Chapter 11:- Type 1 Hypersensitivity reaction, Anaphylaxis, Atopy, and Treatment
HYPERSENSITIVITY REACTIONS
Definition
Hypersensivity reactions are defined as any of the following:
- Hypersensitivity reactions are excessive immune responses leading to damage in the host.
- These are inappropriate immune responses resulting in pathological changes in the host.
- Inappropriate responses to innocuous foreign substances are called allergy or hypersensitivity reactions.
Classification
- Historically these are divided on a time basis:
-
- Immediate reaction: Reaction develops in less than 24 hours.
- Delayed reaction: When reaction develops within 24-48 hours.
- Coomb’s and Gell’s classification: This was given in 1963.
- Ab-dependant reactions (B-L dependant)
-
- Type I = Anaphylactic and immediate reaction.
- Type II = Cytotoxic reaction.
- Type III = Immune-complex disease.
- Ab-independent reaction (T- L dependant)
-
- Type IV = Delayed or cell-mediated immunity.
- Kirk Patrick classification: This was given in 1987:
-
- Class-I = Reagin dependant injury
- Class-II = Cytotoxic reaction
- Class-III = Immune complex disease
- Class-IV = Anti-receptor Ab-reaction
- Class-V = Delayed and cell-mediated
The Coombs and Gell classification is more popular and is commonly used among these three classifications.
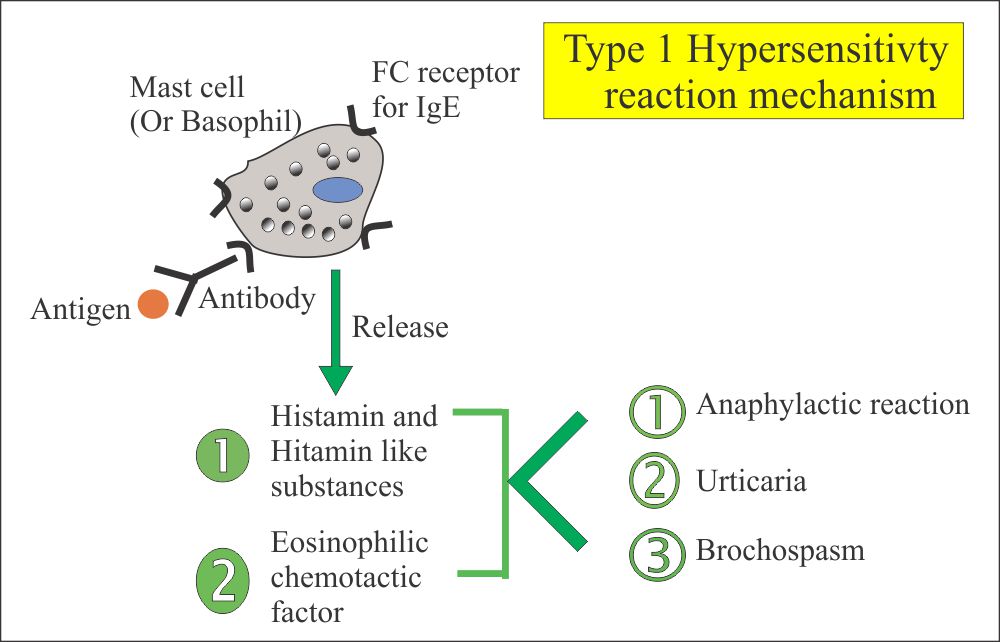
TYPE-I HYPERSENSITIVITY REACTION
- Definition of type 1 hypersensitivity reaction
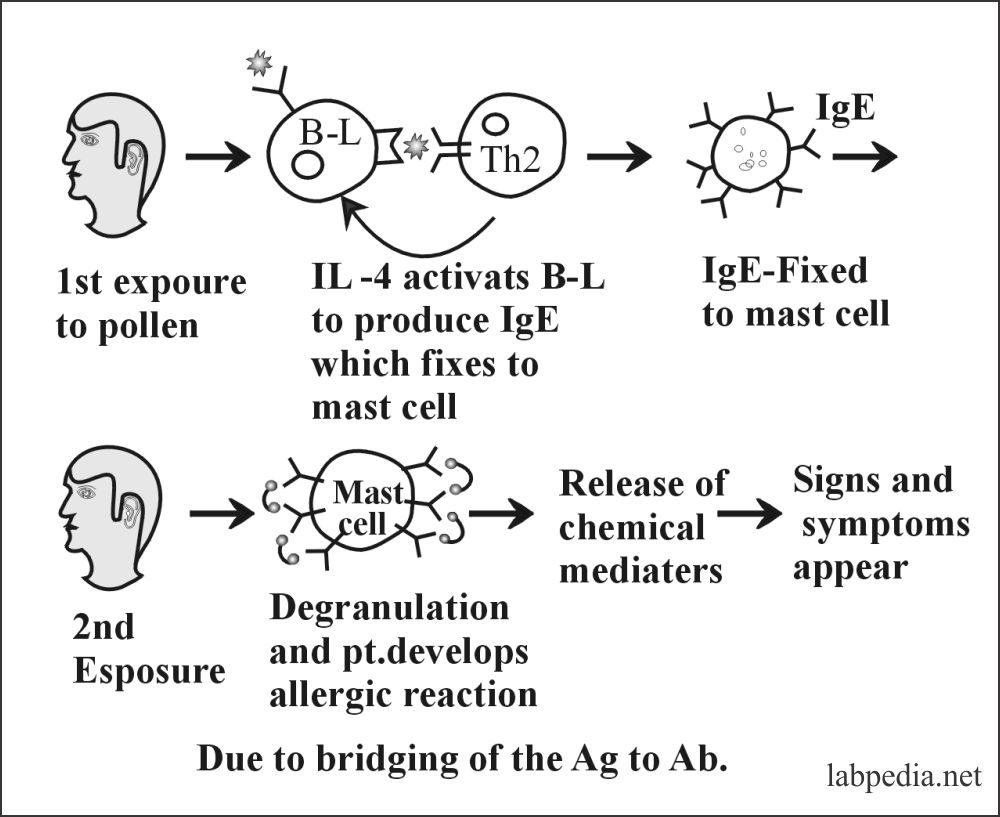
This is also called immediate hypersensitivity when an IgE response is directed against the antigens like pollens and leads to the release of pharmacological mediators, such as histamine IgE-sensitized mast cells, and produces an acute inflammatory reaction with S/S like asthma or rhinitis. - This type 1 reaction can range from the life-threatening anaphylactic reaction to milder forms associated with food allergies.
- Atopic allergy, including hay fever, asthma, and food allergy.
- This is also called an anaphylactic reaction (anaphylaxis – harmful) or allergic reaction. It has two presentations:
- Immediate reaction: This reaction starts within 5-30 minutes and subsides in 60 minutes.
- Late phase reaction: This starts in 2-8 hours and lasts 2-3 days.
- The term allergy was used by Von Pirquet in 1906, meaning the changed reactivity of the host when encountering the antigen on a second or subsequent occasion.
Types of Antigens
- Characteristics of antigen or allergins:
- Any substance which gives rise to the wheel and flare and symptoms of allergic diseases are from various sources.
- When these substances are purified, they have almost all been found to be proteins.
- Their molecular weight varies from 10,000 to 40,000 daltons.
- These proteins are all freely soluble in the aqueous solution but have many different biological functions.
The most common examples of antigens (allergens) are:
| Source of the allergin | Type of airborne particles | Size of the airborne particle |
| Grass | Pollen | 30 µm |
| Dust mite | Feces | 10 to 40 µm |
| Cats | Dander particles | 2 to 15 µm |
| Rat | urine | 2 to 20 |
| German cockroach | Feces and saliva | ≥5 µm |
| Fungi | Spores |
|
Antigens examples:
- Heterologous proteins: e.g., antisera, hormones, enzymes, venom, and pollen.
- Polysaccharides: e.g., Iron-dextran, gives severe reaction, and some other diagnostic agents like iodide and bromosulphophthalin, etc.
- Therapeutic agents: e.g., drugs like antibiotics (Penicillin gives severe reaction) and vitamins.
- Food: e.g., milk, wheat, fish, nuts, and chocolate.
- Insects venoms like bees and wasps.
