Bilirubin:- Part 1 – Bilirubin (Direct and Indirect), Classification of Jaundice
Bilirubin (Direct and Indirect)
What sample is needed for serum Bilirubin?
- This test is performed on the patient’s serum.
- A random sample can be taken, and no need for a fasting sample.
- Fasting samples may be advised to avoid lipemic serum.
- For infants, the blood may be collected from the heel.
- The sample is stable at 4 °C for 3 days when protected from light.
What are the precautions for the estimation of Total Bilirubin (Indirect/direct)?
- Avoid hemolysis.
- Avoid shaking the tube, which may lead to inaccurate results.
- Do not expose the tube to light. Exposure to light, such as sunlight or artificial light, may decrease the value.
- If there is a delay in the test, keep the sample away from the light (artificial or sunlight) and refrigerate it.
- The sensitivity to light is temperature-dependent; for optimal storage, keep the sample in a colored bottle and at a low temperature.
What are the Indications for Total Bilirubin (Direct and Indirect Bilirubin)?
- For the diagnosis of jaundice.
- To differentiate between different types of jaundice.
- For the follow-up of a patient with jaundice, the treatment is.
- To assess the progress of the disease.
- This test is done to evaluate liver function.
- This is done in patients with hemolytic anemia in adults.
- It is also done to evaluate hemolytic anemia in newborns.
How will you define Total Bilirubin (Direct and Indirect Bilirubin)?
- Bilirubin is the orange-yellow pigment derived from the catabolism of hemoglobin (Heme).
- The majority of bilirubin comes from old red blood cells (RBCs).
- Bilirubin is the basic end product of Hemoglobin metabolism.
- Bilirubin is the end product of heme degradation.
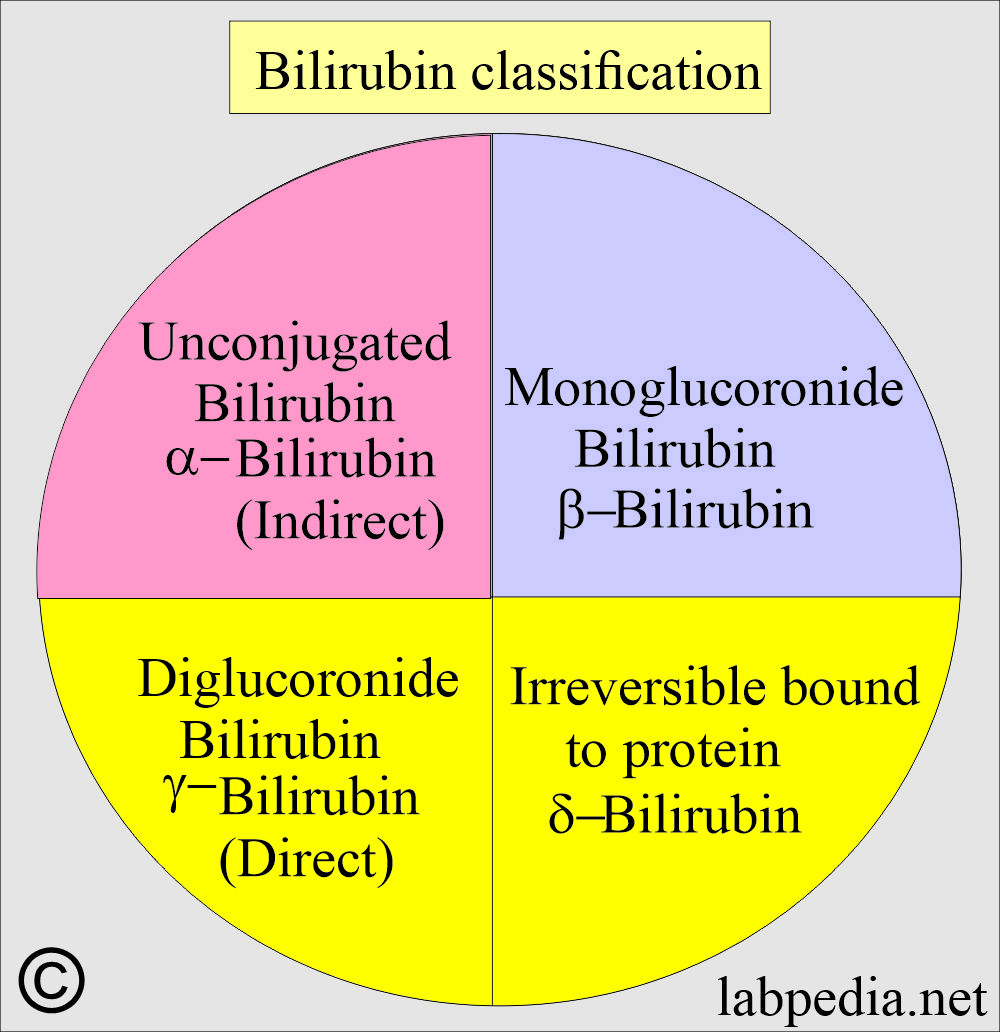
- In circulation, there are 4 types (fractions) of bilirubin:
- Unconjugated bilirubin is also called indirect bilirubin or α-bilirubin.
- Monoglucuronide (monoconjugated) bilirubin, also called β-bilirubin.
- Diglucoronide bilirubin (diconjugated), also called direct bilirubin or γ-bilirubin.
- A fraction of the bilirubin is irreversibly bound to the protein called δ-bilirubin.
- Raised Bilirubin is an indicator of liver dysfunction.
What are the sources of the bilirubin?
- Most of the daily bilirubin production is from senescent red blood cells.
- 1 to 2 x 108 RBCs are destroyed per hour in the human body.
- An average person weighing 70 kg will have a daily turnover of approximately 6 grams of hemoglobin.
- 1 gram of the hemoglobin = 35 mg of bilirubin.
- The total daily production of bilirubin is 250 to 300 mg/day.
- The rest is derived from hepatic hemoproteins and the immature destruction of RBCs in the bone marrow.
- Heme-containing proteins are the non-RBC sources, such as myoglobin, cytochrome, catalase, and peroxidase.
| Source of the bilirubin | Type of bilirubin | Amount in blood |
| Red blood cells (Old RBCS) | Indirect (Unconjugated) | 80% to 85% |
| Ineffective erythropoiesis | Indirect (Unconjugated) | It is variable |
| Heme proteins | Indirect (Unconjugated) | 15% to 20% |
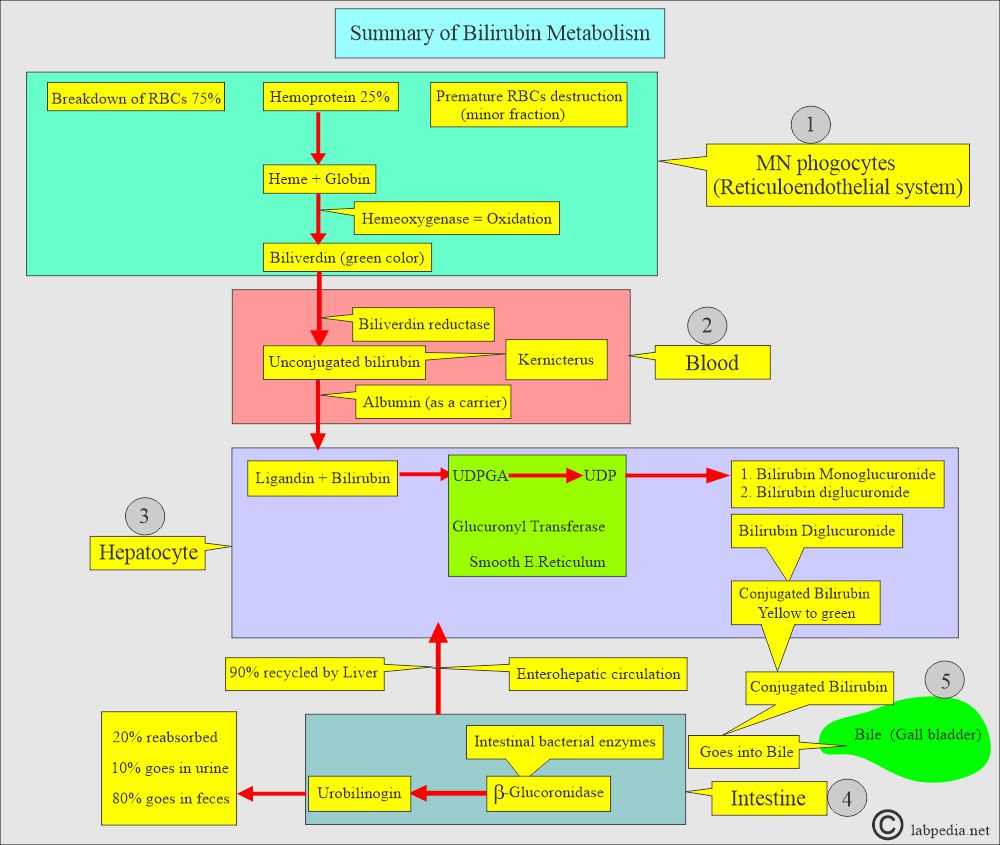
How will you discuss the metabolism of the bilirubin?
