Immunoglobulin A (IgA), Indications and Functions
Immunoglobulin A (IgA)
What sample is needed for Immunoglobulin A (IgA)?
- The patient’s serum is needed to estimate IgA.
- A random sample can be taken.
- Analyzed a fresh sample or stored it at 4 °C for less than 72 hours. Stable for 6 months at -20 °C.
- Avoid lipemic or hemolyzed serum.
What are the indications for Immunoglobulin A (IgA)?
- IgA level is advised in the case of suspected deficiency.
- In case of repeated infections of the sinuses, respiratory system, and GIT.
What factors will influence the result?
- Drugs that will increase the values are:
- Hydralazine.
- Phenytoin.
- Isoniazid (INH).
- Procainamide.
- Tetanus toxin and toxoid.
- Therapeutic gamma globulins.
How will you discuss the pathophysiology of Immunoglobulin A (IgA)?
- IgA is the second most common Ig, and it has two subclasses:
- IgA 1
- IgA2
- It has two categories:
- Secretory IgA.
- Monomer IgA.
- IgA monomer is present in high concentrations in human serum (90 to 450 mg/dL or 55 to 270 IU/L).
- It is 15% to 20% of the total Ig.
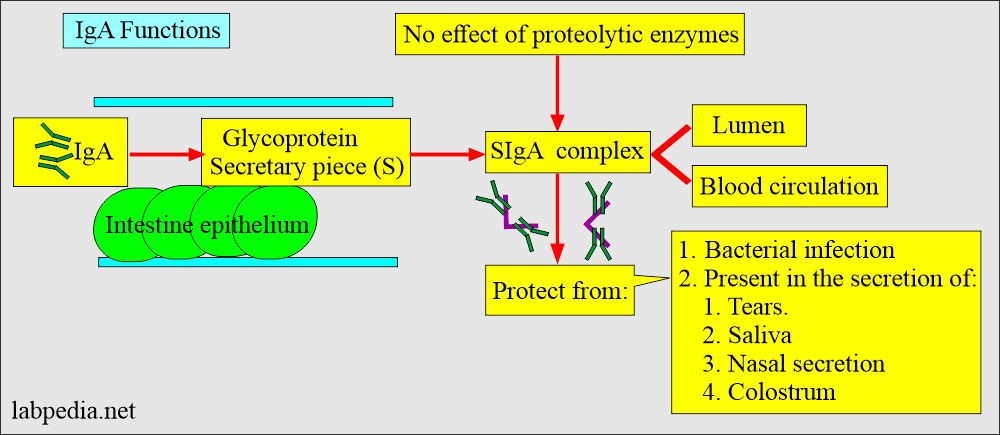
- IgA is the predominant immunoglobulin in the secretion of tears, saliva, colostrum, milk, and intestinal secretions.
- It has a half-life of 6 days.
