Eosinophil Count (Absolute Eosinophil Count)
Eosinophil Count
What Sample is needed for Eosinophil Count?
- Whole blood (EDTA) is needed.
- Heparinized blood can also be used.
- The absolute count should be done within 4 hours, or refrigerate the sample, but do count within 24 hours.
What are the Indications for Eosinophil Count?
- An eosinophil count is done to diagnose allergic conditions.
- To diagnose parasite infestation and its severity.
- This can be used to monitor the treatment of parasites.
What Factors affect the eosinophil count?
- The daily eosinophil count is lowest in the morning. Then, there is a rise from noon until midnight (repeat eosinophil counts each day simultaneously).
- There is a decreased count in stress, burns, postoperative state, labor, and electroshock.
- Eosinophils decrease after the administration of corticosteroids.
How will you define absolute Eosinophil Count?
- Absolute eosinophil count is a blood test that measures one type of blood cell called eosinophils.
- Eosinophiluria is defined when urinary eosinophils are >1% as eosinophils.
- Eosinophils are of two types:
- Eosinophils in peripheral blood smear.
- Tissue eosinophils. Eosinophils migrate to bronchial mucosa, skin, GIT, and vagina in about 12 days.
What are important facts about Eosinophils?
- Hypereosinophilic syndrome is diagnosed if the eosinophil count is elevated >1.5 x 109/L for over 6 months and is associated with tissue damage.
- Persistent eosinophilia with eosinophilic infiltration leads to tissue damage and organ dysfunction.
- The heart valves, skin, and lungs may be affected.
- These diseases are usually treated with steroids or cytotoxic drugs.
- If a clonal cytogenetic abnormality is present in the bone marrow, it is called chronic eosinophilic leukemia.
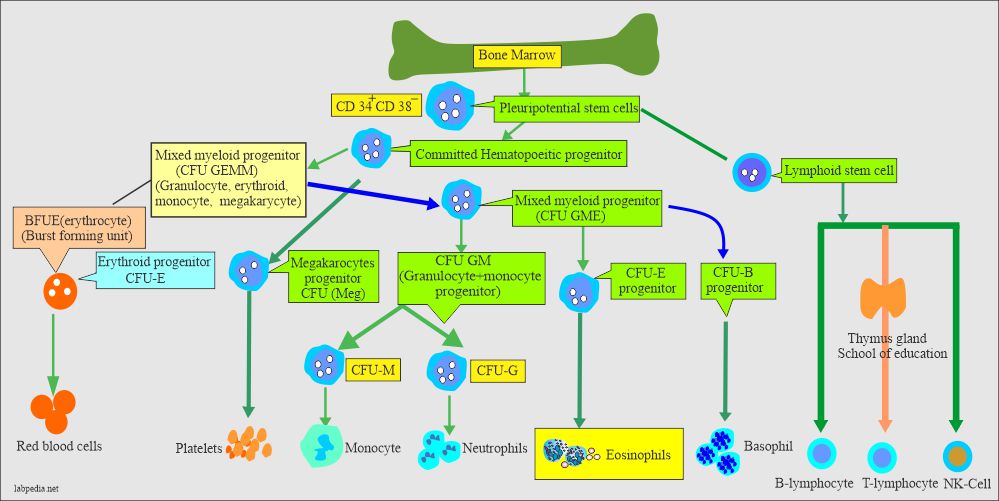
How will you describe eosinophil development?
- Eosinophils have the same stages of maturation as other white cells, like myelocytes, metamyelocytes, band forms, and segmented stages.
- The eosinophils develop from the stem cells in the bone marrow.
- Myeloid series cells mature under the influence of granulocyte colony-stimulating factor (G-CSF).
- Eosinophils take 3 to 6 days in the bone marrow for maturation before they appear in the peripheral blood.
- Bone marrow provides a storage area for eosinophils to be released whenever needed.
- The mean transit time in the circulatory blood system is 8 hours, but in some diseases, it is longer.
- Eosinophils migrate from the blood to tissue after about 8 hours, like bronchial mucosa, skin, gastrointestinal tract, and vagina, for about 12 hours.
- Eosinophils are motile and can migrate between endothelial cells into a tissue or an area of inflammation like neutrophils.