Type of Antibodies
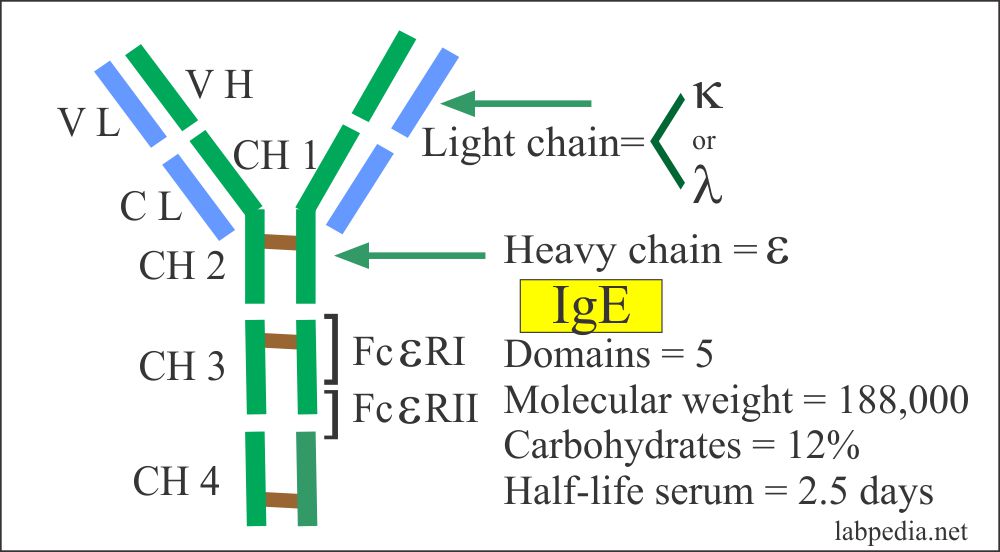
- IgE is the main Ab and is called reagin. It is cytotoxic Ab.
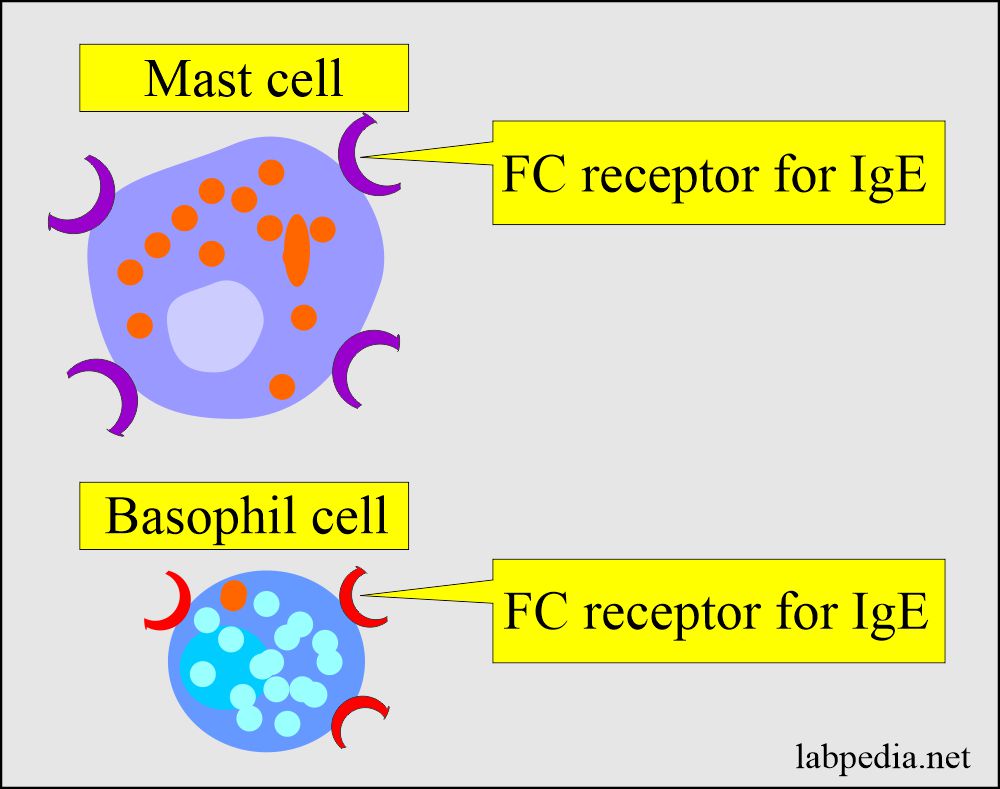
- Once produced, it has love and affinity and attaches to high-affinity receptors (IgεR) present on Mast cells and basophils.
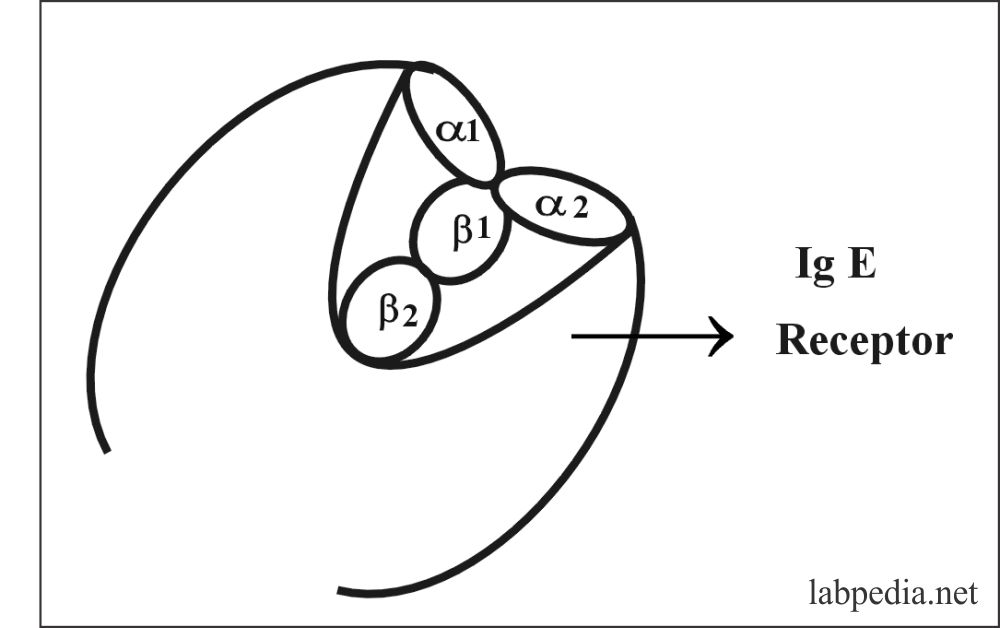
IgE receptor (IgεR) consists of 2-α (molecular weight of 45,000) and 2-β (molecular weight of 30,000) chains.
The Fc-receptor are of two types:
- High affinity is called IgεR1 (IgεRI).