- The Bilirubin metabolism can be described in three stages:
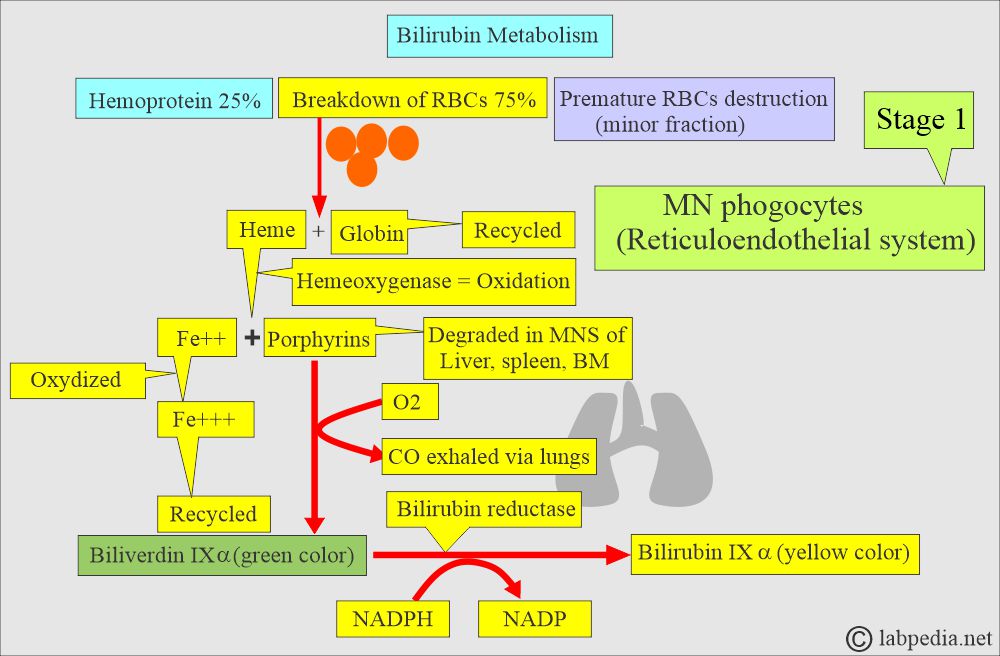
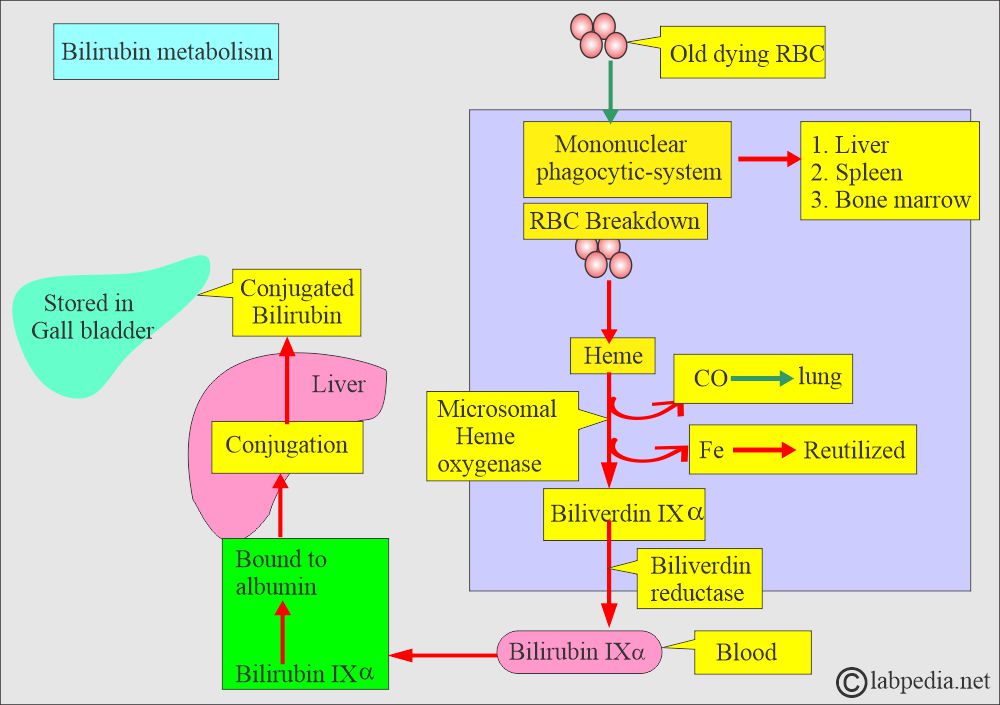
- The first stage is RBCs’ breakdown, forming heme and biliverdin, bilirubin IXα by the mononuclear phagocytic system.
- The second stage is the conjugation of bilirubin, which occurs in the hepatocytes.
- The third stage involves the secretion of bile into the gallbladder and the intestine.
| Stages of Bilirubin formation | Basic mechanism |
|
|
|
|
|
|
The first stage:
What will happen in the first stage?
- Bilirubin metabolism takes place in the mononuclear phagocytic system.
- Hemoglobin from RBCs is released, giving rise to Heme and Globin.
- Heme from the RBC gives rise to protoporphyrins.
- Now, protoporphyrins by microsomal heme oxygenase form Biliverdin IXα.
- Biliverdin reductase enzyme transforms it into bilirubin IXα.
- Globin is degraded into its components, such as amino acids, and then reused or recycled.
- The microsomal heme-oxygenase enzyme degrades heme into iron (Fe++), which is then oxidized to the Fe+++ form and reutilized.
- Under the influence of the above enzyme, iron-free porphyrins are formed.
- An O2 molecule is added, which leads to CO formation, which is then exhaled through the lungs.
- The biliverdin IX-α (green color) is formed under the action of the bilirubin reductase enzyme.
- The heme is reduced by NADPH to NADP and forms the bilirubin IX-α (yellow pigment).
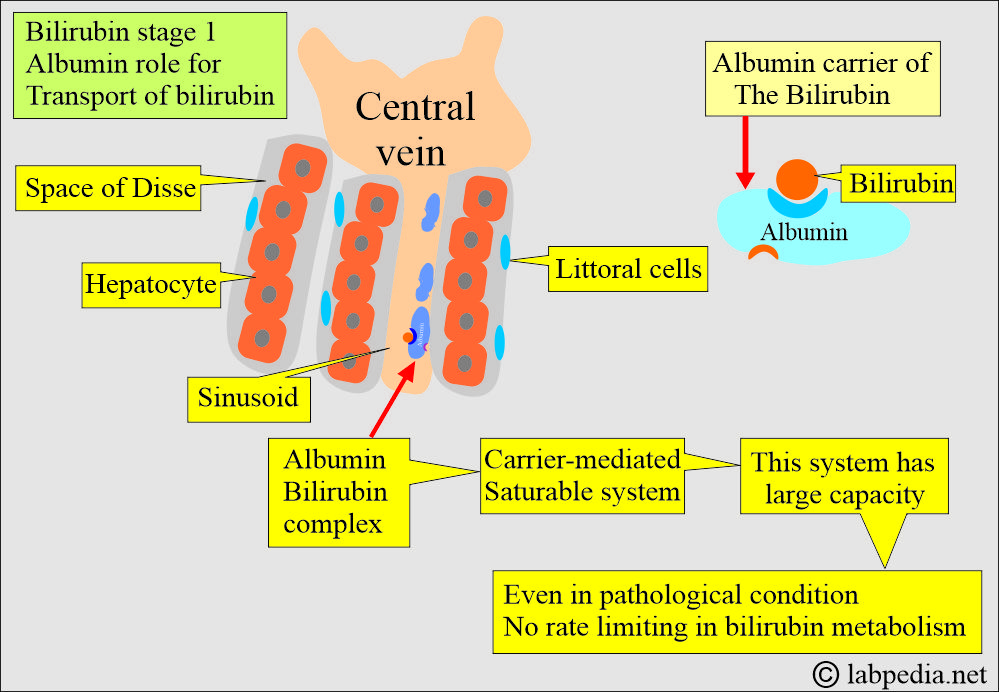
- The plasma albumin takes this unconjugated bilirubin to the liver. Albumin acts as the carrier protein.
- Albumin delivers bilirubin into the hepatocytes and returns to the blood circulation.
- Unconjugated bilirubin (indirect bilirubin) is not water-soluble but is fat-soluble.
- This unconjugated bilirubin combines with albumin, which serves as the carrier protein that transports the bilirubin to the hepatocytes.
- Its solubility increases when it combines with albumin (noncovalent binding to the albumin).