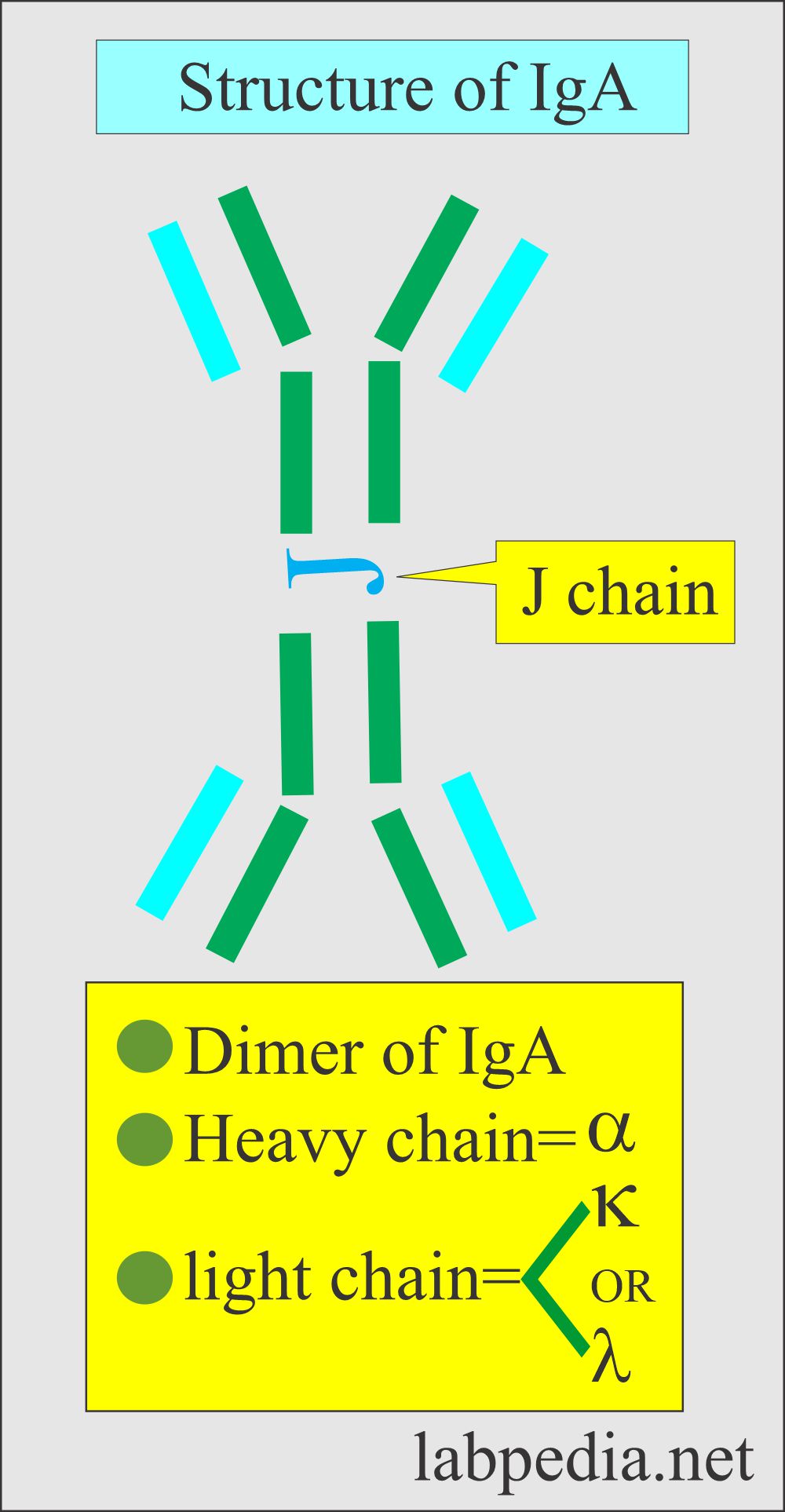
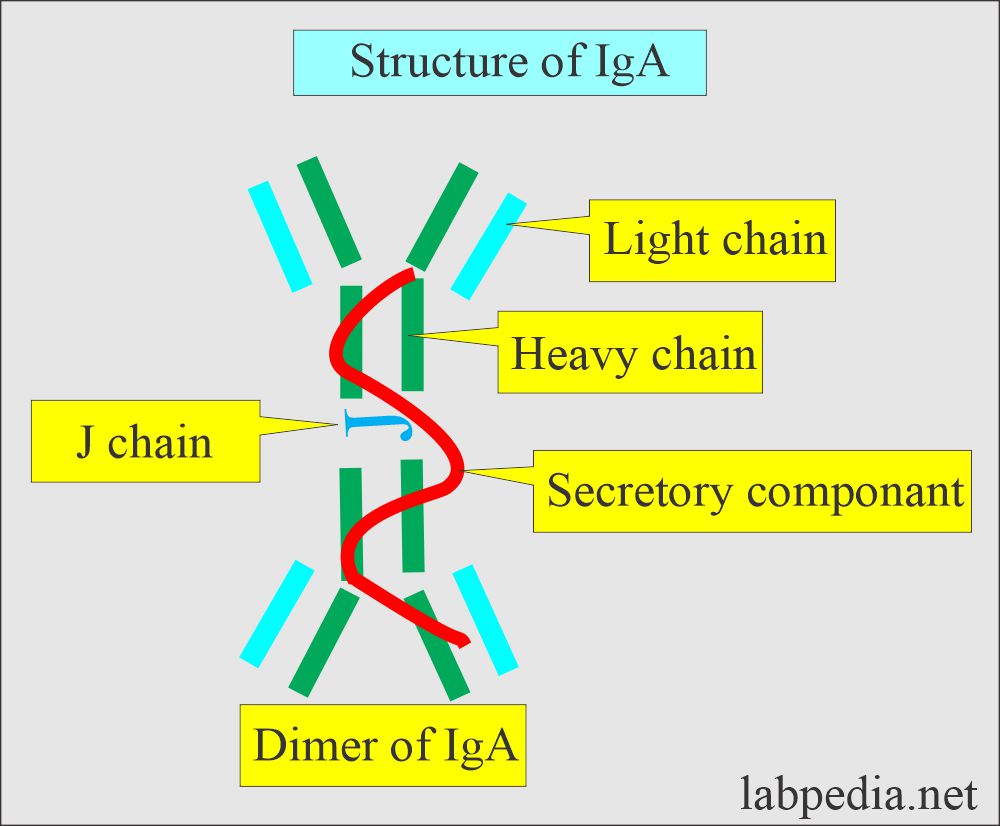
- It has paired kappa (κ) or lambda (λ) chains,
- Two heavy chains.
- IgA consists of two monomers joined by J-chain and secretory fragments.
- IgA monomer form is found in high concentrations in the serum (90 to 450 mg/dL in a normal adult).
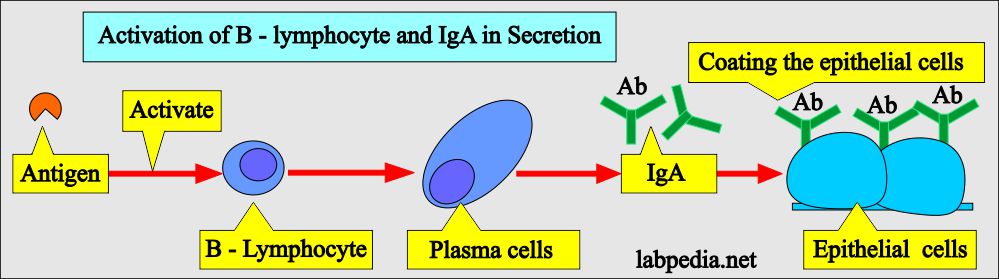
- IgA antibodies are produced by the plasma cells.
- The plasma cells are derived from activated B-B-lymphocytes.
- The presence of IgA secretion is present In:
- IgA antibodies are found in the digestive system, respiratory system, colostrum, milk, nose, eyes, and vagina.
- IgA is also found in saliva, tears, and blood.
- IgA antibodies are found in the digestive system, respiratory system, colostrum, milk, nose, eyes, and vagina.