- Low affinity is called IgεR2 (IgεRII)
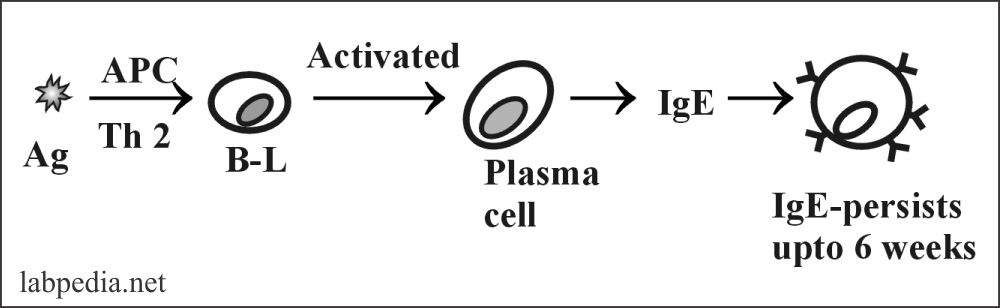
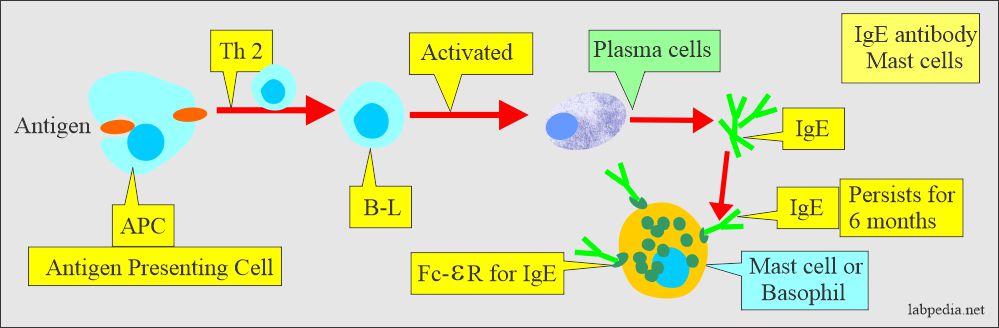
Formation of IgE
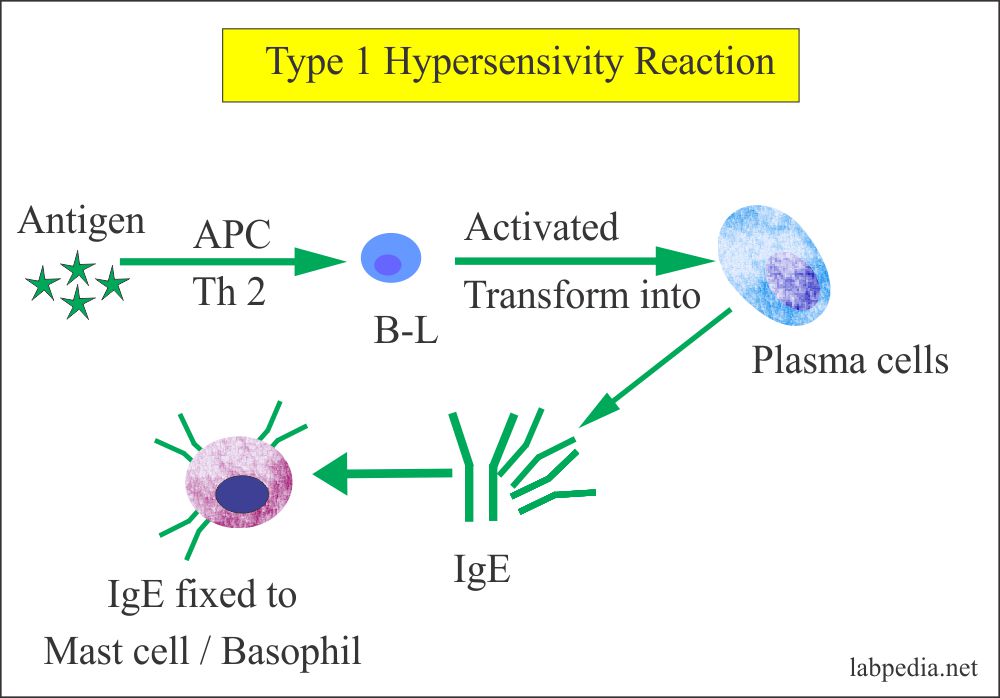
- Antigen stimulates B-L with the help of antigen-presenting cells and Th2. These activated B-lymphocytes are transformed into plasma cells and produce IgE. One hundred molecules of IgE are needed to initiate the reaction.
- IgE is a local response occurring at the entry site of the allergins.
- Locally produced IgE will first sensitize the local mast cells, and the rest of the IgE enters the circulation and binds to the Fc-receptors on basophils and tissue fixed mast cells throughout the body.
- The half-life of serum IgE is only 2.5 days, while mast cells may remain sensitized for up to 12 weeks.
- IgE level is raised in allergic diseases and markedly raised in parasitic infestation.
- There is no transfer across the placenta. In contrast, IgG can cross the placental barrier.
Normal IgE level:
- Serum of normal individual = <10 to 10,000 IU/mL (IU unit = 2.4 ng).
- Most sera contain = <1 µg IgE/mL
- Cord blood = <1 IU/mL (<2 ng/mL)
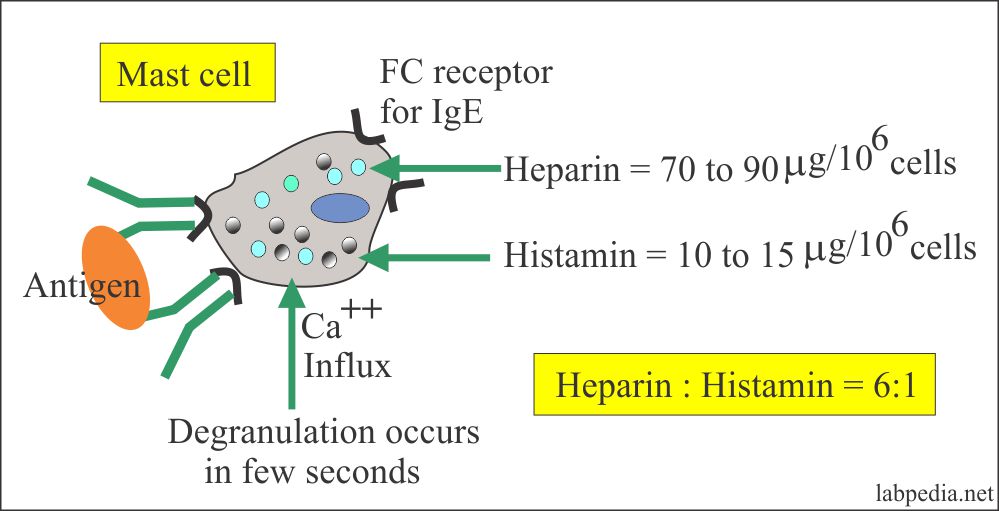
Mast cells:
- Mast cells are found in:
- Around the blood vessels in most of the tissues (Connective tissue mast cells, CTMC).
- Mucosal mast cells are found in the gut and the lungs (Mucosal mast cells, MMC).
- CTMC from the peritoneum and the skin are different in the histamine granules, the density of the staining, and the pharmacological functions.
- MMC is found more in the midgut and the lungs.
- In paracytic infestation, their number increases in the gut.
- Their number also increases in Crohn’s disease and ulcerative colitis.
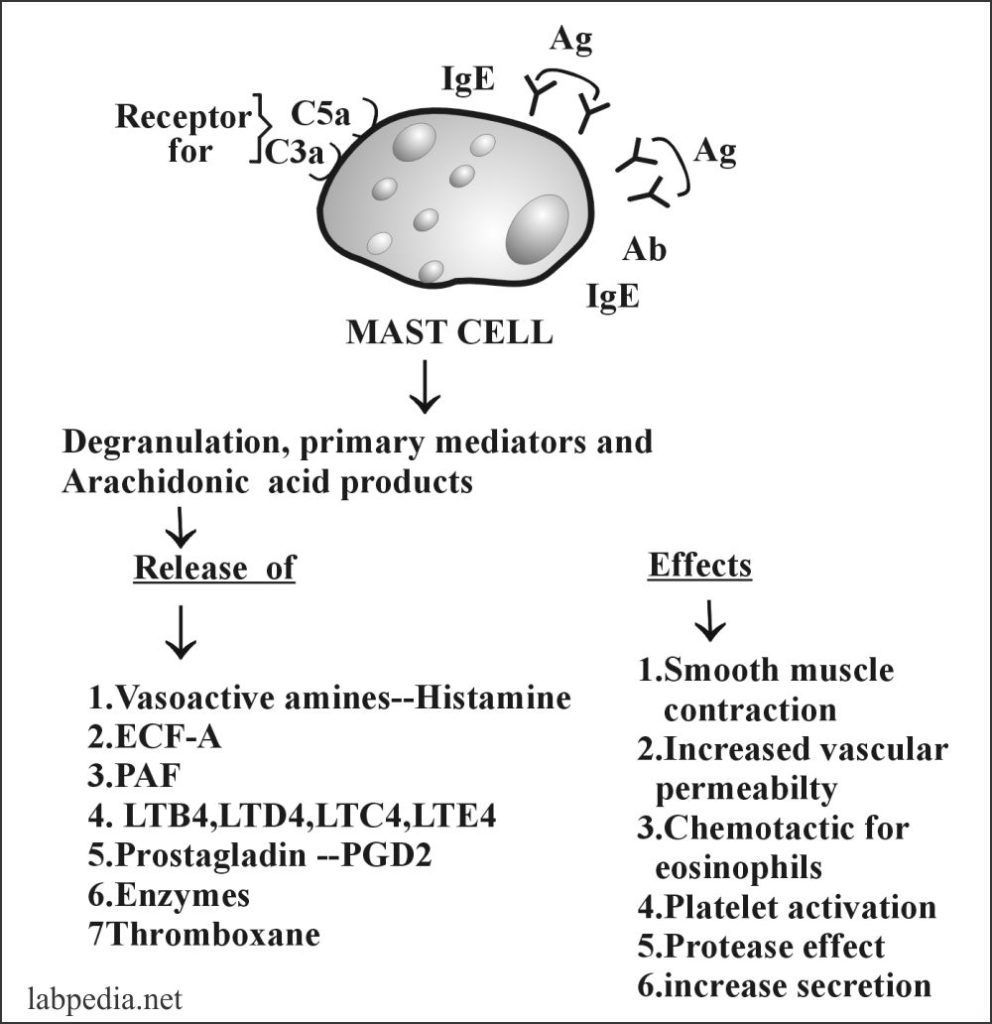