Albumin as a carrier:
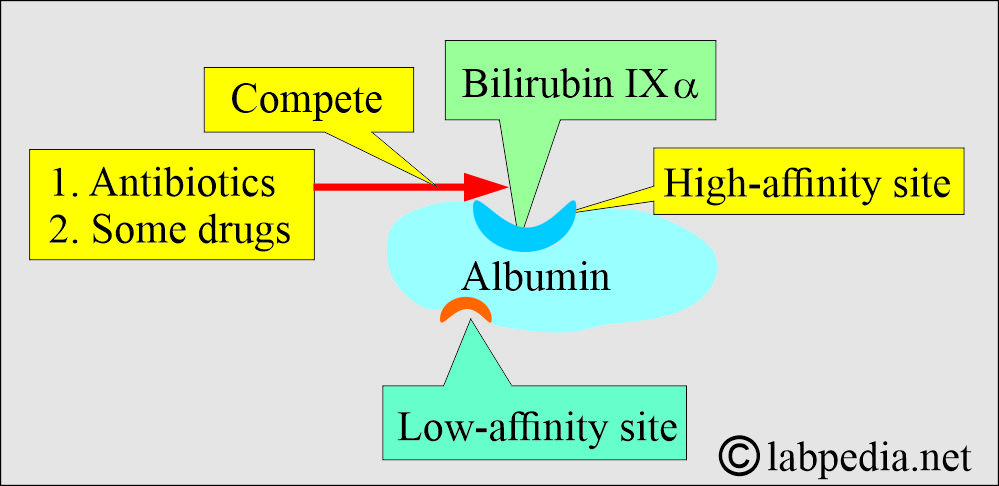
- Albumin has one high-affinity site and one low-affinity site for bilirubin.
- In 100 ml of the plasma:
- Around 25 mg of the bilirubin combines with a high-affinity site.
- An excess of the bilirubin combined with a low-affinity site is easily detachable.
- Antibiotics and some drugs compete with bilirubin for high-affinity sites.
- Bilirubin bound to the high-affinity site on albumin is carried to the liver.
- Bilirubin is removed from the albumin by the hepatocytes’ sinusoidal side by a carrier-mediated, saturable system in the liver.
- This facilitated transport system has an enormous capacity, even in pathological conditions.
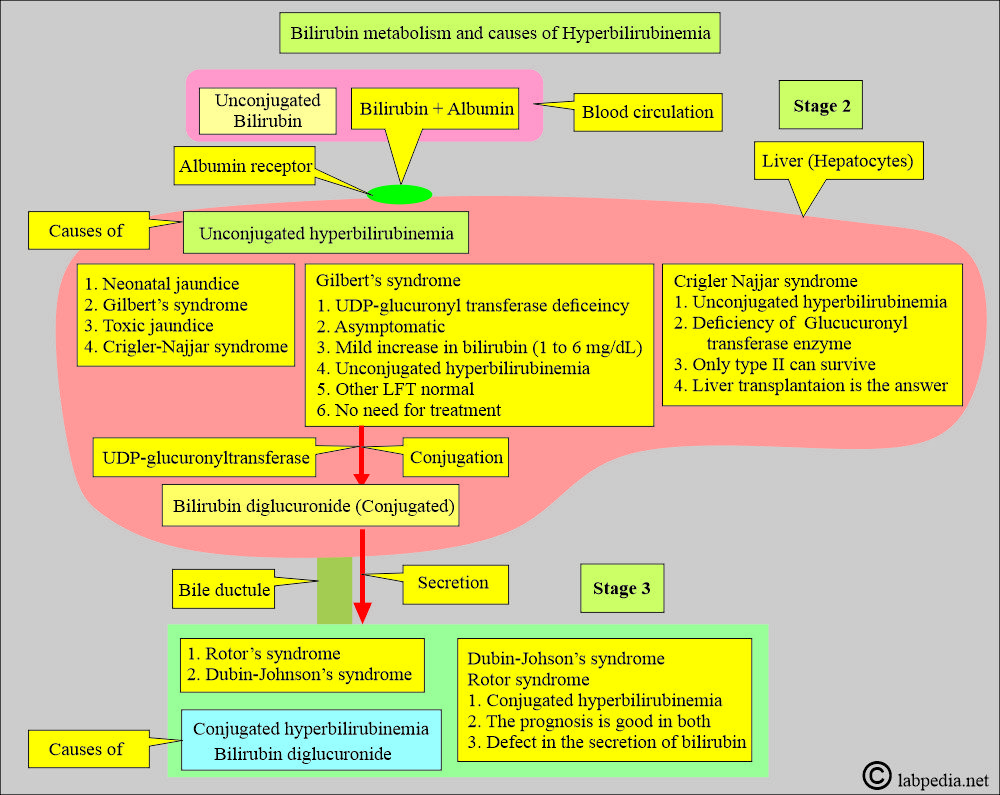
Second stage:
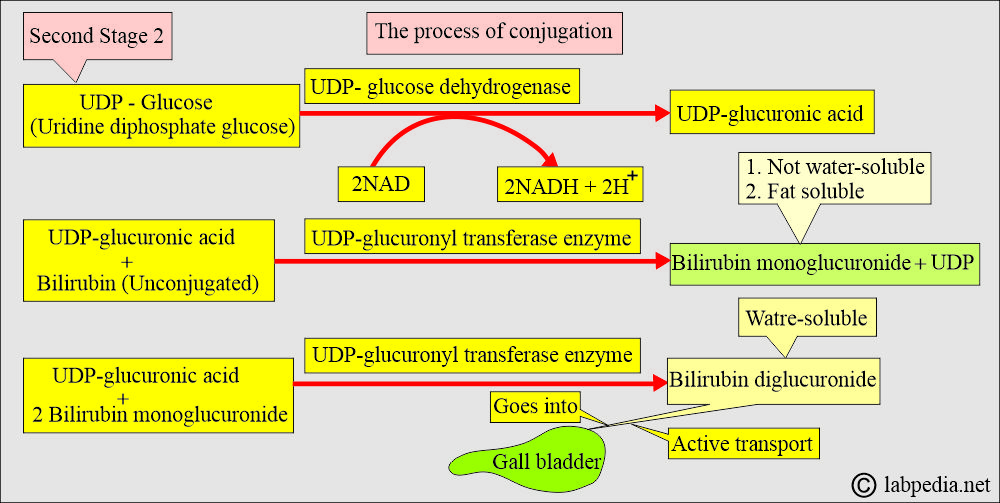
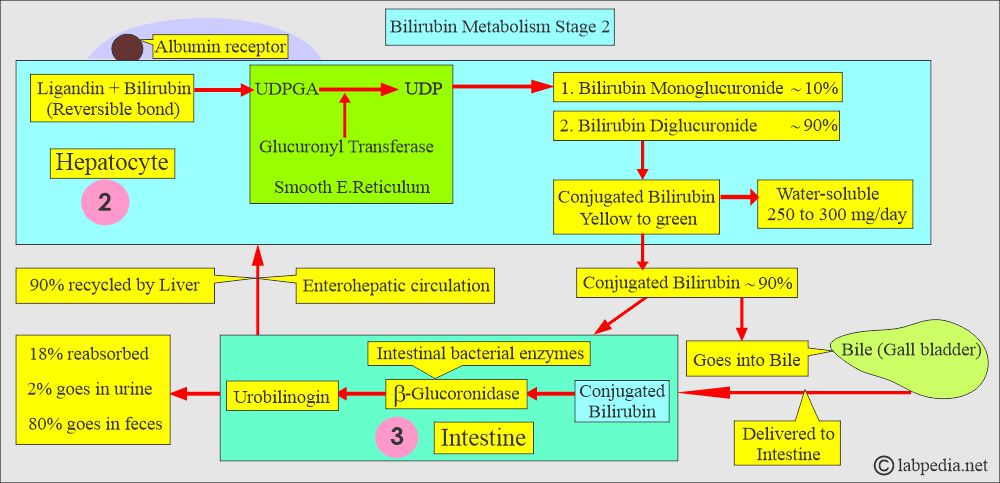
- The second stage is the conjugation process in the hepatocytes:
- Bilirubin is nonpolar and is bound to the lipids in the cells.
- The bilirubin conjugation occurs in the hepatocytes, and the bilirubin becomes water-soluble.
- The bilirubin is taken to the hepatocytes, where albumin remains in the blood, and bilirubin goes into the hepatocytes from the sinusoidal surface.
- Bilirubin is tightly bound but reversibly in the hepatocytes and binds to the cytosolic binding protein, ligandin, and Z protein.
- Bilirubin undergoes the conjugation process in hepatocytes by combining with glucuronic acid (UDPGA = uridine diphosphate glucuronic acid) through the action of the smooth endoplasmic reticulum enzyme glucuronyltransferase (GT).
- The uridine diphosphate glucose (UDP-glucose) will form glucuronic acid.
