Antineutrophil cytoplasmic antibody (ANCA), Wegener’s Granulomatosis
Antineutrophil cytoplasmic antibody (ANCA)
Sample for Antineutrophil cytoplasmic antibody (ANCA)
- The patient’s serum is needed.
- How to get good serum: Take 3 to 5 ml of blood in a disposable syringe or a vacutainer. Keep the syringe for 15 to 30 minutes at 37 °C and then centrifuge for 2 to 4 minutes to get the clear serum.
- No special precaution is required.
- Separate the serum as soon as possible and freeze it.
- Slides from the blood are made, and the indirect immunofluorescent technique is performed for the neutrophils.
- Two types of staining patterns were seen for two different antibodies.
Purpose of the test (Indications) for Antineutrophil cytoplasmic antibody (ANCA)
- For the diagnosis of Wegener’s granulomatosis.
- This is also done to follow the course of the disease and monitor the response to treatment of Wegener’s granulomatosis.
- This test may be done for other autoimmune diseases.
- This test is indicated in the case of vasculitis and inflammatory bowel disease.
- This will help diagnose and classify various vasculitis-associated and autoimmune disorders.
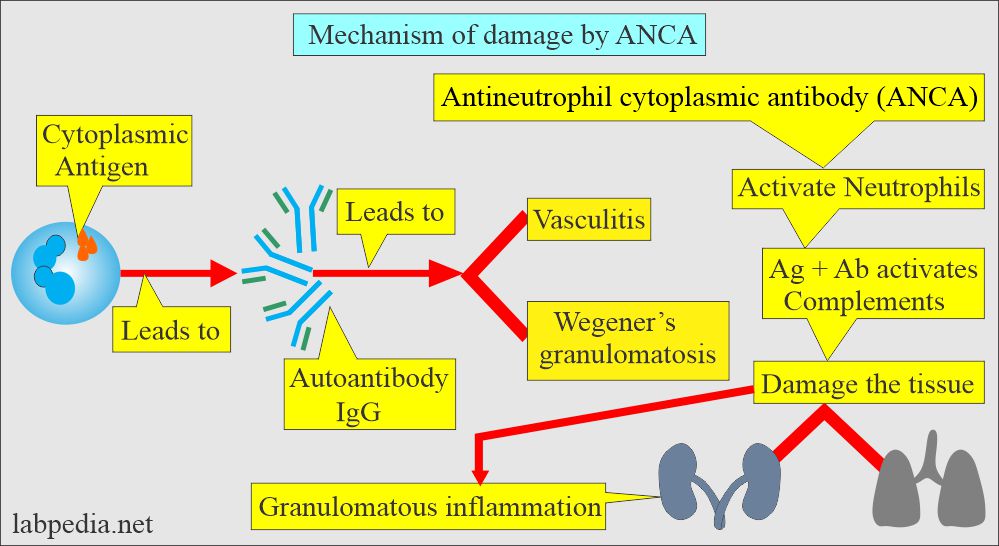
Mechanism of damage by Antineutrophil cytoplasmic antibody (ANCA)
- This is also called an anti-cytoplasmic antibody. These are formed against the antigen in the neutrophils’ cytoplasm and monocytes’ cytoplasm.
- The majority of these are IgG types.
- ANCA activates neutrophils and is followed by the activation of the complement pathway.
- There is damage by vasculitis and accompanied by a chronic inflammatory response.
- Regional vasculitis involves the small arteries of the kidneys, lungs, and upper respiratory tract.
- The pathologic damage is caused by granulomatous inflammation.
- These are autoantibodies against the myeloid-specific lysosomal enzyme.
- ANCA is seen in autoimmune diseases with vasculitis, e.g., Necrotising vasculitis, active Wegener’s granulomatosis, Polyarteritis nodosa, and renal failure.
- These are 85 to 100 % positive in Wegener’s granulomatosis.