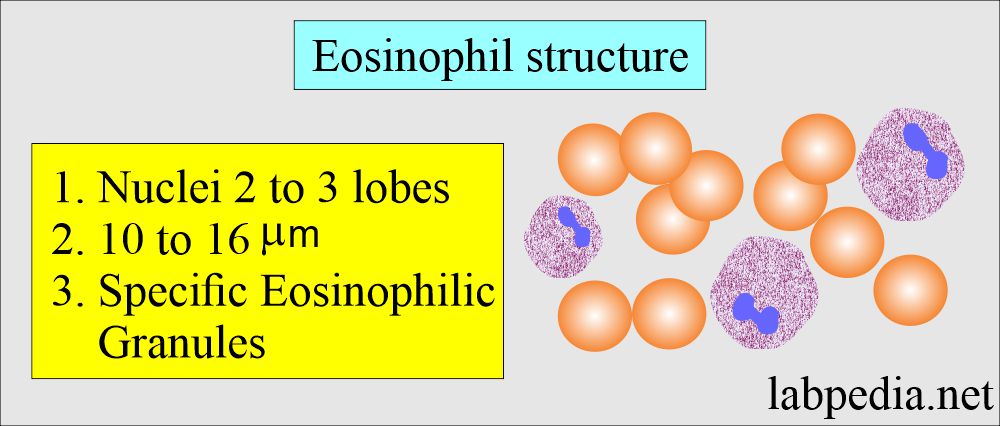
What is the structure of eosinophils?
- Eosinophils are slightly larger than neutrophils. Cell size 10 to 16 µm in diameter.
- The nucleus has two to three lobes. The N: C ratio is 1:1. The nucleus is central or eccentric. The nuclear chromatin is deep-blue purple and coarsely granular chromatin.
- The nuclei have two lobes and occasionally three.
- There are no nucleoli.
- The cytoplasm contains red, uniform, specific eosinophilic granules and occasional vacuoles.
- Eosinophils are like neutrophils, except the cytoplasm contains orange or red staining granules.
- The blood transient time for the eosinophils is longer than for the neutrophils.
- There is a diurnal variation of eosinophil count.
- The lowest count will be in the morning, from 10 AM to 12 AM, and the highest at midnight (4 am).
- The specific granules of eosinophils contain:
- Major basic proteins.
- Peroxidase.
- Perforins.
- Membrane damaging substances.
Name the Eosinophil’s granules?
These are hydrolytic enzymes:
- Peroxidase.
- Acid phosphatase.
- Aryl sulphatase.
- β-glucuronidase.
- Phospholipase.
- Cathepsin.
- Ribonuclease.
But eosinophils lack:
- Cationic proteins.
- Lysosomes.
- Alkaline phosphatase.
What are the functions of Eosinophils?
- The eosinophils can act as phagocytic cells.
- Eosinophils are mainly present in the skin, gastrointestinal tract, and lungs which are involved in hypersensitivity reactions (Type 1) like asthma, hay fever, and eczema.
- Eosinophils are active in antigen-antibody complexes.
- Eosinophils are rich in histamine granules.
- Eosinophils take part in hypersensitivity reaction type 1.
- It helps in the detoxification process.
- A special role in the allergic reaction.
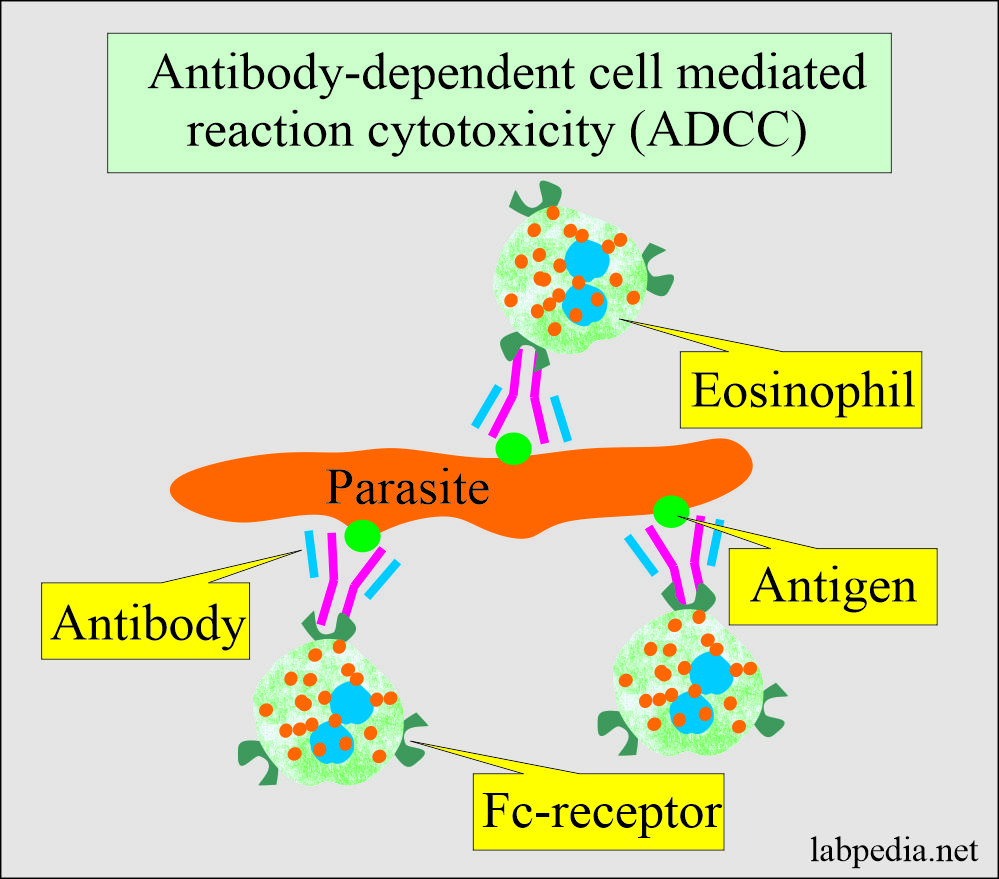
- They are defensive against parasitic infestation. There is the production of IgG and IgE antibodies.