- The main conjugation process takes place in hepatocytes with the assistance of glucuronic acid and the glucuronyl transferase enzyme.
- The microsomal enzyme bilirubin UDP-glucuronyl transferase catalyzes the formation of bilirubin monoglucuronide.
- ∼10% of bilirubin monoglucuronide is secreted into the bile.
- Then there is the formation of the bilirubin diglucuronide.
- ∼90% of the bilirubin diglucuronide is secreted into the bile.
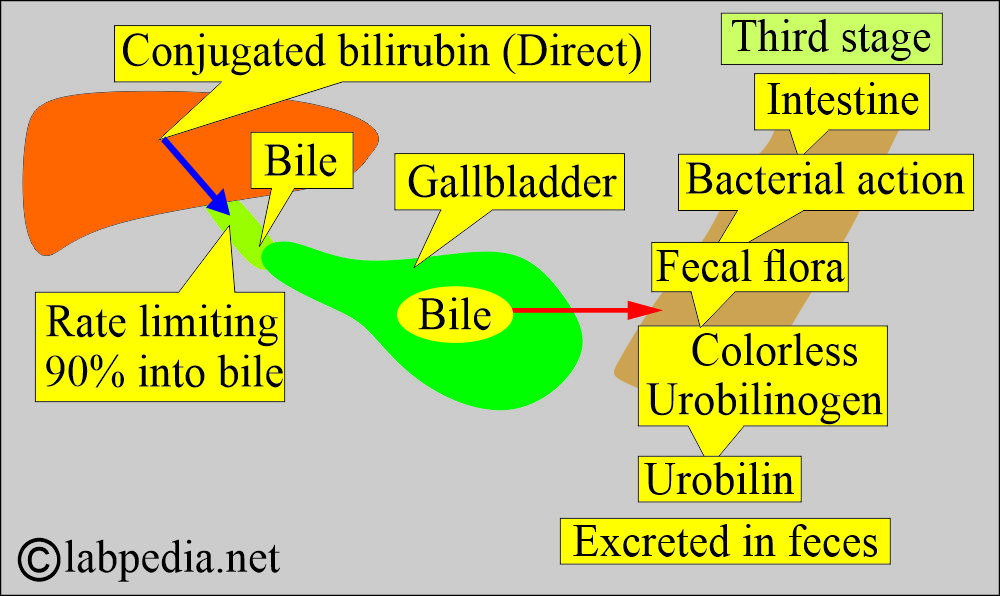
Third stage:
- The third stage is the secretion of conjugated bilirubin into bile and the intestine:
- The secretion of the conjugated bilirubin (bilirubin diglucuronide, direct reacting bilirubin) occurs by an active transport mechanism.
- This secretion of bilirubin in the bile is a rate-limiting process.
- Mainly, the conjugated bilirubin (90%) is secreted into the bile.
- This directly reacting conjugated bilirubin reaches the small intestine (terminal ileum) and the large intestine.
- Most of it is metabolized in the intestine and excreted in feces.
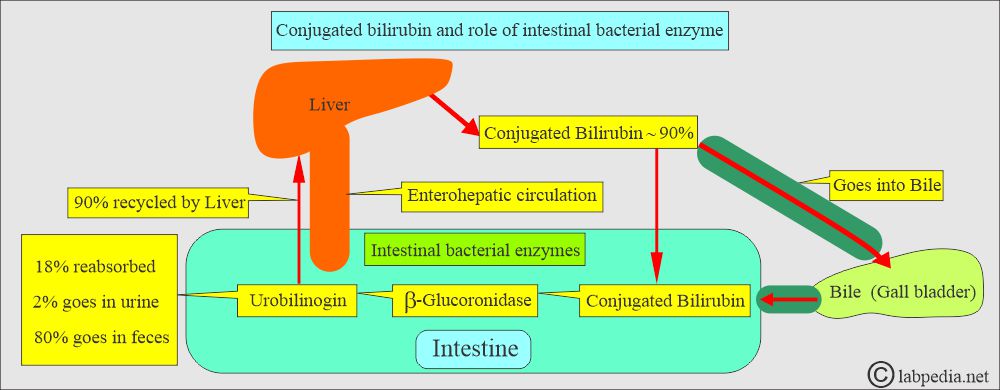
What is the fate of the Conjugated bilirubin in the intestine?
- When bilirubin reaches the terminal ileum and the large intestine, glucuronide is removed by specific bacterial enzymes, β-glucuronidase.
- The fecal flora reduces this pigment to a group of colorless tetrapyrrole compounds called urobilinogen.
- A small fraction of the urobilinogen in the small and large intestines is reabsorbed and excreted through the liver to form enterohepatic circulation.
- If the excessive formation of bile or liver disease interferes with the intrahepatic cycle, urobilinogen will be excreted in the urine.
- Normally, the colorless urobilinogen in the colon is oxidized by the fecal flora and forms the colored compound urobilin.
What are the various facts about bilirubin?
- The increased amount of bilirubin causes the yellow color of the skin and conjunctivae (Jaundice).
- Because bilirubin is an orange-yellow pigment derived from the metabolism of heme.
- Bilirubin is not absorbed in the intestine; it is hydrolyzed by the β-glucuronidase enzyme, which comes from:
- Liver.
- Intestinal epithelial cells.
- Bacteria.
- The intestinal microbial flora reduces this unconjugated bilirubin to urobilinogen (colorless tetrapyrrole compound).
- Analysis of the bilirubin from the sera of various patients with liver diseases shows the following pattern:
- Unconjugated bilirubin = 27%
- Monoconjugated bilirubin = 24%.
- Diconjugated bilirubin = 13%.
- Protein-bound bilirubin = 37%.
- The bilirubin, which is not conjugated, attaches to albumin (a carrying protein ), called Indirect bilirubin.
- Unconjugated (indirect) bilirubin is water-insoluble and bound to albumin in the blood.
- This unconjugated bilirubin is not seen in the urine.
How much is bilirubin in various body fluids?
- Bilirubin is more in the exudate (exudate more icteric) than transudate.
- CSF is more xanthochromic when there is meningitis.
- The basal ganglia are bile-stained due to the high unconjugated bilirubin concentration.
- Ocular fluids are yellow in deep jaundice.
- Urine, sweat, serum, and milk contain bile pigments.
- The paralyzed parts and edematous parts tend to remain uncolored.
- Skin, ocular sclera, and blood vessels contain high elastic tissue, which can easily become icteric.
What is the difference between direct (Conjugated) and Indirect (Unconjugated) bilirubin?
| Characteristics | Conjugated Bilirubin | Unconjugated Bilirubin |
| Structure | Bilirubin diglucuronide | Bilirubin IXα |
| Solubility | Water-soluble | Alcohol soluble |
| Type of compound | Polar | Non-polar |
| Vandenberg reaction | Direct | Indirect |
| Presence in urine with jaundice | Positive (loosely bound to albumin) | Negative (tightly bound to albumin) |
| Toxicity | Non-toxic | Toxic |
What do you know about Bilirubin?
Total Bilirubin = Direct bilirubin + Indirect bilirubin.
- Without an accelerator (alcohol), mainly conjugated bilirubin is measured (direct reaction).
- The accelerator also permits unconjugated bilirubin to react, providing a total bilirubin measurement.
- Indirect bilirubin is calculated as follows:
- Indirect bilirubin = Total bilirubin – direct bilirubin.
Urobilinogen
- It differs in the degree of hydrogenation of the vinyl side chain and the two pyrrole rings at the ends.
- Urobilinogen, containing 6, 8, and 12 more hydrogen ions, respectively, is called:
- Stercobilinogen.
- Mesobilinogen.
- Urobilinogen.
- Up to 20% of urobilinogen produced is reabsorbed and enters the enterohepatic circulation.
- Most of the urobilinogen is reabsorbed, taken up by the liver, and excreted in the bile.
- A small fraction of 2% to 5% goes into general circulation and appears in the urine.
- The bilirubin is conjugated with glucuronic acid. This process occurs in the liver and results in the formation of conjugated or direct bilirubin. Now, conjugated bilirubin is no longer bound to protein.
How is urobilinogen formed?
- Breakdown of the RBCs.
- In the liver, the unconjugated bilirubin is converted into conjugated bilirubin and delivered to the gallbladder.
- In the intestine, conjugated bilirubin by the gut bacteria is converted into urobilinogen.
What is the fate of urobilinogen?
- Enterohepatic circulation.
- Oxidized to urobilin and gives urine a yellow color.
- The remainder is converted into sterobilogen and excreted in the feces.
What are the causes of increased urobilinogen?
| Clinical condition | Causes |
|
|
|
|
|
|
|
|
What is the normal amount of urobilinogen in the urine?
- It is < 1mg/dL
How can you detect urobilinogen?
- It can be detected by using Ehrlich’s reagent.
- The sample may be urine or stool.
Bile
What are the constituents of bile?
- It is formed in the liver and consists of Bile salts, phospholipids, cholesterol, bicarbonate, bilirubin, and water.