Types of Antineutrophil cytoplasmic Antibody (ANCA)
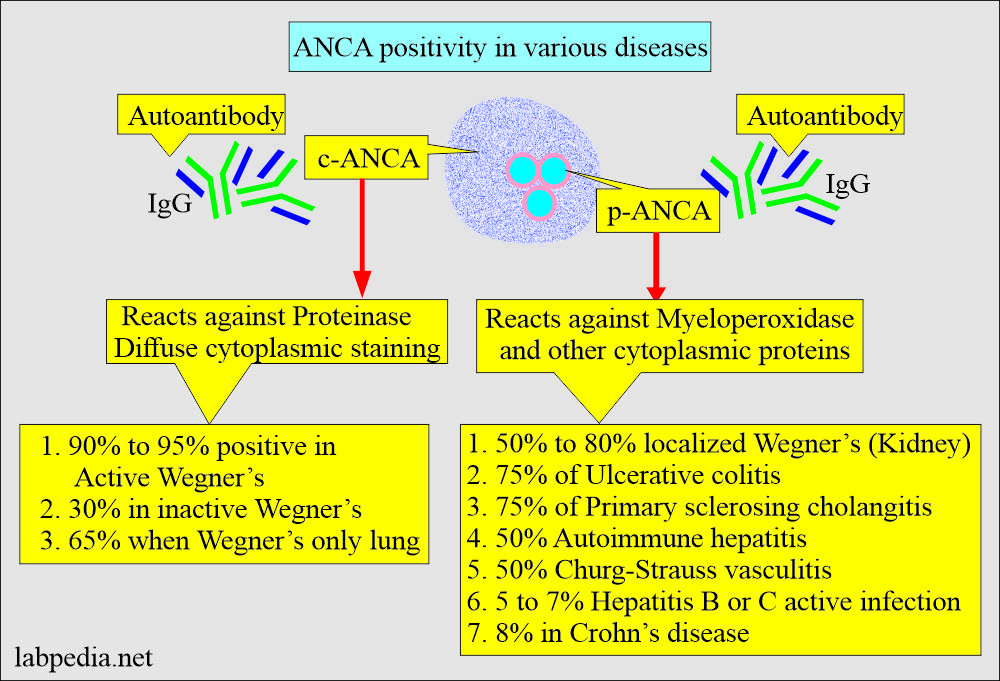
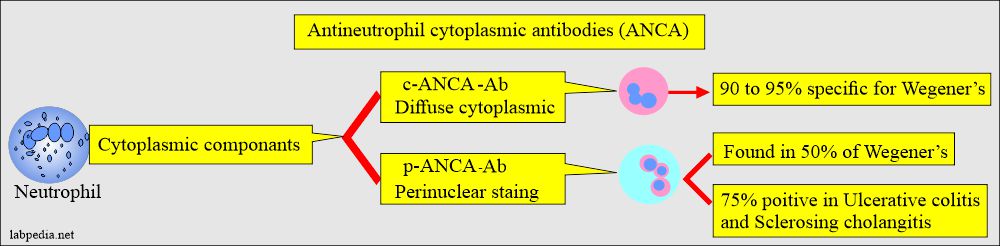
- When patient sera are incubated with alcohol-fixed neutrophils, indirect immunofluorescence shows two patterns:
- c-ANCA(cytoplasmic ANCA):
-
- It is highly specific, 95% to 99% of Wegener’s granulomatosis, and there is diffuse granular staining of the cytoplasm of neutrophils and monocytes (by fluorescent antibody technique ).
- Its sensitivity is >90% in the systemic vasculitis phase.
- It is present in only about 65 % of cases of respiratory disease.
- All of Wegner’s patients with limited disease in the kidney are not positive for c-ANCA (negative c-ANCA).
- When Wegner’s is not active, then percentage drops to 30%.
- A negative result for c-ANCA does not rule out Wegener’s.
- False-positive results are rare.
- A rising titer for c-ANCA suggests relapse.
- When the titer is falling indicates successful treatment.
- p-ANCA(perinuclear ANCA):
-
- It produces a perinuclear pattern of staining in the neutrophil’s cytoplasm.
- It is against various proteins like myeloperoxidase, elastase, and lysozyme.
- It is only seen in the alcohol fixation and not in the formalin.
- A positive result is confirmed by ELIZA,
- This test has poor specificity and 20% to 60% sensitivity in autoimmune diseases.
- It is found in about 50% of patients with kidney disease.
- This is also positive (about 75%) in other autoimmune diseases like Ulcerative colitis or sclerosing cholangitis.
- c-ANCA appears to have anti-proteinase 3 specificity, while p-ANCA has predominantly anti-myeloperoxidase activity.
- Result: Negative when there is very little fluorescence or no fluorescence.
Wegener’s granulomatosis (Granulomatous vasculitis)
Sample for Wegner’s granulomatosis:
- A biopsy of the affected tissue is taken, subjected to culture and special stains to exclude mycobacteria and fungal infections.
- Advise anti-myeloperoxidase antibody.
Definition of Wegener’s Granulomatosis:
- Wegener’s granulomatosis is a rare autoimmune systemic necrotizing or granulomatous vasculitis, mostly affecting the lungs and kidneys.
- Wegner’s granulomatosis is defined as granulomatous inflammation containing foci of vasculitis. Involves the nasopharynx plus proliferative vascular lesion of the kidney.
- A proliferative vascular lesion obliterates a focal area of the Bowman’s capsule of kidneys (crescentic glomerulonephritis).
