Haptoglobin (HP), Acute Phase Protein
Haptoglobin (HP)
What Sample is needed for Haptoglobin (HP)?
- A blood sample of the patient is needed. The serum is needed to perform the test.
- Can store for 2 weeks at -20 °C.
What are the indications for Haptoglobin (HP)?
- This test is done to detect intravascular hemolysis.
- It may be advised in acute or chronic inflammation.
What precautions are needed for Haptoglobin (HP)?
- Avoid the hemolyzed sample.
- Estrogen and oral contraceptives lower the haptoglobin value.
- Steroid therapy increases the haptoglobin level.
- Regular vigorous exercise lowers the haptoglobin value.
How will you define Haptoglobin (HP)?
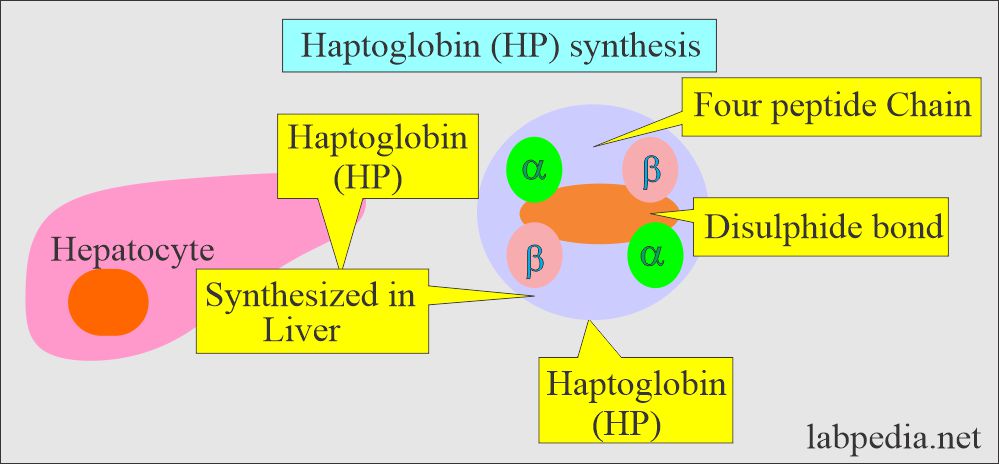
- Haptoglobin is a glycoprotein synthesized in the liver.
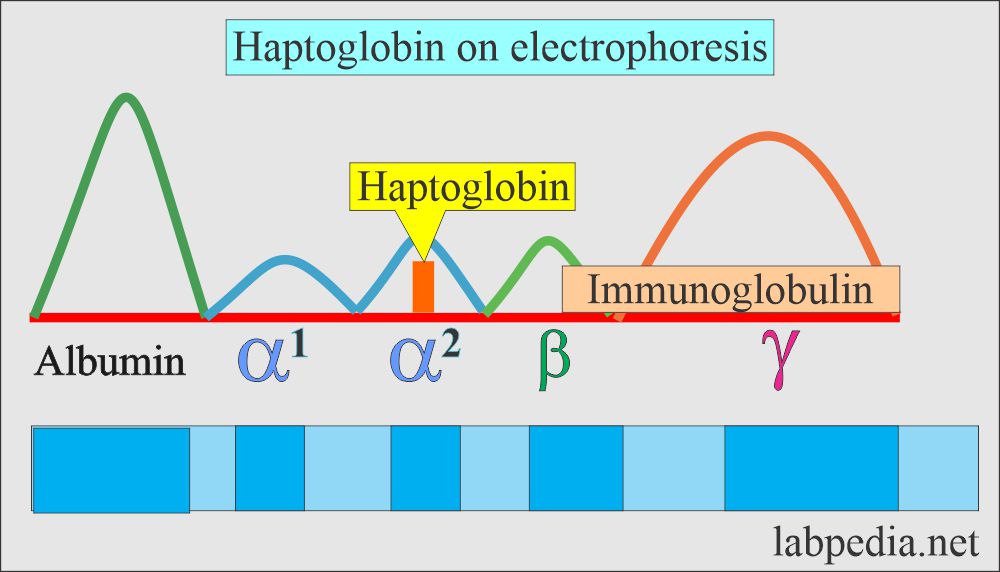
- This is an α-2 glycoprotein (globulin) that binds irreversibly to free hemoglobin released from the intravascular or extravascular destruction of RBCs.
- This is present in the α-2 zone on electrophoresis.
- The α2-globulin band contains haptoglobin, α2-macroglobulin, and ceruloplasmin.
- This is a free Hb-binding protein.
- Haptoglobin, also called transport glycoprotein, is synthesized in the liver. It is a carrier for free hemoglobin in the blood.
- This is present in the α-2 zone on electrophoresis.
What are the characteristic features of Haptoglobin (HP)?