- Bile consists of the following:
- Bile salt (conjugated bile acids).
- Bilirubin.
- Cholesterol.
- Electrolytes.
- Water.
- In the bile:
- Bilirubin diglucuronide is ∼90%.
- Bilirubin monoglucuronide is ∼10%.
- What are the types of bile acids?
- Primary bile acids are Cholic acid and chenodeoxycholic acid.
- Secondary bile acids are Deoxycholic acid and Lithocholic acid. Intestinal bacteria form these.
- What are the facts about bile acids and bile salts?
- Both primary and secondary bile acids are from the bile acid pool.
- The liver assists in intestinal digestion by secreting 700 to 1200 mL of bile /per day.
- Bile is a bitter taste, alkaline, and yellowish-green in color.
- Bilirubin is one component of bile transported from the liver, stored in the gallbladder, and delivered to the intestine.
- What are the functions of bile?
- Intestinal fat emulsification.
- Absorption of the fat.
- Bile has two fractions:
- The bile acid-dependent fraction consists of bile acids, cholesterol, lecithin (phospholipids), and bilirubin. The hepatocytes secrete this fraction.
- The bile acid-independent fraction, which is secreted by the hepatocytes and epithelial cells of bile canaliculi, is a bicarbonate-rich aqueous fluid that gives bile an alkaline pH.
Jaundice
How will you define jaundice?
- Jaundice appears when the bilirubin level is above 2.5 mg/dl.
- When the liver cannot conjugate bilirubin in the newborn, and if the level increases, this indirect bilirubin can cross the blood-brain barrier and lead to toxic injury to the brain, known as Kernicterus.
- If the bilirubin level exceeds 15 mg/dl, start the treatment to avoid brain damage.
- While physiologic jaundice appears after 3 to 4 days and subsides on its own.
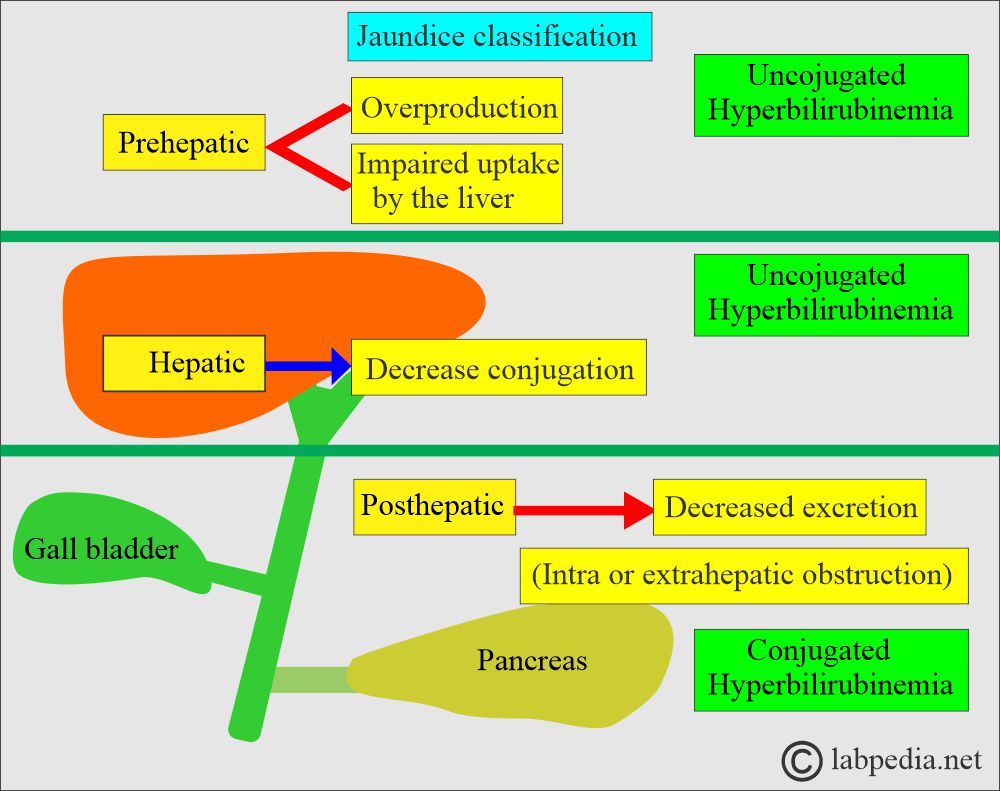
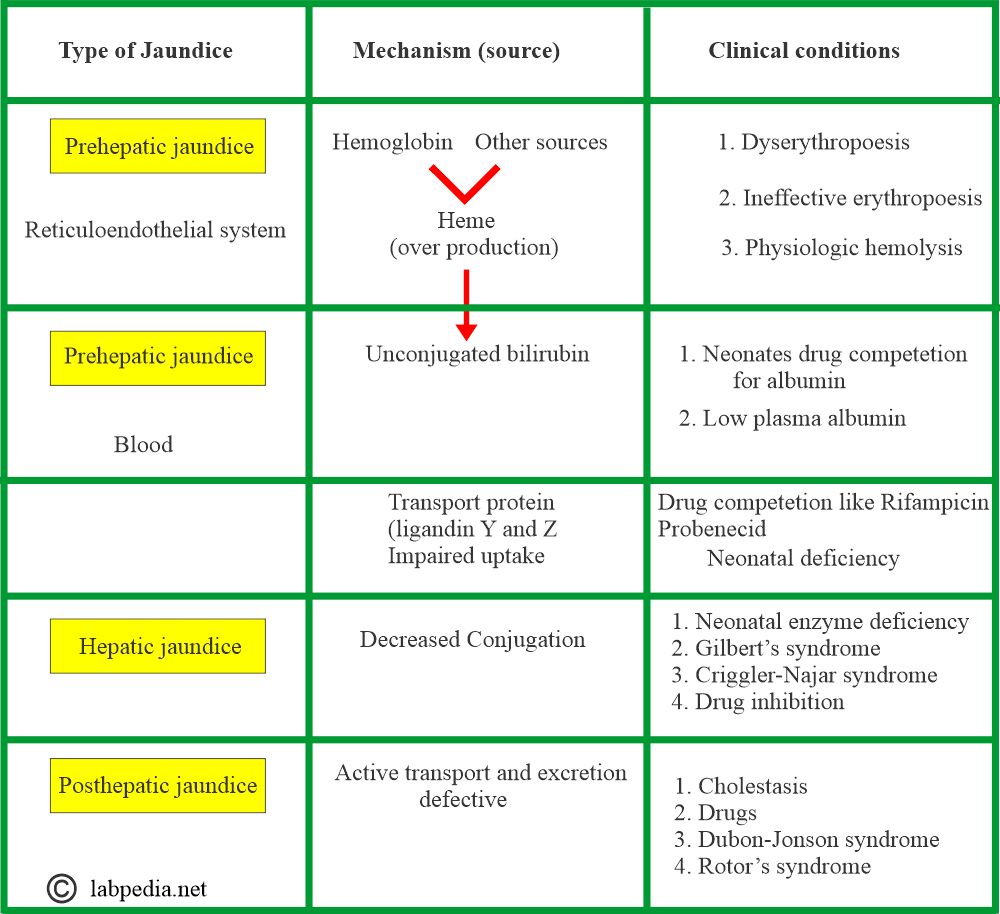
What are the types of jaundice?
- Pre-hepatic jaundice. The etiology occurs before the liver, such as increased hemolysis of RBCs.
- Hepatic jaundice. Now the causes are in the liver, like hepatitis.
- Post-hepatic jaundice. The cause is after the liver, like gallstones, and cancers, leading to the obstructive type of jaundice.
What are the types of jaundice, and what are their causes?
| Type of Jaundice | Causes | Pathophysiology |
|
|
|
|
|
|
What are the normal bilirubin values?
Adult values
- Total bilirubin = 0.3 to 1.0 mg/dL or 5.1 to 17.0 mmol/L
- Direct bilirubin (conjugated bilirubin) = 0.1 to 0.3 mg/dL or 1.0 to 5.1 mmol/L
- Indirect bilirubin (unconjugated bilirubin) = (total bilirubin minus direct bilirubin level) = 0.2 to 0.7 mg/dL or 3.4 to 11.9 mmol/L
- Total bilirubin in:
- Umbilical cord blood = less than 2 mg/ dl.
Infants values
- 0 to 1 day = less than 6 mg/ dl
- 0 to 2 days = less than 8 mg/ dl
- 3 to 5 days = less than 12 mg/dl
- after 5 days = less than .2 to 1.0 mg/ dl
- Urine is negative for bilirubin.