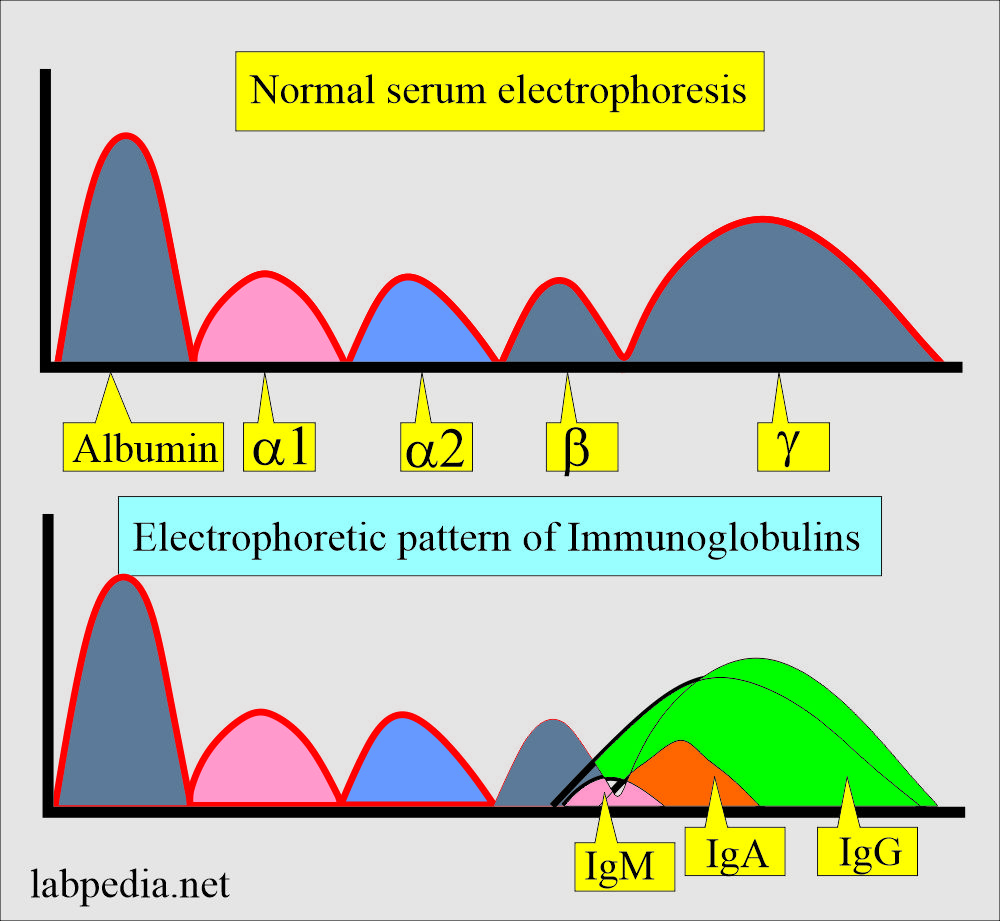
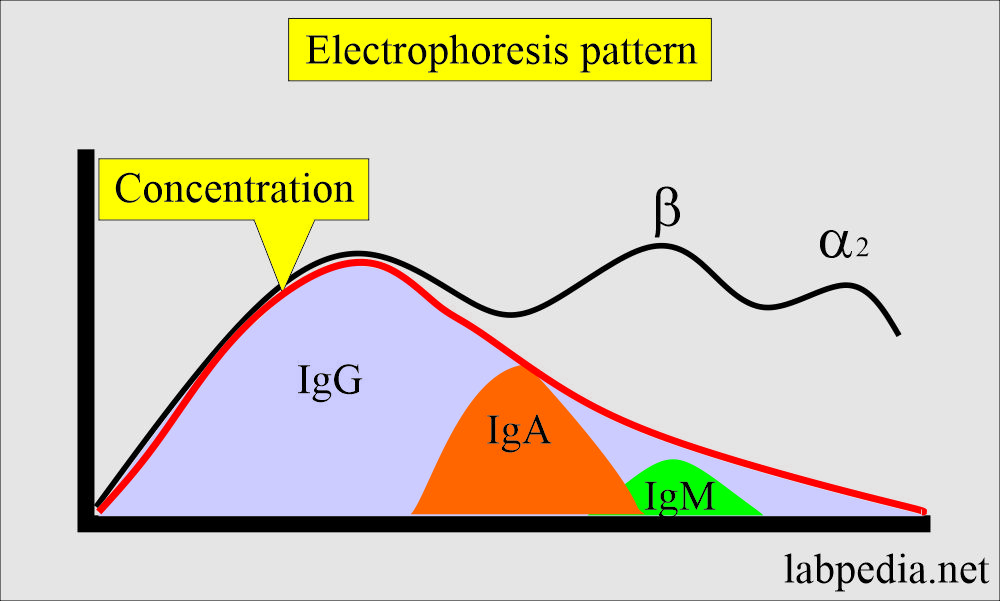
- Immunoglobulins are present in the γ and β-region on the electrophoresis.
