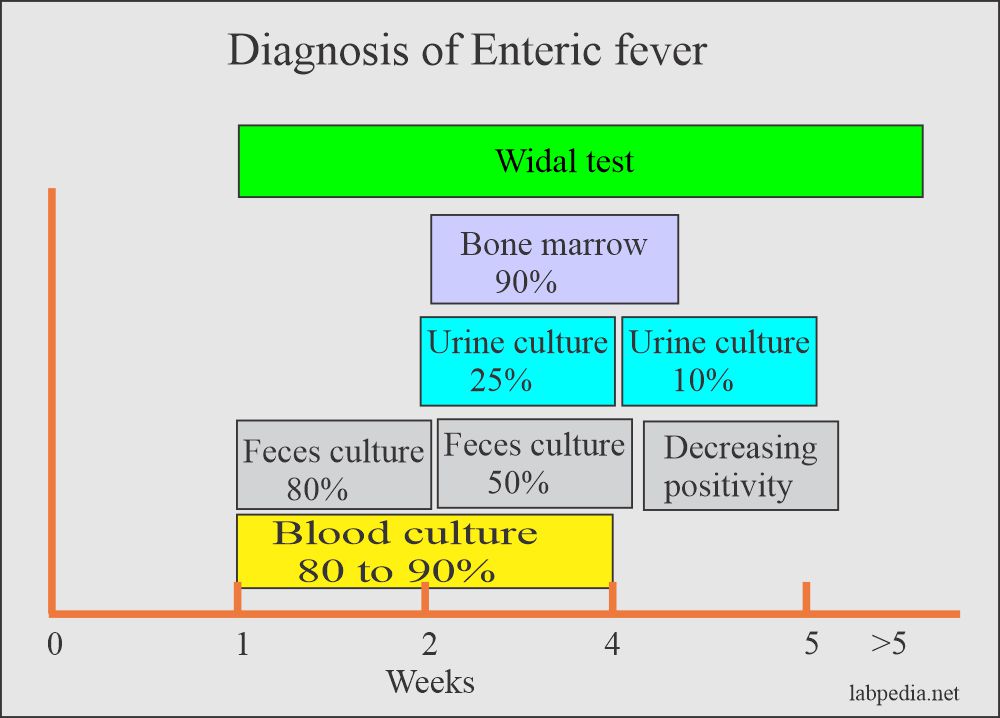
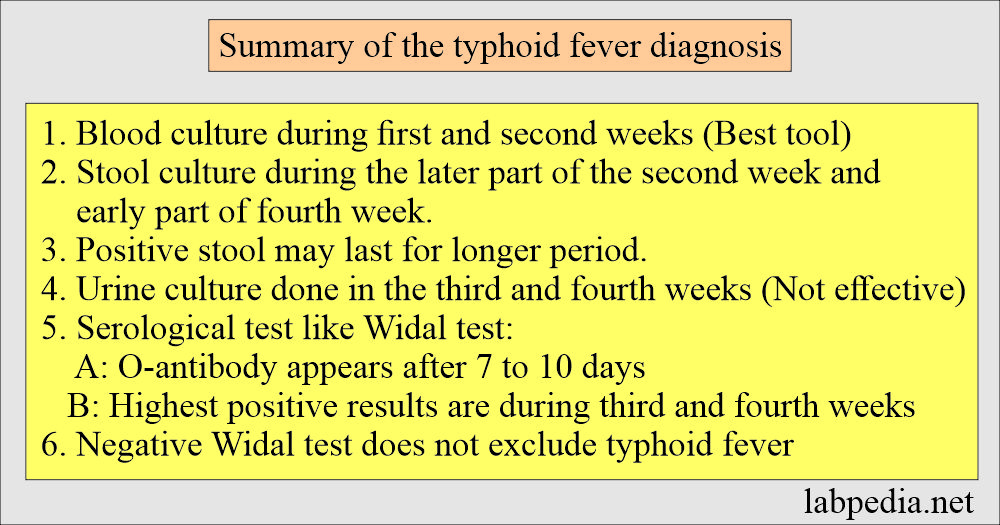
- Blood culture: When you take>15 mL is positive during the first 10 days of infection, positivity may reach 90% and even in the relapse.
- <30% of cases are positive in the third week.