-
- For conversion to SI unit, multiply by 17.1 and report as µmol/L (mmol/L)
-
Another source: Total bilirubin level
| Age | Premature mg/dL | Full-term mg/dL | Adult mg/dL |
| Cord blood | <2 mg | <2.0 | |
| 0 to 1 day | <8.0 | 1.4 to 8.7 | |
| 1 to 2 days | <12.0 | 3.4 to 11.5 | |
| 3 to 5 days | <16.0 | 1.5 to 12.0 | |
| 5 days to 60 years | 0.3 to 1.2 | ||
| 60 to 90 years | 0.2 to 1.1 | ||
| >90 years | 0.2 to 0.9 |
What are the causes of raised Total Bilirubin levels?
- Some infections, such as an infected gallbladder or cholecystitis.
- Some inherited diseases, such as Gilbert’s syndrome.
- Although jaundice may occur in some people with Gilbert’s syndrome, the condition is not harmful.
- Diseases causing liver damage, such as hepatitis, cirrhosis, or mononucleosis.
- Diseases that cause blockage of the bile ducts, such as gallstones or cancer of the pancreas.
- Rapid destruction of red blood cells in the blood, such as sickle cell disease or an allergic reaction to blood received during a transfusion (called a transfusion reaction).
- Medicines that may increase bilirubin levels. This includes antibiotics, some types of birth control pills, indomethacin (Indocin), phenytoin (Dilantin), diazepam (Valium), and flurazepam (Dalmane).
What are the causes of decreased Total Bilirubin levels?
- Medicines that may decrease bilirubin levels. This includes vitamin C (ascorbic acid), phenobarbital, and theophylline.
What are the causes of direct hyperbilirubinemia (Conjugated bilirubin)?
- When more than 50% of the bilirubin is direct bilirubin.
- Gallstones.
- Gallbladder tumors.
- Inflammatory scarring or obstruction of the extrahepatic ducts.
- It can be resolved by surgery.
- Dubin-Johnson syndrome.
- Rotor’s syndrome.
- Drugs may cause cholestasis.
What are the causes of Indirect hyperbilirubinemia (Unconjugated bilirubin)?
- When the direct bilirubin level is less than 15% to 20%.
- Increased RBC hemolysis ( Erythroblastosis fetalis).
- Sickle cell anemia.
- Hepatitis.
- Cirrhosis.
- Crigler-Najjar syndrome.
- Gilbert syndrome.
- Congenital enzyme deficiency.
- Drugs
- Transfusion reactions.
- There is no role in surgery.
How will you differentiate between hepatocellular and cholestatic jaundice?
| Laboratory tests/ symptoms | Hepatocellular jaundice | Obstructive/cholestatic jaundice |
|
|
|
|
|
|
|
|
|
|
|
|
How will you diagnose jaundice?
- Advise liver function tests (LFT), which include:
- Total bilirubin
- Direct and indirect bilirubin.
- SGOT.
- SGPT.
- Alkaline phosphatase.
- Total proteins.
- Albumin level.
- γ-GT (gamma-glutamyltransferase) level.
- Bilirubin in urine:
- Foam test: This test is used to detect bilirubin in the urine.
- How will you perform the foam test?
- Place 3 to 5 mL of urine in the test tube.
- Cap the tube and shake it vigorously.
- If the foam at the top is white, = Test is negative (no bilirubin in the urine).
- If the foam is orange in color = the Test is positive (bilirubin is present in the urine).
- Precaution: Phenazopyridine also gives orange foam.
- Ictototest for bilirubin in the urine:
- This can detect bilirubin levels in urine as low as 0.05 mg/dL and as high as 0.1 mg/dL.
- Ictotest tablets are commercially available.
- Don’t expose the ictotest tablets to light, heat, or moisture.
What is the differential diagnosis of urine bilirubin and urine urobilinogen?
| Urine sample | Normal person | Hemolytic disease | Hepatic diseases | Biliary obstruction |
|
|
|
|
|
|
|
|
|
|
What are the differential diagnoses of various types of jaundice?
| Type of jaundice | Direct bilirubin | Indirect bilirubin | Stool bilirubin | Stool urobilinogen | Urine bilirubin | Urine urobilinogen | Total cholesterol |
|
Increased (early) | Increased (predominant) | Decreased | Decreased | Increased | Normal or increased | Normal or decreased |
|
Increased | Mild increase | Decreased | Decreased | Increased | Normal or decreased | Increased |
|
Increased early | Increased | Decreased | Decreased | Increased | Normal or increased | Normal |
|
Increased | Normal or mildly increased | Markedly Decreased | Markedly decreased | Increased | Decreased | Increased mild to marked |
|
Increased <indirect | Increased >direct | Increased | Normal or increased | Normal or decreased |
Questions and answers:
Question 1: What is the best indicator of obstructive jaundice?
Question 2: How will you decide the raised level of alkaline phosphatase from the liver or bone?

Thanks for best info and anlysis
Thanks for the comments.
I am testing LFT and found serrum bilirubin 3.1 so now what I do
You should have complete LFT (Bilirubin, direct and indirect, SGOT, SGPT, Alk.phosphatase, gamma-GT), HBV, HCV (viral profile) and ultrasound abdomen. I will also suggest you consult some good physicians.
Total bilirubin 0.51, direct bilirubin 0.14, indirect bilirubin 0.37
Hello Dr Riaz
Above is the lab finding of my father. Of this normal or abnormal value of liver function. Kindly help.
These values are in the normal range. What about SGOT and SGPT?. If those are normal then no need to worry.
Dear Dr Riaz,
Thank you for the info
LFT all in normal range
Except for the direct bilirubin it’s .341 mg/dl
While the total is .761
CBC lipid kidney vitamins etc all normal
I had an esophagectomy 3 years ago adenocarcinoma esophageal lower part of the esophagus early stage 1b no chemo or radiation only surgery
Do you think that the solitary slightly raised direct bilirubin is a cause of concern in my case while other blood tests are normal?
Thank you so much for your feedback
Your bilirubin is in the normal range.
Good day doctor, I am treating hbv with tenofovir, my total bilirubin is 15.59, conjugated bilirubin is 6.6, ast is 32.9, alt is 35.9, alkaline is 90, albumin is 4.4, total protein is 7.1, should I worry?
One thing that is strange for me is that your ALT and AST are normal, but bilirubin is too high. You have to worry about finding the cause of raised bilirubin level. Your liver function test suggests hemolysis, prehaptic jaundice. Do your eyes are yellow? Please consult a physician to find the cause of the increased bilirubin level.
I AM testing bilirubin 8.9 so how what I to
Thanks. Please see your email.
Hello I have been diagnosed with gilbert syndrome. What can I take to lower levels of indirect billirubin during episodes of jaundice.
Please help .
Please see this link:
https://labpedia.net/gilberts-syndrome-signs-symptoms-and-diagnosis/
Unless bilirubin is too high, there is no need for any treatment.
Respected Doctor.
First of all thank you. I am testing bilirubin ..total is 2.4 mg/dl..direct is 0.6 mg/dl and indirect is 1.8 mg/dl ..i feel weak and i have also nightfall problem ..what can Ido now ..please help me Dr. Riaz
I tested complete LFT SGOT, SGPT, Alk.phosphatase, gamma-GT), Protine, these all component is normal
Thanks.
Hi doctor
I have replied your comment.
Thanks . I test LFT ..and report found bilirubin direct 0.6 indirect 1.8 and total 2.4 mg/dl. other elements is normal … its danger or not ?..please suggest me .
Thanks. I have sent details in your email.
Thanks doc , Me too I have same problem
Total 2.5
Direct .9
In direct 1.6
I have rheumatoid arthritis and tacking hcq 200 mg one per day ,
Ag 35
Weight 85kg
And usually feel burn on the stomach,.
I did LFT few times due to concern of Hepatitis or Acute Pancreatitis.
Today test shows Biliruin level of 5. I am worried. Pls advice.
LFT Done at various dates in last one month
Date 10-Jul 23-Jul 25-Jul 05-Aug 09-Aug
Bilirubin -Total 0.50 1.10 2.40 3.80 5.05
Bilirubin – Direct 0.15 0.80 1.90 3.20 4.01
Bilirubin – Indirect 0.35 0.30 0.50 0.60 1.04
Total Protien – 8.50 8.20 8.70 8.46
Albumin 4.77 4.70 4.70 4.60 4.97
Globulin 2.86 3.80 3.50 4.10 3.49
SGOT – AST 55 125 250 67 48
SGPT – ALT 82 232 384 119 70
Alkaline Phosphatase 111 361 486 320 368
Gamma GT NA 1,017 1,193 412 298
Amylase Na 134 247 na na
Lipase Na 273 513 na na
Dear
Bilirubin is too high. You have not mentioned about Viral hepatitis profile particularly HBV, HCV. I hope you don’t take alcohol.
I will suggest you consult the physician.
thanks for reply Dr.
HBV and HCV non-reactive. Only antibody HAV – igg- 9.84 value
I am consulting physician.
Wanted your opinion Dr. As advisory.
Gallstones are ruled out by MRCP. Pancreatitis supsected. Recent Ultrasound says its is fine. No visible CBD obstruction.