- Mast cells activation:
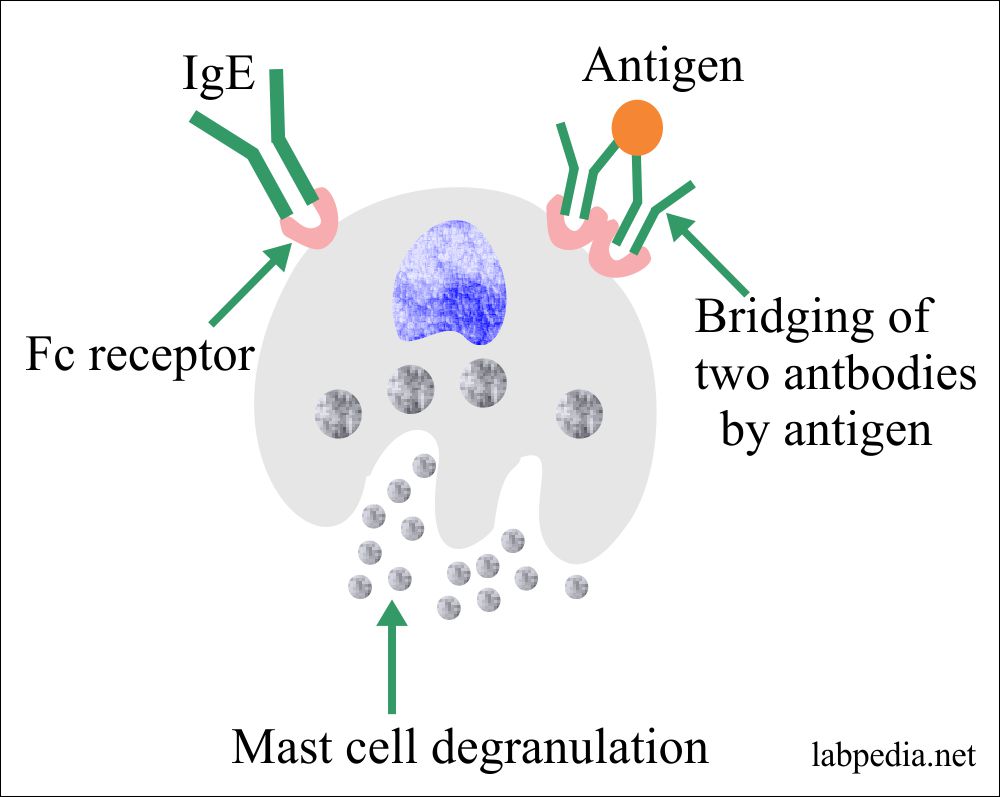
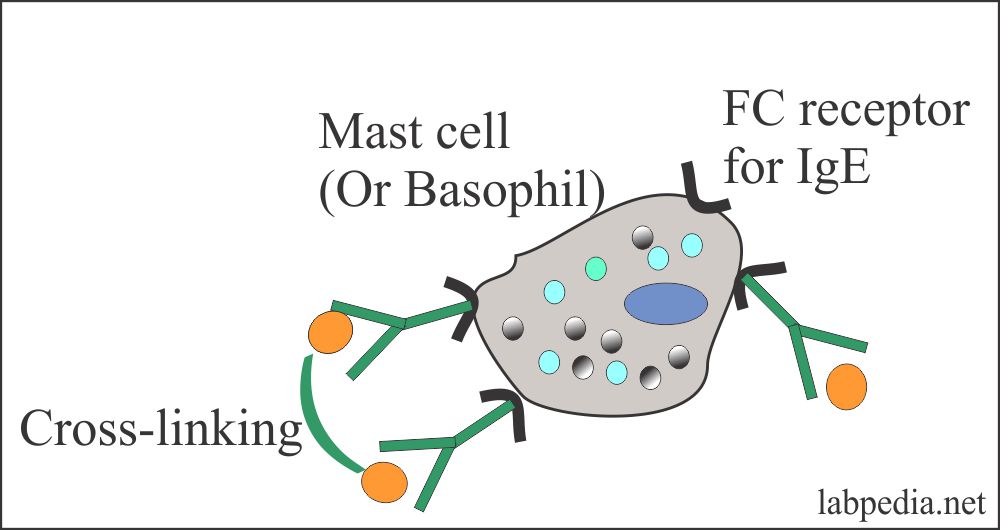
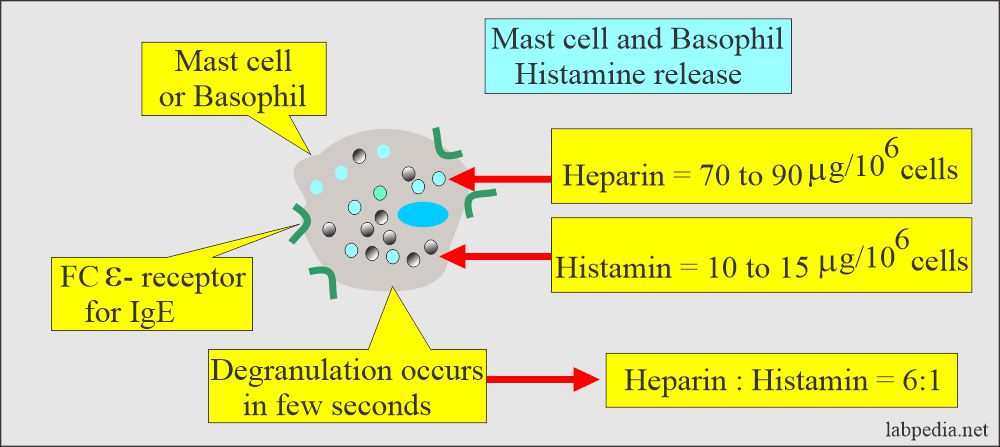
- Once the IgE binds to the Fc receptor on the mast cells and basophils, degranulation occurs by cross-linking the IgE antibody.
Difference between the connective tissue mast cells and the mucosal mast cells:
| Characteristics | Connective tissue mast cells | Mucosal mast cells |
| Location in the body |
|
|
| Functions in the body | Parasitic worm infestation | |
| Morphology | larger in size | Smaller in size |
| Life span in the body | >40 days | <40 days (smaller and short-lived) |
| Intracytoplasmic IgE | Negative | Positive |
| Histamine contents | Positive (++) | Positive (+) |
| T-lymphocytes dependency | Negative | Positive (dependant) |
| Number of Fc-receptors | 3 x 104 | 2 x 105 |
| Cytoplasmic granules |
|
Histamine and serotonin |
| Arachidonic acid metabolites |
|
|
| Effect of drugs (Theophylline, Na cromoglycate) | Inhibit histamine release |
|
The cells with Fcε-receptor are:
- Mast cells and basophils.
- These have IgE-mediated reactions through Fcε-receptor.
- T-lymphocytes have about 1% Fcε-receptor, increasing in the atopy during the pollen season.
- B-lymphocytes, about 30% have Fcε-receptor and increase during the pollen season.
- Monocytes, about 2% have Fcε-receptor and increase up to 20% in allergic conditions.
- Eosinophils have Fcε-receptor that causes damage to the parasites.
- Platelets also have Fcε-receptor.
Type of Cells that take part in type 1 hypersensitivity reaction:
- These are mast cells in the tissue and basophil in the blood.
- Mast cells are of two types:
- Mast cells in the connective tissue.
- Mast cells in the mucosa of the gut.