- It is positive in the first week of infection in 80% of the cases. But blood culture may reach 90% of the cases, decreasing to 50% in the third week.
- Roughly 105 to 109 organisms are required for the culture, but this count may be low in infants and older adults.
- This count may be low in patients taking antacids and H2 receptor blockers.
- Blood culture is positive in 80% of the cases in the first week of infection.
- Blood culture is considered 100% specific.
- Buffy coats may decrease the time for isolation.
- This is subcultured on the MacConkey media.
- Roughly 105 to 109 organisms are required for the culture, but this count may be low in infants and older adults.
- Bone marrow culture is more sensitive than blood culture but is usually unnecessary.
- These bacteria (Salmonella) are:
- Non-lactose fermentor.
- Motile.
- Produce H2S.
- Bone marrow culture will be positive and may have a high yield of up to 90% sensitivity. Bone marrow culture is more sensitive (80% to 95%), irrespective of the stage and even with antibiotic therapy.
- Stool:
- Stool examination shows leucocytes and rarely RBCs.
- Stool culture:
- It will be a positive but not reliable test. This will be positive within the first 7 to 10 days of infection.
- The positivity frequency increases up to the fourth or fifth week in <50% of the cases.
- This is negative in 60% to 70% of the cases during the first week if the patient is untreated, then positivity in these patients in the third week.
- The chronic carrier may have stool culture positive even up to one year.
- Positive stool culture after four months indicates carrier states (3%).
- Feces cultures on solid selective media:
- Desoxycholate citrate agar where there are non-lactose fermenting colonies.
- McConkey medium shows non-lactose fermenting colonies.
- There is no gas and no fermentation of sugar.
- Xylose lysine desoxycholate agar shows red colonies with a black center.
- Characteristic features of salmonella on culture are:
Lab test Result Oxidase test Negative Indol Negative Lactose (nonlactose fermenter) Negative Urease Negative Voges-Proskauer Negative Simmon’s citrate Positive/Negative TSI (Produce H2S) Positive (except S.typhi is negative) - Salmonella serology:
- It increases titer >4 folds of O antigen (unvaccinated patient).
- Salmonella has five serogroups: A, B, C, D, and E, based on O somatic antigen.
- Based on H-antigen are 1200 serotypes.
- 7 to 10 days, antibody to D-somatic antigen appears.
- These antibodies against O antigens reach their peak in 3 to 5 weeks.
- H-flagellar antibodies appear later on.
- 7 to 10 days, antibody to D-somatic antigen appears.
- Serological diagnosis is unreliable, like the Widal test.
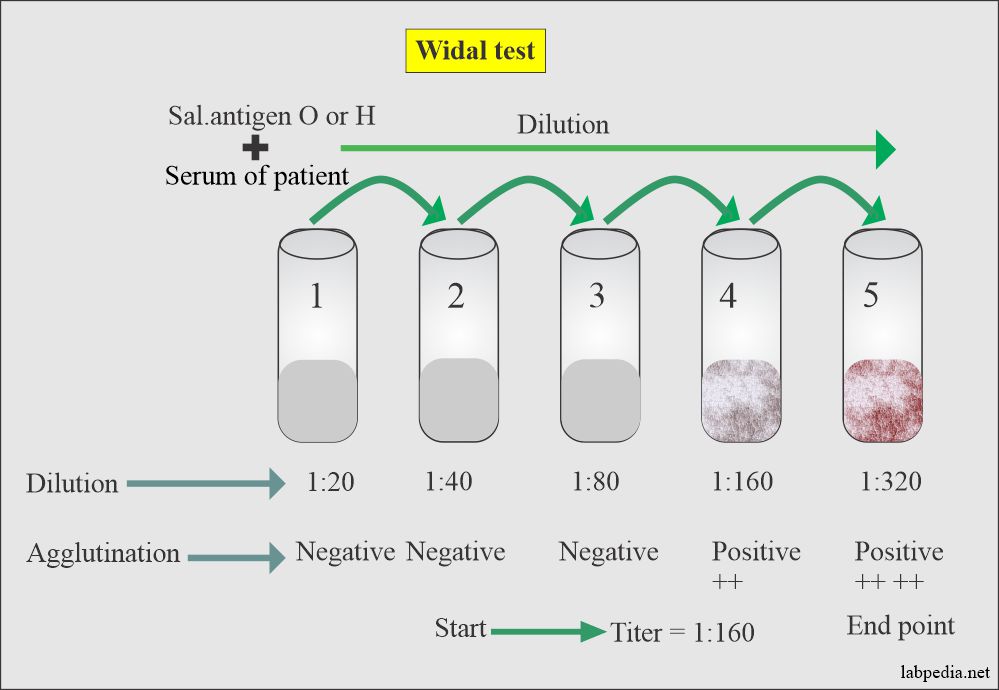
What is the significance of the Widal test for diagnosing enteric fever (Typhoid fever)?