I am very occasional drinker…last drink as 2 months ago.
Hi Dr. Riaz,
My father Bilirubin total is 2.9 in that direct is 2.0 and indirect is 0.9. Could you please advise on this. is this too high?
Please see your email.
Respected Doctor.
I got my 4 days old baby girl tested upon learning potential symptoms for jaundice. The results is as follows: Serum Bilirubin (Total) by DPD Method is 16.22, Serum Bilirubin (Direct) by DPD Method is 0.52 and Serum Bilirubin (Indirect) by DPD Method is 15.7. Phototherapy is adviced in report. Seek your advice as well. Please help Dr. Riaz
Dear, I have replied to you in your email.
Hi doctor
Please read my comment.
Sir maine apna blood test karwaya tho pata chala mera (direct Bilirubin 1.39) & indirect Bilirubin 3.16) aaya or mujhe koi symptoms Nahin dikh rahe sirf eyes Mein pilapan Hai Thoda Sa mujhe smjh nhi aa rha sir m kaya karu
Please advise the complete liver function test. If SGOT and SGPT are normal, then rule out the congenital hyperbilirubinemia. I will suggest consulting some physicians for the exact diagnosis. App nain apni age bhi naheen likhi.
My Total bilirubin leval (22)
But normal range 1.71 to 20.5
What I can understand you mean your bilirubin is 22 mg/dl. That is very high. Please if possible send the report or consult the physician.
I have tested for bilirubin quite a few times in this month.
Result are as such.
6/08/2020- Direct .3, Indirect 2.5
18/08/2020- Direct .39, Indirect 2.03, Alkaline phosphatase 360
24/08/2020- Direct .58, Indirect .63
Can you please tell me why direct has risen when my indirect bilirubin has fallen so drastically? Is there any special diet I can follow to reduce the direct?
First of all, I don’t know your age and sex. Rest Now your bilirubins are in the normal range. Best will be a repeat LFT after few days. If the values are above normal then consult a good physician.
I need your advise regarding infant bilirubin. My son of 16 days old result is
Total bilirubin 8.1 normal range up to 1 mg/dl
Direct bilirubin 0.64 normal range up to .25 mg/dl
If the bilirubin rises after 3 to 5 days then it is physiologic jaundice. Please give your son phototherapy. Also, keep on checking the total bilirubin, if it is rising then please consult the pediatrician immediately. Otherwise it should become normal.
My direct bilirubin is .0.30 is dangers
And total bilirubin 1.3
The total bilirubin is slightly raised. Please get a complete liver function test. If SGOt and SGPT are normal, then no need to worry. Repeat LFT after one month. If still bilirubin is raised then consult a physician.
Please advise LFT and ultrasound abdomen. If the LFT is abnormal then please consult a physician.
Please advice my father is 72 yrs old suffering from jaundice as well minor dibetic first time , after 1 month having medicine diabetic normal . but bilrubin is 2.9 , he having medicine 1. ursosave 300 -1*2 2. normflokind, 3. zory -o.5 once a day 4. traxol 1.5 -7 days 5. one tablet for gas as well constipation…..having medicine since 3 months …… since some days after 9:30pm full body tempreture approx 99 after that full body pain ..
please guide us dr. is going rt or wrong ….or we will have to change physician
You need complete liver function tests, ultrasound abdomen, and consultation with a good physician.
My father has jaundice his bilirubin level is 6.08 mg/dl … is thisvery high doctor?
His total bilirubin is 6.08 mg/dl
Bilirubin is too high. Please consult good physicians before it is too late.
He needs complete workup to find the cause of jaundice if his viral profile is negative.
Sir what is the treatment of hereditary spherocytes
Please consult to a clinical hematologist.
Yes, bilirubin is high.
Sir can I send the report to you …can you please what’s the condition is?
Yes, you can send me the report and I will give comments.
Sir Iam pregnant and my bilirubin ,direct is 0.37mg/DL only it is high
Hi Dr saab, My direct bilirubin is 13 umol/l and indirect bilirubin is 4. how can I find the total bilirubin level in umol/l?
Total bilirubin = Indirect bilirubin + direct bilirubin
Hi doctor sab, My direct Bilirubin is 0.91 mg/dl indirect bilirubin is 2.0 How can i find the bilirubin level in mg/dl value
Direct + indirect bilirubin = Total bilirubin
Hi, doc. My age is 28
My total bilirubin is 1.22 mg/dl – ref 0.2 to 1.0
Direct bilirubin is 0.14 mg/dl – ref upto 0.2
Indirect bilirubin is 1.08 mg/dl – ref upto 0.8
Can you tell me the condition
Your total bilirubin is borderline. Please wait and repeat bilirubin after few days from a different laboratory.
Hi, sir My age is 26
My total bilirubin is 4.54 mg/dl – ref 0.2 to 1.0
Direct bilirubin is 1.08 mg/dl – ref upto 0.2
Indirect bilirubin is 3.46 mg/dl – ref upto 0.8
AST – 31 ALT – 29 GGTP – 16 ALP – 71 PROTEIN – 7.50 ALBUMIN – 4.60 ND USG OF ABDOMEN IS NORMAL ON 25/10/20 nd at present i m feeling DAY BY DAY WEIGHT LOSS , WEAKNESS , DARK URINE…..I M WORRIED….WHAT I DO…CN U SUGGEST ME WHAT IS THE PROBLEM ???
Your LFT shows indirect bilirubin increased. While AST and ALT and Alk.phospharse are normal. Check your thyroid glands, and I hope not taking any medicines. You are losing weight and that is worrisome. Please better consult good physician.
Yes my thyroid TSH level was same day 12.48…..nd i am not taking specific medicine for that …
but i worried about my increased T.bilrubin level…..what i do for lower level …..i m totlly …depressed !!!!!
Hi Sir,
My mother, is suffering from jaundice.
Total bilirubin = 21
Direct = 14
Indirect=7
Viral Markers are negative
Ultrasound suggested normal with normal echopattern, slight gallbladder wall thickening.
Please suggest what should be the course of action?
ALT = 303.8
AST=407.8
ALP=189.5
Viral markers are negative so she does not have viral hepatitis. Definitely she needs hospitalization and a good physician.
Hi Sir, My mother is suffering from jaundice
Total Bilirubin= 23.3
Direct Bilirubin= 16.9
Indirect Bilirubin= 6.42-mg/dl
ALT= 303.8
AST= 407.8
ALP= 189.5
Viral markers are negative
Ultrasound suggests normal size and echopattern, with mild gallbladder wall thickening,
Please suggest what should be the course of action?
Thanks
Bilirubin direct is too high, showing direct hyperbilirubinemia. Other enzymes are also raised. But Alkaline phosphatase is not too high to rule out the obstruction. What is her ESR?. She might have a drug reaction. She needs thorough work up to rule out the cause of direct hyperbilirubinemia.
I think you should hospitalize your mother and get a consultation from a good physician.
Dear Sir,
My bilurubin is 2.5 direct .8 and indirect 1.6 SGOT 23.90 SGPT -25.10 S. alkeline 62 protien 6.8 albumin 4.5 globulin 2.3 GGT -14.01 Lectose Dehydrognose 398.5 KFT -Notmal HbA1C- Normal PT & INR- Normal ESR-6 CBC Normal Hb. 15.4
Ultrasound report -Normal HCV -Negative Hepatitis B -negative…….Please suggest me how to lower down it
Please check your email, replied in detail.
not regular alcohol taker but taken alcohol two weeks back no wait loss or no appetite loss my age is 32
not regular alcohol taker but taken alcohol two weeks back no wait loss or no appetite loss my age is 32…… pls reply
Hi Doctor,
My this week report says Total Bilirubin is 1.45, direct is 0.38 and indirect is 1.07 and earlier reports are as follows
13th Jan 2020 Total 1.5 Direct 0.08 and Indirect is 1.42
March 2019 is Total 1.32 Direct 0.28 Indirect is 1.04
I am type 2 diabetic Please advise me the condition of Liver function
Please check your email.
Hi I am 48 years old male & i did my yearly health check on fasting. The total Bilirubin 1.5 . Direct 0.1 and indirect 1.4, SGPT 44 on 31st October.
On 18 Nov I did the test again Post Lunch. The readings are Total Billirubin 1.3. Direct 0.8 and Indirect 0.5
Please suggest is this alarming. i drink alocohol once a week.
Hi I am 48 years old male & i did my yearly health check on fasting. The total Bilirubin 1.5 . Direct 0.1 and indirect 1.4, SGPT 44 on 31st October.
On 18 Nov I did the test again Post Lunch. The readings are Total Billirubin 1.3. Direct 0.8 and Indirect 0.5
Please suggest is this alarming. i drink alocohol once a week.
I was just going thru my reports and last 8 years in annual checkup my Bilirubin levels are in the same range from 1.2 to 1.5 with Fatty liver.
Please check your email.