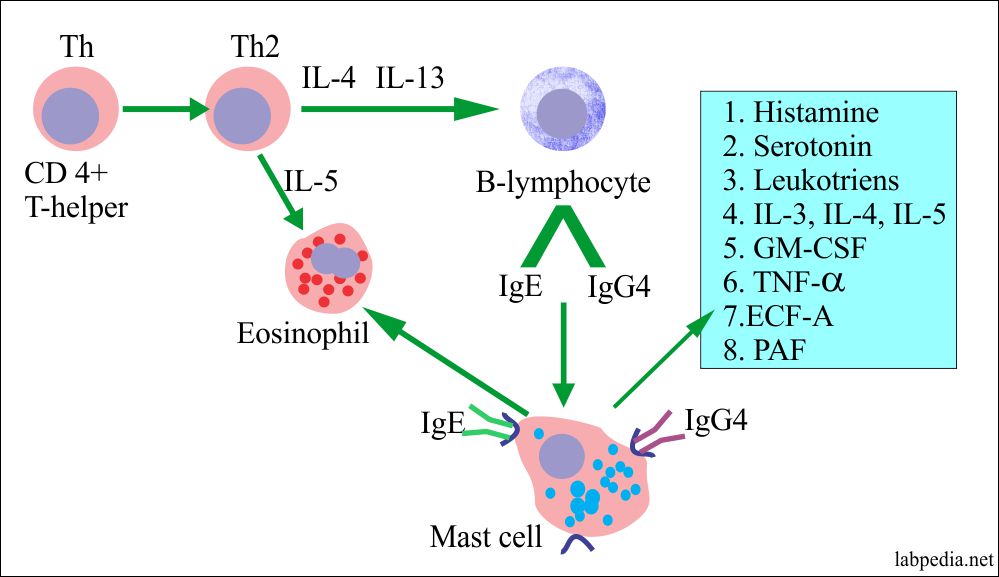
Role of T-lymphocytes in the activation of B-lymphocyte and formation of IgE and IgG4:
- IgE production depends on the T-lymphocytes, which activate the B-lymphocytes and produce IgE and IgG4.
- The T-cells can suppress the formation of IgE by the production of interferon-gamma (IFN-γ).
- The production of IgE is dependent upon the Th-2 helper cells. At the same time, Th-1 cells will suppress IgE production.
Stages of Type 1 Hypersensitivity Reactions are:
This reaction takes place in two stages:
- First Stage: This is the stage where there is sensitization of the host and formation of IgE Ab, which, once formed, attaches to the receptors on mast cells or basophil.
- Second Stage: This is the stage of reaction or shocking dose in this stage where patients will have histamine effects and called histamine poisoning.
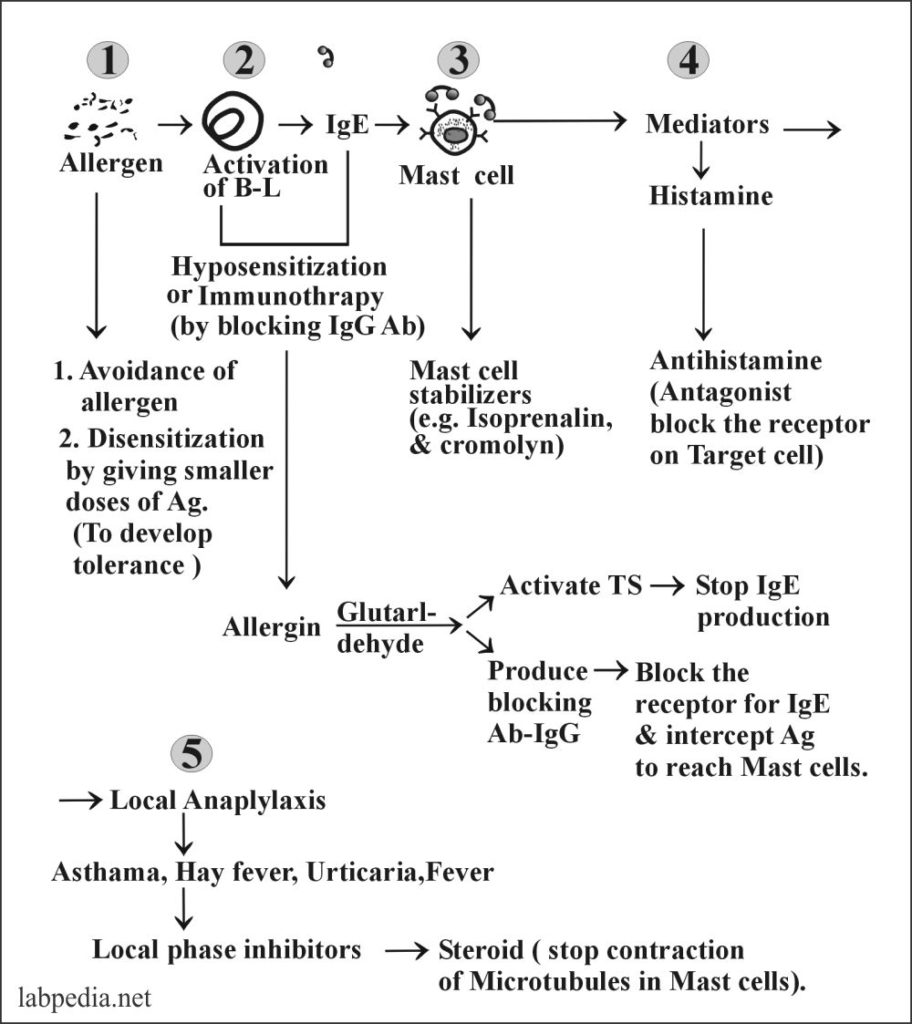
Type 1 reaction has four stages:
- Activation of the B-lymphocytes to produce IgE.
- Antigen and IgE will sensitize mast cells.
- Mast cells release chemical mediators.
- The patient will have S/S like asthma, hay fever, or atopic eczema.
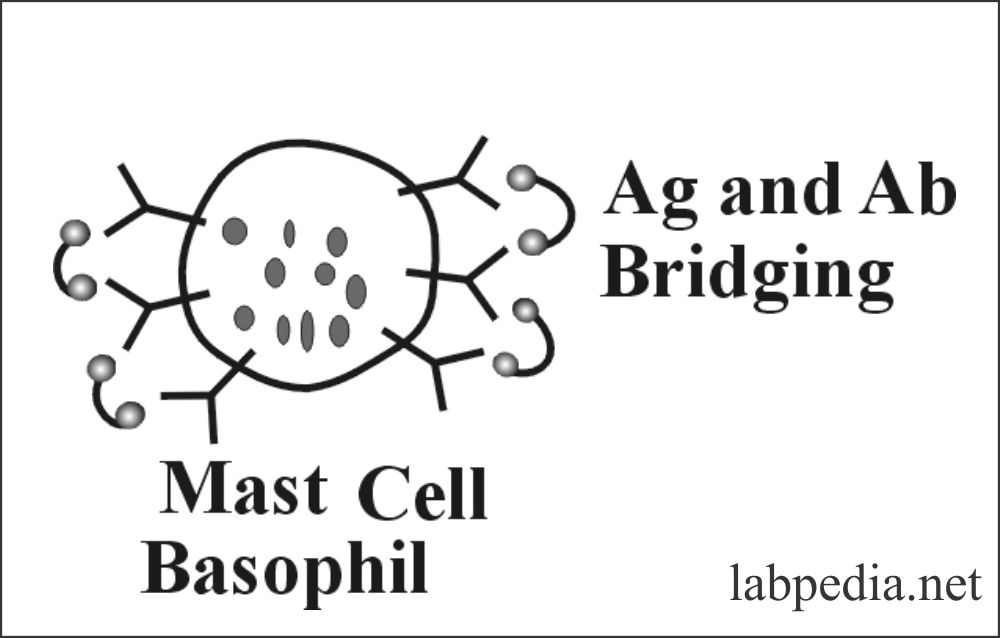
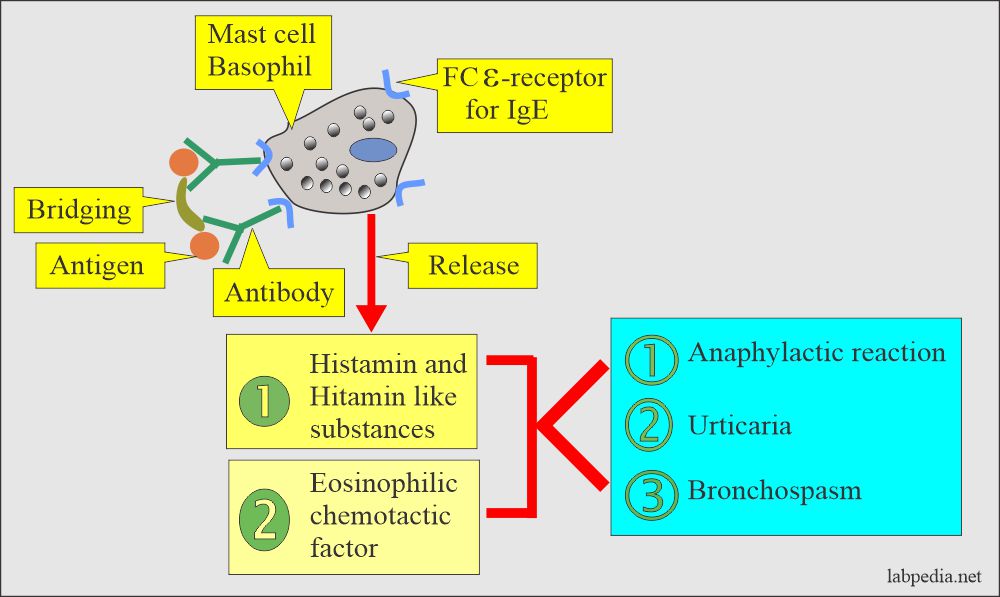
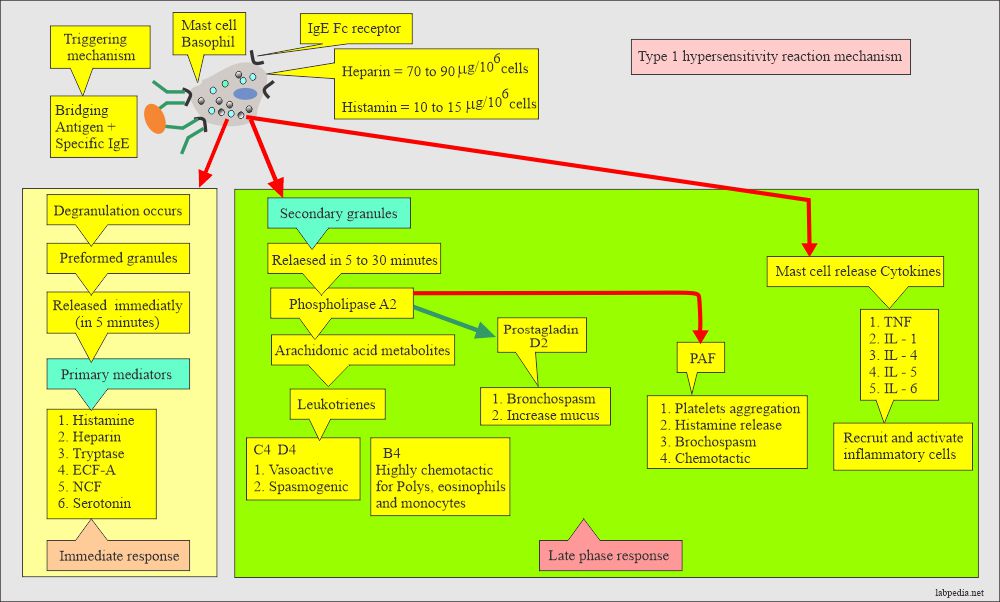
Ag and Ab (Ag +IgE) bridging leads to degranulation, where Ag makes bridging between two IgE-Ab molecules present on the mast cell or basophils.
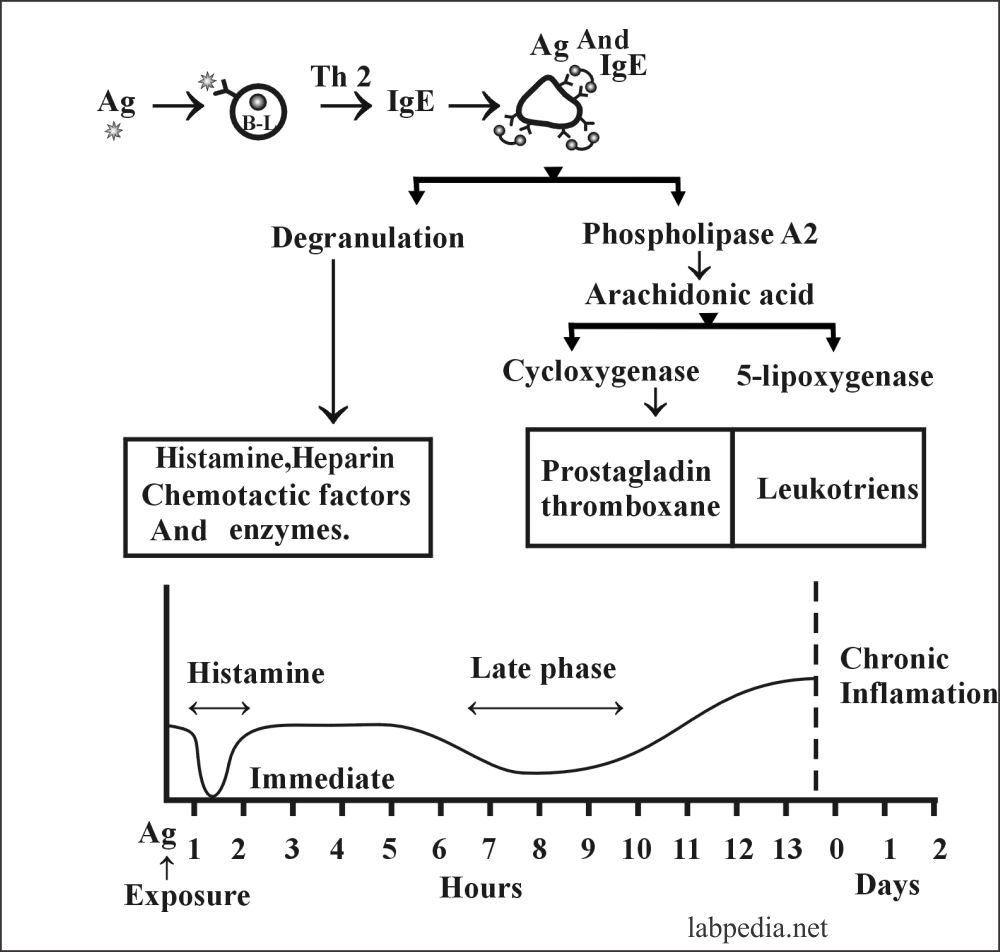
Degranulation is an active process where:
- There is an influx of calcium.
- Initially, there is a rise in cAMP, and later on, it decreases.
Degranulation leads to the release of:
- Primary mediators
- Secondary mediators
- Cytokines
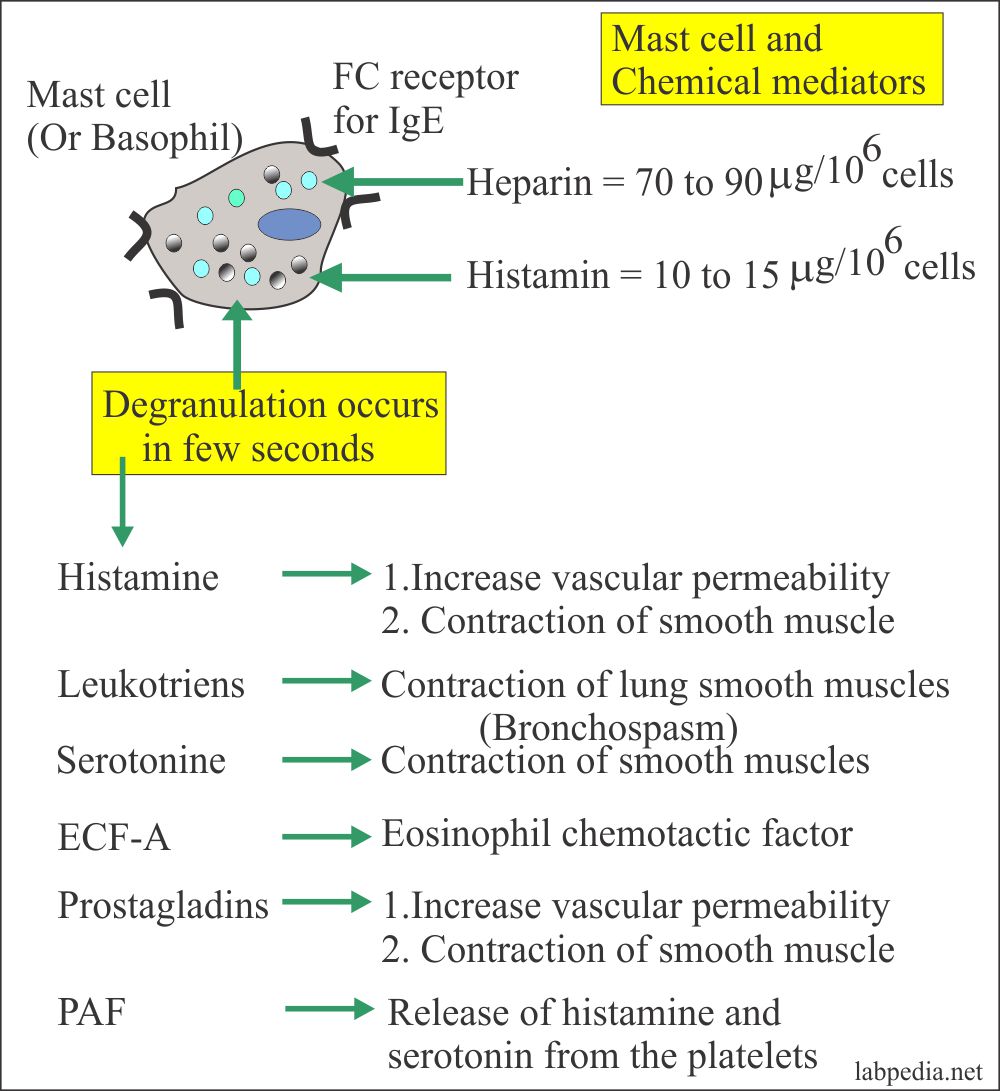
Chemical Mediators of type 1 Hypersensitivity Reaction are:
Primary or Preformed Mediators:
These are as follows:
- Histamine
- ECF-A (Eosinophilic chemotactic factor of anaphylaxis).