- The widal test was developed in 1896.
- It will be positive after 7 to 10 days of infection.
- The blood, bone marrow, bile, and stool culture is superior to the widal test for typhoid fever or carrier state diagnosis.
- If the culture’s facilities are unavailable, then the widal test is valuable for the diagnosis.
- The titer of O-antibodies 1:80 is suspicious in unvaccinated patients.
- The titer of 1:160 is strongly suggestive of infection in unvaccinated individuals.
- The titer of 1:40 for Antibody to flagellar-antigen (H) is suspicious in unvaccinated individuals.
- While 1:160 is strongly suggestive.
- Titers are much higher in the vaccinated individual.
- H-antigen and antibody titer:
- H-antigen antibodies appear later than the antibody against O-antigen.
- It also disappears later than the O-antigen antibodies.
- Vi antigen for S. typhi is used to screen the carrier. Antibodies to Vi-antigen are positive in only 70% of the chronic carriers of S. typhi.
How will you report the Widal test?
What are the Drawbacks of the Widal test?
- Antibodies are absent in the early illness and may appear after 7 days.
- Antibodies may not develop due to antibiotic therapy.
- Antibody response is variable and does not correlate with the severity of the disease.
- In some patients, there is no adequate level of O-antibody titer.
- The widal test is positive in the vaccinated person or previous infection.
- False positive reactions are seen in autoimmune diseases.
- Early antibiotic treatment may not increase the titer.
- >10% of the cases in endemic areas are seronegative.
How will you diagnose the Enteric fever (Salmonella infection)?
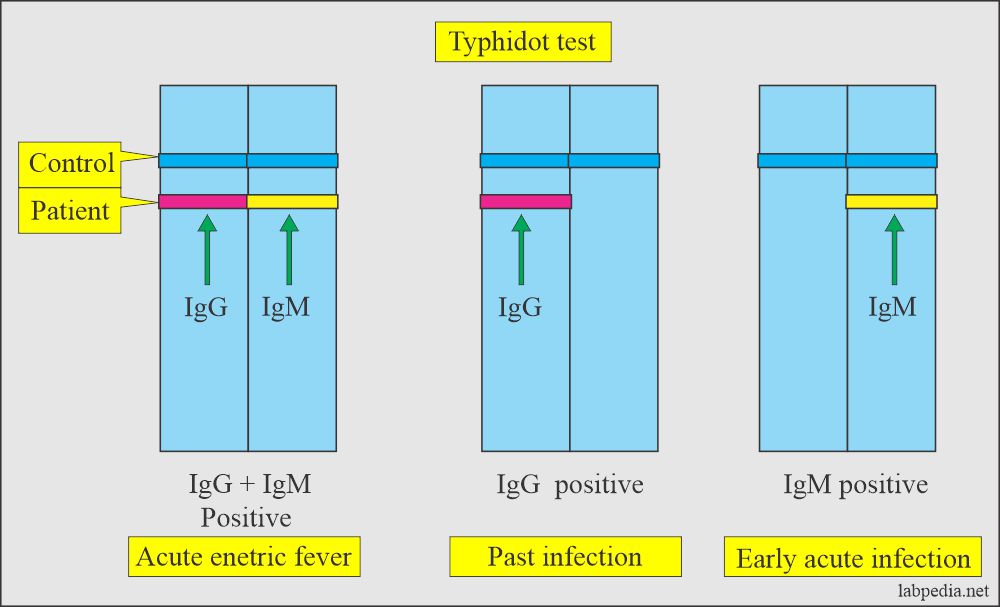
- Typhidot test:
- The manufacturing companies claim that it would be positive after 2 to 3 days.
- The urine culture may be done and is positive in the case of enteric fever but is less sensitive.