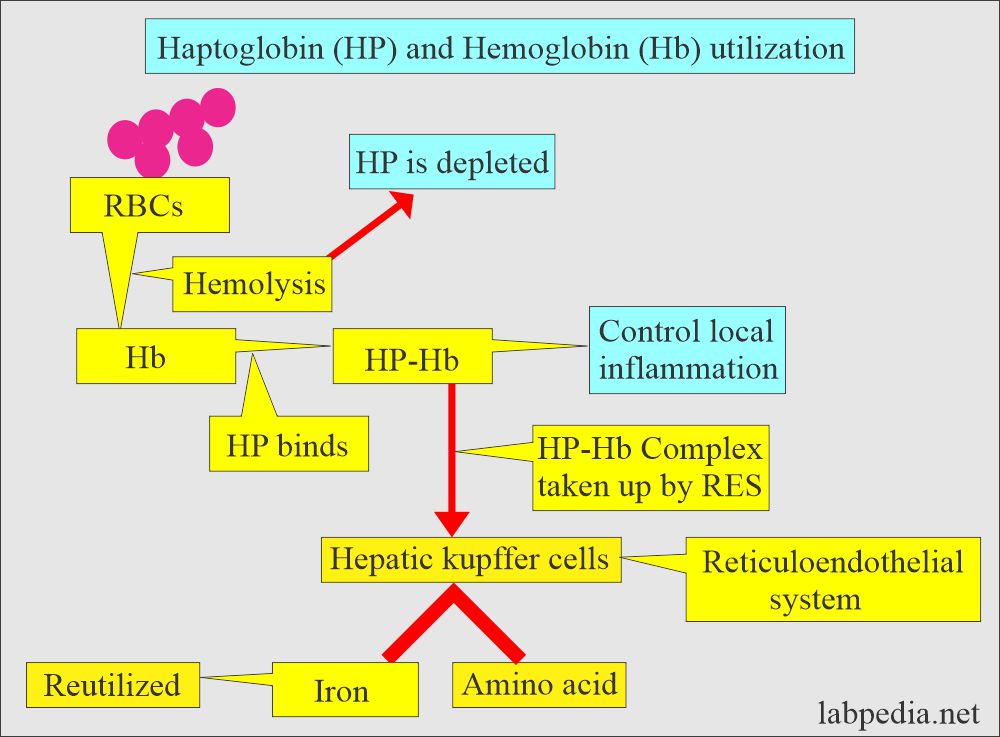
- Transport the free hemoglobin through the blood to the liver for degradation.
- Free hemoglobin is bound to the α-chain of the haptoglobin.
- Haptoglobin increases from the mean value of 0.02 g/L at birth to an adult level within the first year of life.
- It increases with increasing age.
- Methods to measure haptoglobin (HP):
- It is measured by immunologic techniques.
- Total haptoglobin level decreases more slowly than the binding capacity.
- After the hemolysis attack, its level decreases after 6 to 8 hours.
- Haptoglobin-binding capacity:
- It can be measured by electrophoresis or chemical methods.
- HP-binding capacity decreases immediately after the hemolysis or when free hemoglobin is released into the blood circulation and remains low for 2 to 4 days.
- Antihaptoglobulin antibody method.
- It is measured by immunologic techniques.
- Estimation of the haptoglobin for the possibility of hemolysis is controversial.
- Congenital absence of haptoglobin occurs roughly in 3% African Americans and about 1% Europeans.
- 80% to 90% of newborns lack haptoglobin after the first day of birth until they are 1 to 6 months old.
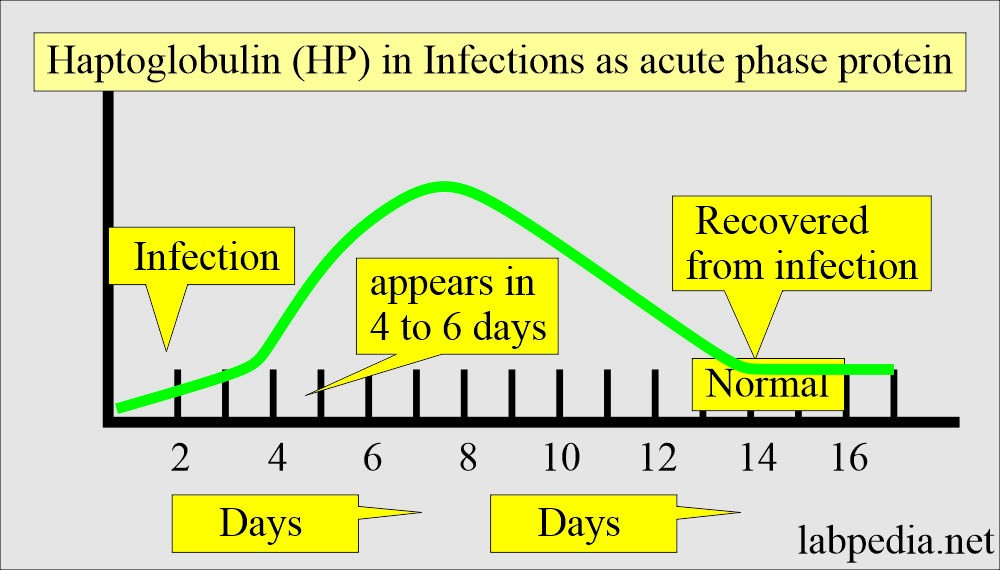
- Haptoglobin is an acute-phase protein, increased in severe infection, acute myocardial infarction, burns, damage to the tissues, and some cancer patients.