- IgG migrates in the area between the β-region and γ-region.
- IgA migrates in the pregamma region and some portion in the γ-region.
- IgM is also present in the pregama and γ-region.
- The average adult level is attained by the age of 16 years.
- IgA concentration is > 1mg/dL, and CSF contains 0.1 to 0.6 mg/dL.
What is the normal structure of IgA?
- IgA consists of a dimer structure.
- There is a J-chain that joins the two molecules of immunoglobulins.
- Also, there is a secretory piece.
What are the Functions of Immunoglobulin A (IgA)?
- IgA antibodies’ main function is to protect the mucosa exposed to various antigens.
- It can activate complement by alternative pathways.
- It is an effective opsonin.
- The secretory IgA consists of two 4- 4-basic chain units (dimeric form) joined by the J-chain.
- IgA secretory components are very important in protecting the mucous membrane.
- Its importance in secretion is to protect from the microorganisms like tears, saliva, nasal fluids, and colostrum.
- The deficiency of IgA leads to infection of the gastrointestinal and respiratory systems.
- It has antiviral activity.
- Its major role is protecting against bacteria, viruses, and protozoal infections by preventing their attachment and colonization of the mucosa.
What is the Normal level of Immunoglobulin A (IgA)?
Source 1
| Age | mg/dL |
| Cord serum | 1 to 4 |
| one month | 2 to 50 |
| 2 to 5 month | 4 to 80 |
| 6 to 9 month | 8 to 80 |
| 10 to 12 month | 15 to 90 |
| one year | 15 to 110 |
| 2 to 3 year | 18 to 150 |
| 4 to 5 year | 25 to 160 |
| 6 to 8 year | 35 to 200 |
| 9 to 12 year | 45 to 250 |
| >12 year | 40 to 350 |
- To convert into SI unit x 10 = mg/L
Source 2
- Adult = 85 to 385 mg/dL
- Children = 1 to 350 mg/dL
Another source
- 0 to <5 months = 7.0 to 37.0 mg/dL
- 15 to <24 months = 36 to 79 mg/dL
- 2 to <4 years = 27 to 246 mg/dL
- 10 to <13 years = 42 to 295 mg/dL
- 16 to <18 years = 60 to 337 mg/dL
- more than 18 years = 61 to 356 mg/dL
What are the conditions with increased Immunoglobulin A (IgA) levels?
- Multiple Myeloma
- Cirrhosis of liver
- Systemic lupus erythematosus
- Rheumatoid arthritis
- Sarcoidosis
- Wiskott-Aldrich syndrome
What are the conditions with decreased levels of Immunoglobulin A (IgA)?
- Hereditary telangiectasia
- Type 111 dysgammaglobulinemia
- Malabsorption in some cases
- Occasional cases of Cirrhosis of the liver.
- Occasional cases of SLE
- Occasional cases of Still’s disease
- Occasional cases of recurrent otitis media
- In Agammaglobulinemia
- Hereditary thymic aplasia
- Waldenstrom macroglobulinemia
- Non-IgA myeloma
- Acquired immune deficiency syndrome (AIDS)
Question 1: What is the function of the IgA.
Question 2: What are the types of IgA.
Question 3: What is the half-life of IgA.