- Neutrophil chemotactic factors (NCF).
- Serotonin.
Secondary Mediators (Arachidonic Acid Metabolites):
These are:
- Slow releasing substances of anaphylaxis (SRS-A) and now called leukotrienes, e.g., LTB4, LTC4, LTD4, LTE4.
- Platelet-activating factor (PAF).
- Prostaglandin D2 (PGD2).
Mast Cell Associated Cytokines:
- These cells recruit more inflammatory cells.
- TNFa, IL1, IL3, IL4, IL5, IL6, GM-CSF.
Histamine
It is 10% of the weight of cells. It has the highest level in the morning and the lowest level in the late afternoon.
Histamine acts through separate receptors, and these are named:-
H1 – present in smooth muscles of bronchi, and action stops by the antihistamine.
H2 – Present in the stomach, and action stops by cimetidine.
H3 – Present in CNS. It is under research.
Histamine clinically leads to:-
- Wheal and flare.
- Broncho-constriction.
- Increase mucous secretions.
- Hypotension due to vasodilatation and increased vascular permeability.
- Cardiac arrhythmia.
Histamine target areas show:-
- Skin – edema, and hives.
- Trachea and bronchi due to broncho-constriction lead to asthma and increased mucous secretions.
- Eyes and nose – increase secretion and red eyes.
- Uterus – smooth muscle contraction leads to abortion and pain.
- Gastrointestinal tract. There is nausea, vomiting, abdominal pain, and diarrhea.
Secondary Mediators
- Leukotrienes:
- These are the metabolites of arachidonic acid metabolism. These have the same action as histamine but are more potent and strong, almost several thousand times more active than histamine.
- These are vasoactive and spasmogenic leading to contraction of smooth muscles and increased vascular permeability.
- LTB4 – It is chemotactic for eosinophils, ploys, and monocytes.
- Another leukotriene LTC4 (Previously) is called SRS-A.
- Platelet Activating Factors (PAF)
- It is generated from complex -lipids stored in the cell membrane. It leads to:-
- Platelet aggregation and their lysis lead to histamine release.
- It activates neutrophils and eosinophils.
- It is the most potent eosinophil chemotactic factor.
- Prostaglandin (PGD2)
-
- It is produced by human mast cells and leads to increased secretion, edema, and smooth muscle contraction.
- Bridging antigen and antibody over the surface of mast cell or basophil leads to the release of mediators.
- Type 1 Hypersensitivity reaction depends upon the production of IgE by activating B-L with the help of the Th2 helper cell.
Mediators of the type 1 hypersensitivity reactions are:
| Chemical mediators | Pharmacological action |
| Histamine |
|
| Serotonin | This leads to the contraction of the smooth muscle |
| Prostaglandin |
|
| Platelet-activating factor |
|
| The eosinophilic chemotactic factor of anaphylaxis (ECF-A) |
|
| Leukotrienes |
|
| Basophil kallikrein | It generates the kinins |
Clinically Anaphylactic Reaction may be:
- Localized reaction.
- Systemic reaction.
- Localized Reaction:
- It causes skin allergies (wheel), Hay fever, allergic rhinitis, asthma, atopic conjunctivitis, and urticaria.
- Systemic Anaphylactic Reaction:
- It is a generalized phenomenon and leads to:-
- Pallor, Nausea, vomiting, asthma, laryngeal edema, and Hoarseness.
- Abdominal pain, diarrhea, low blood pressure, and ultimately patient goes into shock (anaphylactic shock).
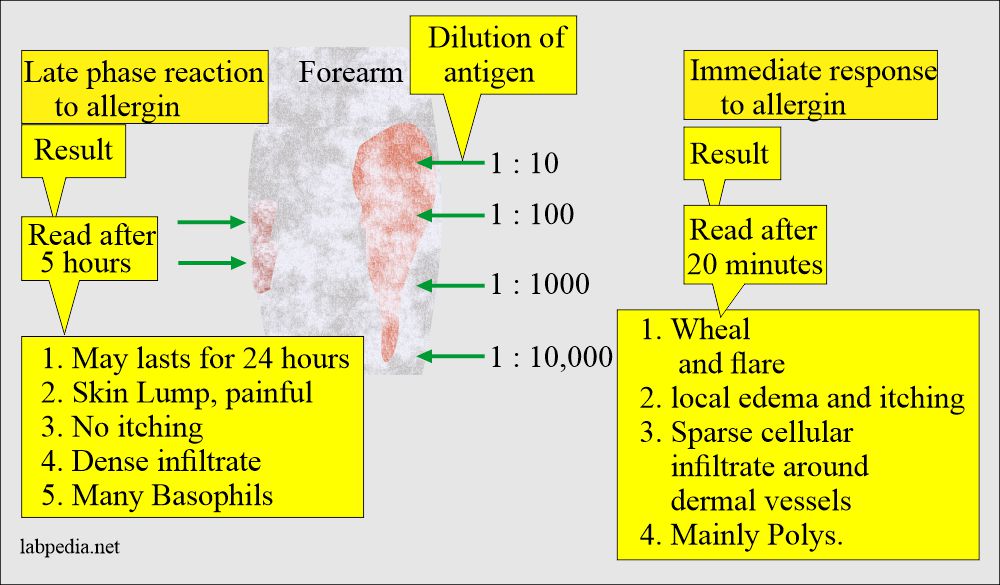
Immediate Reactions:
- It starts within a few seconds to 30 minutes and may subside in 60 minutes.
Late Phase Reaction:
- It starts in 2-8 hours and may last for 2-3 days, and is normally due to secondary mediators and inflammatory cell reaction.
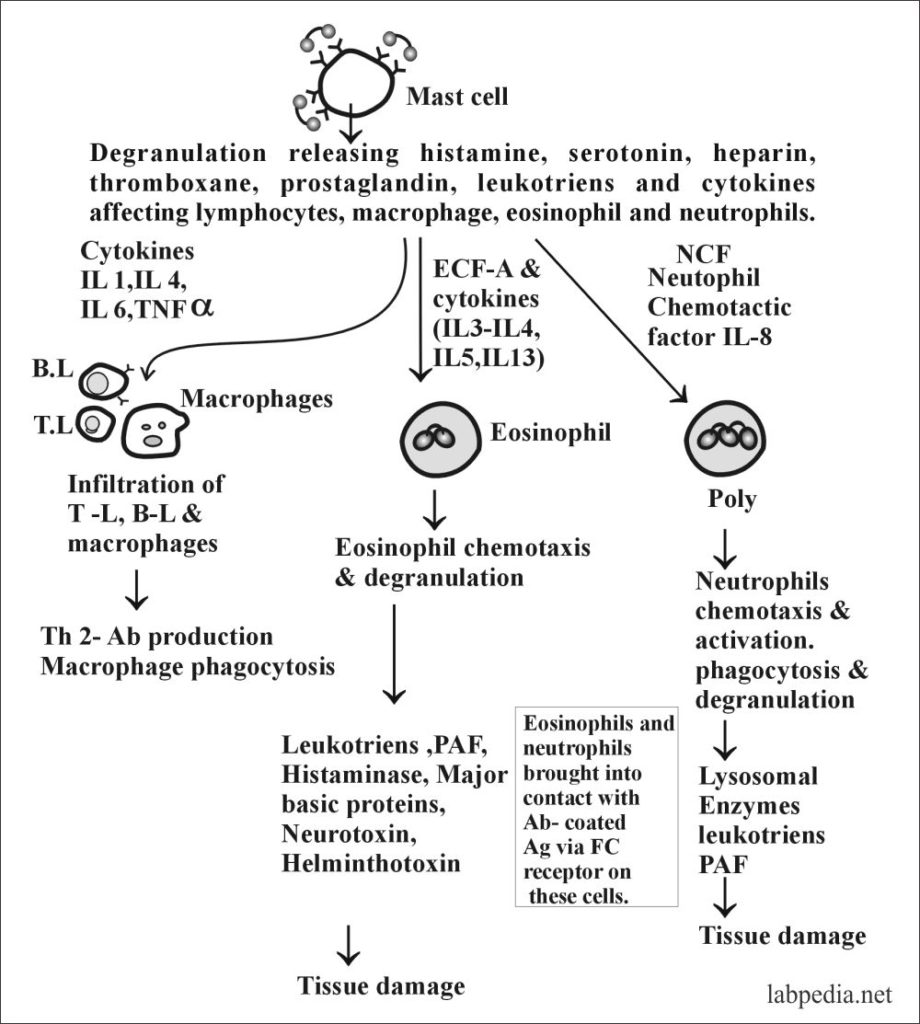
The late Phase:
- It is produced by the activated mast cells, and there is:-
- 1. Profound inflammatory response.