Discuss the synthesis of haptoglobin (HP)?
- This is synthesized in the liver and consists of four peptide chains (αβ)2 linked by a disulfide bond.
- One of the references says there are three possible alpha (α) chains and only one β-chain.
- It binds free hemoglobin and is rapidly cleared from the blood in case of intravascular hemolysis.
- In the initial stage of hemolysis, the liver can compensate for the synthesis of HP, so its level is decreased.
What are the functions of haptoglobin (HP)?
- Haptoglobin increases in acute and chronic inflammation.
- Haptoglobin-free and its complex (HP+Hb) are significant in the inflammatory process.
- Haptoglobin is a natural bacteriostatic agent.
- Haptoglobin synthesis is stimulated by inflammation and not by hemolysis.
- It is a natural bacteriostatic agent for iron-requiring bacteria, e.g., E.coli.
- This acute-phase protein increased in ulcerative colitis, acute rheumatic diseases, and heart attacks.
- Haptoglobin’s physiologic function is to preserve the iron in the body.
- Haptoglobin prevents damage to renal tubules by the excreted hemoglobin.
- Haptoglobin binds the hemoglobin and carries that complex to the reticuloendothelial system.
- Haptoglobin (HP) helps differentiate hemolytic anemia from the other causes.
| Clinical condition | Haptoglobin level | Reticulocytes count |
|
|
|
|
|
|
|
|
|
- Haptoglobin depletion is a sensitive marker for hemolysis.
- HP is decreased in hemoglobinuria.
- HP is unchanged in myoglobinuria and rhabdomyolysis because there is no binding with HP.
What is the role of Haptoglobin (HP) as an acute-phase protein?
- Haptoglobin synthesis is increased in acute inflammation, tissue necrosis, and malignancy.
- It increases after 4 to 6 days of the inflammatory process.
- It takes around 2 weeks to become normal after removing the stimulating factor (infection or inflammation).
- The cytokine, especially IL-6, initiates its synthesis.
What is the normal haptoglobin (HP) level?
- Newborn = 5 to 48 mg/dL (50 to 480 mg/L). It may be absent at birth.
- 6 months to 16 years = 25 to 138 mg/dL
- 16 to 60 years = 15 to 200 mg/dL
- >60 years = 35 to 175 mg/dL
- Another source
- Adult = 20 to 220 mg/dL
- Newborn = 0 to 10 mg/dL
- Children = Adult level reach by one year
- Critical value = <40 mg /dL
What are the conditions that lead to increased haptoglobin level + ESR?
- By corticosteroid hormones and nonsteroidal anti-inflammatory drugs.
- In nephrotic syndrome.
- In biliary obstruction in the absence of hepatocellular disease.
- Ulcerative colitis.
- Peptic ulcer.
- Acute rheumatic disease.
- In cancers.
- In acute and chronic inflammatory diseases, it acts as an acute-phase protein.
- In acute myocardial infarction.
- In tissue destruction like burn and cancers.
- Drugs that may increase the level are:
- Steroids.
- Androgens.
What are the conditions for increased haptoglobin (HP) levels?
- Acute and chronic infections or inflammation.
- Tissue destruction.
- Advanced lymphomas.
- Malignant tumors.
- Biliary obstruction.
- Collagen diseases.
What are the conditions for decreased haptoglobin (HP) levels?
- Genetic deficiency.
- In hemolytic anemia.
- Systemic lupus erythematosus
- Erythroblastosis fetalis.
- Estrogen will decrease its synthesis.
- Decreased with severe liver diseases.
- A slight decrease in blood transfusion, even in the compatible blood transfusion, is due to a few RBC hemolysis.
- This may be decreased in hematoma because of the binding of Hb with HP.
- Drugs that may decrease the level are:
- Chlorpromazine.
- Isoniazid.
- Oral contraceptives.
- Streptomycin.
- Quinidine.
- Nitrofurantoin.
- What is the critical value?
- It is <40 mg/dL.
Questions and answers:
Question 1: What is the role of haptoglobin?
Question 2: What is the role of haptoglobin for RBC?