- Eosinophils bind to the antibody-coated parasites and release cytotoxic substances that damage the parasites’ surface, destroying them.
- Antibody-dependent cell-mediated cytotoxicity by eosinophils is effective against parasites in the tissue. This immune response protects from schistosomiasis, hookworms, Ascaris, Fasciola, and Toxocara.
- Eosinophils remove the fibrin during the inflammation,
- With the help of the IgE antibody, Eosinophils can produce histamine from the mast cells or the basophils.
- Eosinophils contain substances that inactivate histamine and factors released during an anaphylactic reaction.
How will you count Eosinophils?
- 1. The best method to count eosinophils is an automated analyzer.
Dunger’s solution:
- This will use an acid dye like eosin.
- Water may be used to lyse the RBC when the eosinophils resist water.
Phloxine stain: It consists of:
- Phloxine 0.1% solution to water 10 mL.
- Distilled water 40 mL.
- Propylene glycol 50 mL.
- Sodium carbonate 1% 1 mL.
What is the procedure for Eosinophil Count?
- A blood sample is diluted in the WBC pipette as 1: 20 dilutions with staining fluids.
- Mix well for 30 seconds.
- Leave the chamber for at least 10 minutes to count the cells.
- Now, fill the chamber and count the colored eosinophils.
What is the normal Eosinophil Count in blood?
Source 2
- Absolute value = 50 to 400 cells/cmm
- Peripheral blood smear (DLC) = 1% to 5%.
- Normal bone marrow = 0% to 3%.
Source 4
- Absolute count = 0% to 0.7 x 109/L
- Differential count = 0% to 3% of total WBC
What are the conditions when Eosinophils are Increased?
- When eosinophils are more than 5% or >500 cells/cmm.
- Allergic disorders:
- Bronchial asthma.
- Angioneurotic edema.
- Hay fever.
- Drug sensitivity.
- Food sensitivity.
- Graft-versus-host disease.
- Bacterial infection in some conditions may be associated with eosinophilia like:
- Scarlet fever.
- Brucellosis.
- Skin diseases:
- Eczema
- Exfoliative dermatitis.
- Pemphigus.
- Psoriasis.
- Urticaria.
- Angioedema.
- Atopic dermatitis.
- Parasitic infestations:
- Especially those parasites that invade the tissue. e.g., Trichinosis, Echinococcus, amoebiasis, hookworm, tape-worm, and ascariasis.
- Hematological disorders:
- Chronic myeloid leukemia.
- Polycythemia vera.
- Pernicious anemia.
- Hodgkin’s lymphoma.
- Hypereosinophilic syndrome:
- Eosinophilic leukemia.
- Trichinosis invasion.
- Dermatitis herpetiformis.
- Idiopathic.
- Malignant tumors:
- Especially with metastasis and necrosis.
- Hodgkin’s disease.
- Clonal T-cell disorders.
- Myeloproliferative diseases include systemic mastocytosis.
- Pulmonary syndromes:
- Eosinophilic pneumonia.
- Tropical pulmonary eosinophilia.
- Loeffler’s syndrome (transient pulmonary infiltrates).
- Allergic granulomatosis.
- Miscellaneous:
- Loeffler’s syndrome.
- Tropical eosinophilia.
- Radiation.
- Rheumatoid arthritis.
- Tuberculosis.
- Sarcoidosis.
- Certain poison.
Hypereosinophilic syndrome:
- Hypereosinophilic syndrome is diagnosed if the eosinophil count is elevated >1.5 x 109/L for over 6 months and is associated with tissue damage.
- The heart valves, skin, and lungs may be affected.
- The treatment is usually steroids or cytotoxic drugs.
- Idiopathic.
- Eosinophilic leukemia.
- Chronic eosinophilic leukemia is a clonal cytogenetic abnormality in the bone marrow.
- Dermatitis herpetiformis.
- Trichinosis invasion.
How will you define Eosinopenia?
- When < 50/cmm is seen in the following conditions:
- Cushing’s syndrome (<50/cmm)
- Due to some drugs like ACTH, epinephrine, thyroxine, and prostaglandin.
- In the shift to the left, there are immature cells.
When can you see Eosinophilic myelocytes?
- These are found in leukemia or leukemoid blood smear.
Questions and answers:
Question 1: How will you define eosinopenia?
Question 2: How eosinophils destroy parasites?