- The cells are attracted to the site and activate other cells like eosinophils, Neutrophils, Basophils, Lymphocytes, and Macrophages.
Clinically types of the type 1 hypersensitivity reaction are:
| Syndrome | Common allergen (Ag) | Route of entry | Response |
| Systemic anaphylaxis | Drugs, serum. Venom | I/V | Edema, vaso-dilatation Asthma. Laryngeal edema, shock, and death |
| Wheal and flare | insect bites, sensitivity testing | Subcutaneous | Local vasodilatation and local edema |
| Allergic Rhinitis and hay fever | Pollen (ragweed), dust, mites, feces | Inhaled | Edema of the nose, irritation of nasal mucosa |
| Bronchial asthma | Pollen dust, mites, and feces | Inhaled | Bronchial constriction, increased mucous and airway inflammation |
| Food allergy | Fish, milk, egg, wheat | Oral | vomiting and diarrhea. pruritis (itching) urticaria (Hives) |
Table XVIII – IgE associated diseases
- In late-phase activation of Mast Cells and its mediators ultimately leading to tissue damage, elaborated as follows:
ATOPY
- Coca and Cooke described this in 1923; the term atopy described clinical features of type 1 hypersensitivity reaction, like asthma, eczema, hay fever, and urticaria in subjects with a family history of similar complaints and showing immediate positive wheal and flare skin reactions to common inhalant allergens.
- It is a Greek word that means out of place. The patients give 50% family history. There is an association with HLA DR2 for ragweed.
- If both parents have a history of allergy, 50% of children will develop an allergy. Even with one of the parents having an allergy, the chances are still 30% in the children.
- 5% of the American population has asthma.
- 10% suffer from Hay fever.
- 1-2% have atopic dermatitis.
- Suppose there is a history of sensitivity to any antigen or allergic disease in a family and present in both parents. In that case, offspring will have 75% if one of the parents is then 50%. If none of these have sensitivity, only 15% will develop atopy.
- The tendency for allergic reactions has a strong heritability, and such a tendency is called Atopy.
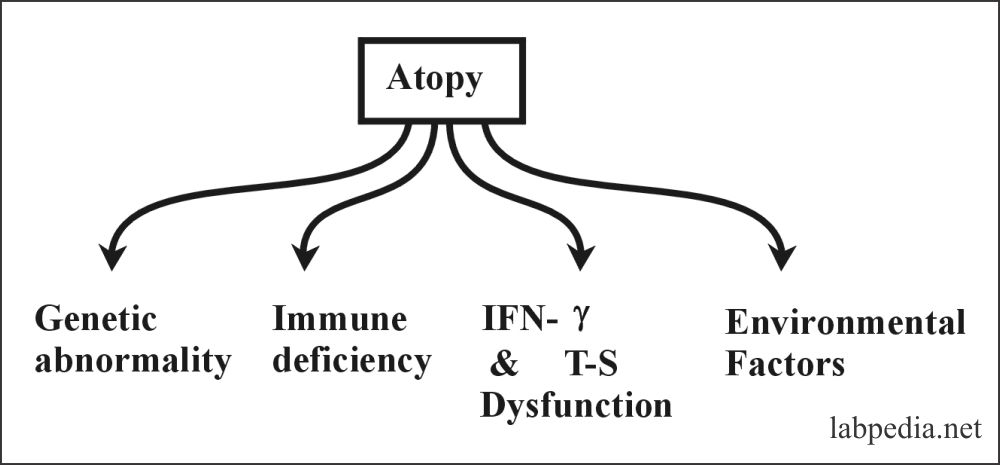
Atopy may be due to:
- Genetic abnormality: One researcher group showed increased IgE response and gene on chromosome II.
- It is seen in immune deficiency diseases like IgA deficiency leading to eczema and asthma.
- A high level of IgE in the cord blood of infants predicts the future development of atopy.
- Immune responsiveness: IFN-γ Production down-regulates IgE production. So when there is a decrease in IFN-γ, there will be an increase in IgE production. Also, there is the role of T-suppressor cells.
- Environmental factors like environmental allergen exposure in fetal life also influence such diseases.
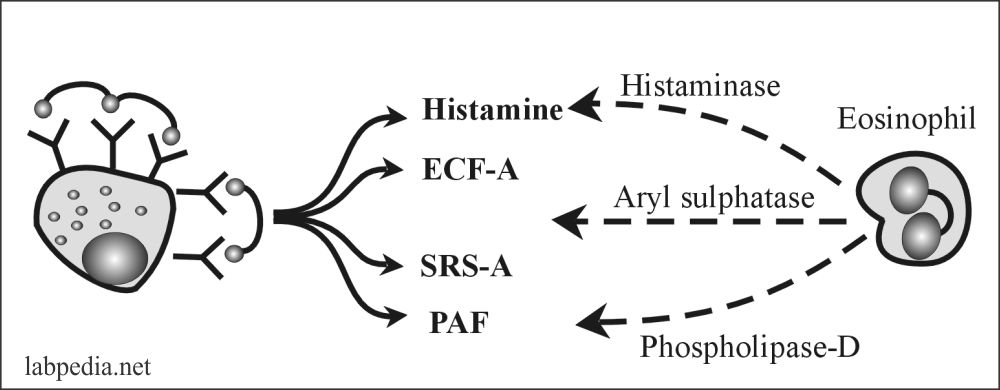
Nature Check Mechanism
Nature has a check mechanism; otherwise, a small dose of Ag might have led to death. There is the production of some enzymes that inactivate the type-I reaction mediators.
- Histaminase = Inactivate histamine
- Aryl sulphatase = Inactivate SRS – A
- Phospholipase D = Inactivate PAF
Diagnosis Type 1 hypersensitivity reaction
The diagnosis may be made by:
- A detailed history of the patient and guesses may be made for the allergen.
- Skin testing with a wide panel of Ag. This is done by injecting Ag subcutaneously or by patch test to see wheal and flare response.
- The antigen is introduced subcutaneously, leading to the release of preformed mediators, which will increase vascular permeability, local edema, and itching.
- The late phase reaction is usually overlooked, and it will show with the appearance of a lump in the skin and is painful rather itchy.
- IgE level:- Total IgE level may be raised in the majority of the patients.
- RAST: – This is a radioallergosorbent test, which detects allergen-specific IgE. It is a costly test and not as good as skin tests.
- Eosinophil Count:-Blood eosinophilia may be found in allergic diseases.
Treatment
Type I reactions can be treated at different stages of reaction. The best treatment is the avoidance of the source (Ag). Treatment is shown diagrammatically with the phases of an allergic reaction.
Hypersensitivity reactions and their summary:
| Hypersensitivity reaction | Type of reaction | Time of development | Type of Antibody | Type of cells involved | Role of complement | Example of the disease |
| Type 1 | IgE dependent reaction | Immediate | IgE | Mast cells | No |
|
| Type II |
|
Immediate | IgG and IgM | Macrophagic cells | Frequently involved |
|
| Type III | Immune-complex mediated reaction | Immediate | IgG and IgM | Neutrophils | Yes |
|
| Type IV | Cell-mediated reaction | Delayed | None |
|
None |
|
Go Back to Elementary Immunology