- Urine culture is positive during the second to the third week in 25% of the cases, even if the blood culture is negative.
- This is positive in the third or fourth week of the infection.
- This is done on the MacConkey media.
- Bacteriophage typing is done to identify the different strains of S.typhi and Paratyphi.
- This is useful for epidemiological investigations in case of the outbreak’s source.
- Summary of Diagnosis of typhoid fever:
- Samonella is non-motile.
- Biochemical tests show acid and gas formation from carbohydrates.
- S.typhi does not produce gas formation.
- Serologically, it can identify antigens.
- O somatic antigen.
- H flagellar antigen.
- Vi surface antigen
Explain the Summary of the available lab tests for diagnosing Typhoid fever?
What is the Summary of typhoid fever diagnostic tests?
- White blood cell count: It is low during the first two weeks.
- WBC count decreased from 4000 to 6000/cmm.
- 3000 to 5000/cmm during the next two weeks.
- 10,000/cmm or more/cmm may suggest perforation or sepsis (suppuration).
- There may be anemia, and this may be due to bleeding and is hypochromic and microcytic.
- Blood cultures are positive during the first 10 days in 90% of the patients and relapse.
- <30% are positive after the third week.
- Stool culture is positive after the 10th day, increasing frequency up to the 4th or 5th week.
- Stool culture-positive after 4 months indicates a carrier.
- Urine culture is positive during the 2nd to 3rd week in 25% of the patients; even the blood culture is negative.
- Widal test: H and O agglutinins appear in the serum after 7 to 10 days, increase to the peak in the 3rd to 5th week, then gradually fall for several weeks; there is no increase during the relapse.
- O Antibody appears before the H appears and is usually higher at the beginning.
- During convalescence, the H titer becomes higher than the O antibody.
- The widal test may be positive in case of vaccination or previous infection.
- Early treatment with antibiotics may cause titer to remain low or negative.
How will you Treat Enteric fever (Typhoid fever)?
- The drug of choice is Ciprofloxacin.
- Chloramphenicol is also effective, but this may have serious side effects.
- Co-trimoxazole is also used and has less serious side effects than Chloramphenicol.
How will you Treat the carrier of enteric fever?
- The carriers are asymptomatic.
- It is documented that the carrier sheds S.tryphi in the stool for one year and is observed in 1% to 3% of these patients.
- The gallbladder is the site for persistent infection.
- It is difficult to eradicate S. typhi from the gallbladder. Mostly, these are permanent carriers.
- To eradicate carrier infection, prolonged use and a high dose of antibiotics are needed.
- Ampicillin is the drug of choice, but it must be given in higher doses and prolonged.
- Chloramphenicol is not suitable for carriers.
- Ciprofloxacin has good results.
How will you control the typhoid fever?
- The Hygenic measures like:
- Clean water supply.
- Adequate disposal of sewage material.
- Washing of the hands after the defecation. The best is to wash your hands with soap at least three times.
- Take care of food handling and processing.
- For the carriers, give them treatment and advise them to wash their hands after the defection.
- Vaccination should be advised in the family with a history of enteric fever.
- Injectable vaccine.
- The oral vaccine is replacing the injectable vaccines. These are Vi capsular polysaccharides.
What types of vaccines are used for enteric fever?
| Type of vaccine | Dose of vaccine | Remarks |
| Vi capsular polysaccharide (ViCPS) Typhim Vi |
|
|
| Heat killed the whole organism (S.typhi) |
|
|
|
Ty21a (Vivotif Berna) This is live oral, attenuated live bacteria |
|
|
How will you answer the layman’s question?
- The widal test will be positive after 7 to 10 days of typhoid fever.
- O antigen indicates an acute infection and is early to rise.
- H antigen appears later than the O antigen and indicates past infection or vaccination.
- The titer of O antigen 1:40 is negative.
- The titer of 1:80 is borderline; repeat the widal test after 5 to 7 days.
- A rising titer will indicate typhoid fever.
- If the level is the same, typhoid fever is less likely.
- The widal test will be negative in the first 3 to 7 days of typhoid fever.
- In the first few days, advise blood culture.
Questions and answers:
Question 1: What are the complications of typhoid fever?
Question 2: Which salmonella antigen is specific for acute typhoid fever?