- There is regional systemic vasculitis or fatal granulomatous vasculitis.
- Small arteries of the kidneys, lungs, and upper respiratory system (nasopharynx) are involved.
- The damage is due to granulomatous inflammation.
- The renal lesion is focal segmental necrotizing glomerulonephritis.
- It is a vasculitis involving small and medium-sized blood vessels in various organs.
- The common sites are the kidneys and respiratory system.
Diagnostic criteria of Wegner’s Granulomatosis:
- Necrotizing granulomas in the respiratory tract.
- Generalized necrotizing arteritis.
- Glomerulonephritis.
Signs and symptoms of Wegner’s Granulomatosis:
- The patient has a fever and arthralgia.
- Nose bleed, epistaxis.
- Stuffy nose, nasal ulceration, and crusty secretions.
- Rhinitis is the first symptom.
- There is sinus involvement.
- Ear shows conductive hearing loss due to auditory dysfunction.
- There are otitis media.
- The kidney shows glomerulitis.
- There is hypertension.
- The oral cavity shows nonspecific mucosal ulceration.
- There is gingivitis.
- Bone destruction and loosening of the teeth.
- Lung shows pulmonary nodules like coin lesions.
- There is an infiltrate looking like pneumonia.
- There is pulmonary hemorrhage leading to hemoptysis.
- Rarely there is bronchial stenosis.
- The skin may show a subcutaneous nodule which is like a granuloma.
- There may be cutaneous vasculitis.
- CNS may show sensory neuropathy.
- Multiple cranial nerve involvement.
- The eye shows Inflammation like:
- Scleritis and conjunctivitis are common.
- There is proptosis or ptosis.
- There are orbital granulomas.
- There is a corneal ulcer.
- There may be scleritis or episcleritis.
- There may be uveitis.
- There may be retinitis.
- Damage to the heart, lungs, and kidneys may be very severe.
- Usually, heart, CNS, and GI tract involvement are rare.
- Histologically there are poorly formed granulomas, with the presence of necrosis and many multinucleated giant cells.
- It is believed that ANCA antibodies are responsible for inflammation.
Lab diagnosis of Wegner’s Granulomatosis:
- Serological method for the detection of ANCA.
- c-ANCA:
- Detection of c-ANCA is sensitive and specific for diagnosing Wegener’s disease.
- Biopsy of the affected area with the fluorescent method shows antibodies localization in the neutrophil cytoplasm, having a granular appearance throughout the cytoplasm (c-ANCA).
- c-ANCA is reported 90% to 95% positivity in Wegner’s granulomatosis (range 84% to 100%).
- In inactive Wegner’s disease, 30% positivity (range is 13% to 41%).
- In the case of only respiratory system involvement is 65% (range is 60% to 85%).
- p-ANCA reacts to myeloperoxidase and is detected in 50% to 80% of the localized Wegner’s granulomatosis involving the kidneys.
- p-ANCA is seen in other diseases as well like;
- Ulcerative colitis (roughly in 75% of the cases).
- Sclerosing cholangitis also shows 75% positivity.
- Autoimmune hepatitis shows 50% positivity.
- HCV and HBV in active diseases show 5% to 7% of the cases.
- Crohn’s disease shows 8% positivity.
- p-ANCA is seen in other diseases as well like;
- A biopsy is more diagnostic.
- There is hematuria, and proteinuria.
- Urine culture is negative.
- WBC count and ESR are raised in active disease.
Normal ANCA
- Serological method
- Not found normally in the serum.
- Negative = <1:20
- ANCA by EIA =
- Negtive = <21 units
- Weak positive = 21 to 30 units
- Positive = >30 units.
Source 4
- Tissue biopsy
- Negative for ANCA by IFA.
- In positive c-ANCA, then the results are titrated.
- In positive p-ACNA, MPO (myeloperoxidase) testing is performed by ELIZA.
- Not all p-ANCA cases are positive for MPO.
Source 2
- Blood = Negative
- ANCA is also found in ulcerative colitis and inflammatory bowel disease.
- Also positive in Crohn’s disease, specifically p-ANCA.
Antineutrophil cytoplasmic antibody (ANCA) Increased in:
- Wegener’s granulomatosis (>90% positive predictive value).
- Polyarteritis nodosa
- Necrotizing vasculitis.
- Inflammatory bowel disease.
- Systemic lupus erythematosus.
- Rheumatoid arthritis.
p-ANCA is not specific, but these are seen in the following:
- Polyarteritis nodosum.
- Primary sclerosing cholangitis.
- Microscopic polyangiitis.
- Ulcerative colitis.
Questions and answers:
Question 1: Which test is specific for Wegener's.
Question 2: What type of antibodies are found in Wegener's.