Hi I am 48 years old male & i did my yearly health check on fasting. The total Bilirubin 1.5 . Direct 0.1 and indirect 1.4, SGPT 44 on 31st October.
On 18 Nov I did the test again Post Lunch. The readings are Total Billirubin 1.3. Direct 0.8 and Indirect 0.5
Please suggest is this alarming. i drink alocohol once a week.
Last 8-9 years my total bilirubin are in the same elevated range from 1.2 till 1.5 mg dl. My family dr says ignore maybe gilbert syndrome as I do not have any other symptoms
Please check your email.
Dear Sir,
I am 39 year old woman.
My Bilirubin Total is 2.35
Direct 0.42
Indirect 1.93
SGOT 39
SGPT 42
GGTP 21
Alkaline Phosphate 81
Total Protein 6.98
Albumin 4.42
A:G Ratio 1.73
Urea 21.80
Creatinine 0.53
Haemoglobin 14.20
Eosinophils 0.60
Basophils 0.00
Mean Platelet Volume 12.10
Folate, Serum 5.00
You have mild indirect bilirubinemia. Please keep an eye on your LFT. Repeat after every 3 months. There is a role of phenobarbitone but consult a physician for its use. Or you can do phototherapy. This is the safest method.
Dear Sir,
My bilurubin is 2.5 direct .8 and indirect 1.6 SGOT 23.90 SGPT -25.10 S. alkeline 62 protien 6.8 albumin 4.5 globulin 2.3 GGT -14.01 Lectose Dehydrognose 398.5 KFT -Notmal HbA1C- Normal PT & INR- Normal ESR-6 CBC Normal Hb. 15.4
Ultrasound report -Normal HCV -Negative Hepatitis B -negative…….Please suggest me how to lower down it…not regular alcohol taker but taken alcohol two weeks back no wait loss or no appetite loss my age is 32
thank you so much Sir
Hi I am 43 years old male .I did LFT on 17-10-2020 and on 22-11-2020.
My LFT values are total Bilirubin 1.29 . Direct 0.42 and indirect 0.87, SGOT 26.61 , SGPT 18.85 on 17 October.
My LFT values are total Bilirubin 1.3 . Direct 0.5 and indirect 0.80, SGOT 40.0 , SGPT 32 on 22 November.
i dont take alcohol
I think youR LFT looks normal. Please repeat after 4 weeks.
Sir , Got following results for my Mother (63 Yrs) on 22 Nov 2020 :
Indirect Bilurubin in above range , kindly advise :
BILIRUBIN -DIRECT : 0.27 mg/dl
BILIRUBIN – TOTAL : 1.36 mg/dl
BILIRUBIN (INDIRECT) : 1.09 mg/dl
ALKALINE PHOSPHATASE : 83.2 U/L
GAMMA GLUTAMYL TRANSFERASE (GGT) : 15.5 U/l
ASPARTATE AMINOTRANSFERASE (SGOT ) : 25.8 U/l
ALANINE TRANSAMINASE (SGPT) : 28.6 U/l
PROTEIN – TOTAL : 7.11 gm/dl
ALBUMIN – SERUM : 4.23 gm/dl
SERUM GLOBULIN : 2.88 gm/dL
SERUM ALB/GLOBULIN RATIO : 1.47
There is a mild increase in Bilirubin and indirect bilirubin. Please repeat only bilirubin and its fractions after one month and see the result. I hope this may become normal.
But sir , my doctor has put me on no-oil diet for next 10 days and asked to repeat test after that. Moreover though i have no vomitting , hunger is same as before , but have occasional pain on th right side below rib cage , that’s why i di d LFT done . I smoke weed at least 5 times a week
Dr.
39 week newborn Billi levels 24 hours after birth were 5.5 total with .6 being direct. Then we re-did it 5.5 days after birth and they were 6.7 total with .9 being direct. Should I be concerned with the increase in both the indirect but mostly the direct? Most doctors are not concerned at this point in time. Baby is eating/peeing/pooping normal. I am nervous about BA.
Dr.
39 week newborn Billi levels 24 hours after birth were 5.5 total with .6 being direct. Then we re-did it 5.5 days after birth and they were 6.7 total with .9 being direct. Should I be concerned with the increase in both the indirect but mostly the direct? Most doctors are not concerned at this point in time. Baby is eating/peeing/pooping normal. I am nervous about BA.
This may be physiologic jaundice. It needs phototherapy. The only concern is that jaundice appears within 24 hours. You have to keep an eye on total bilirubin level, it should not cross 12 mg/dL because after 15 mg/dL needs immediate treatment.
at what point do you stop worrying about BA? Right now my son is one month old as of tomorrow. As of 12/15, total billi is at 3.4 with direct at 1.2 (different lab). Direct has never gone above 1 on the four previous draws. We did it at a different lab this time. All liver tests including GGT are normal. The only thing is that ALP is elevated to 600, but it’s a newborn and since GGT is normal that seems ok. What do you think? No jaundice, stools are still the correct color.
My new born baby (male) having high direct bilirubin (3.02) where as total bilirubin is 7.10 , direct bilirubin gradually increased from 1.43, 1.69, 2.49,2.75, 2.60 , 3.02
Lft done where alp is slightly higher than benchmark
Ultrasound abdomen done where everything seems normal
Urine for reducing substances done where result comes negative
Stool colour is yellowish
Recommended hida test but baby unable to inject radioactive syrup .
Please suggest what is the reason behind increased direct bilirubin .
It is good that direct bilirubin is increasing, which shows that the liver is working. Please keep monitoring that bilirubin should not go above 10 mg/dL. Also, give phototherapy. I am sure that the baby is under the supervision of a pediaarician.
Praveen,
My son had a similar situation and I’ve been researching this. Those are abnormal numbers. What is the timeframe between the increases? My sons ALP was also elevated. Did you get a GGT level done?
Good day Doctor, please help me out am on drug for hepatitis B. I did LFT in August 2020 the results is normal after three months it’s elevated (higher)
August, 5th 2020
Total bilirubin is 0.55 mg/dl..
Direct is 0.16 mg/dl
Indirect is 0.39 mg/dl
ALT 36.11 ref up to 49
AST 26.86 ref up to 46
ALP 177 ref 64-306
Total protein 74 ref 62-80
Albumin 46 ref 35-50
November, 11th 2020
After three months that I repeat the LFT November my results is nown give.
Total bilirubin is 2.28 mg/dl..
Direct is 0.68 mg/dl
Indirect is 1.6 mg/dl
ALT 20.76 ref up to 49
AST 25.64 ref up to 46
ALP 179 ref 64-306
Total protein 76 ref 62-80
Albumin 40 ref 35-50
Ultrasound report -Normal HCV – positive Hepatitis B positive which the HBV DNA copies is < 28 copies/ml is less than what machine can detect.
Please suggest me how to lower down it
total bilirubin 2.4 mg dl direct bilirubin 1.0 mg/dl indirect bilirubin 1.4 mg/dl sir what I do
total bilirubin 2.4 mg dl direct bilirubin 1.0 mg/dl indirect bilirubin 1.4 mg/dl sir what I do
Hemoglobine 9.6 G/dl female
Your indirect bilirubin and total bilirubin are raised. Hemoglobin is also low. I will suggest you consult a physician for further workup.
Good day, doctor! May I ask if what is the formula in the calculation of the Bilirubin Concentration of the unknown and Control? And can I ask for some examples of the computation?
This is a universal formula for unknown substances= Concentration of unknown/concentration of standard = OD of unknown / OD of standard. You can solve this by knowing three values. and unknown will be the answer.
Good day, doctor! May I ask if what is the formula in the calculation of the Bilirubin Concentration of the unknown and Control? And can I ask for some examples of the computation?
Hi doctor my indirct bilurburin is 2mg/ dl
And my direct bilurburin is 0.7mg/ dl
Alt – Ast normal , my age is 35 and i have no symptoms , does it mean i have liver damage
Your total bilirubin and indirect bilirubin are raised. You need to work up to find the pathology or cause of the increased bilirubin. No doubt this is benign hyperbilirubinemia. Still, I will suggest consulting a physician.
Doctor,
One month 10 days old with Total Bilirubin value at 16.5 mg/dl – direct value of 0.3, other tests for thyroid, count and culture for blood and urine are normal. Currently running an antibiotic course of 7 days for ear infection. Feeding, peeing are normal. We have been advised by doctors to wait and retest again.
Please advise.
You have not told me when jaundice appears? Anyhow the recommendations are if bilirubin is above 15 mg/dL, then immediate treatment is needed by exchange blood transfusion or phototherapy. I will also recommend checking bilirubin levels daily to avoid damage to the brain. This should not cross 20 mg/dL.
Doctor,
Jaundice was there during the first week, it became normal after a few sessions of photo therapy. This is appeared again after almost 35 days after birth. The doctors have suggested breast milk jaundice.
Rgds.
There is a condition of breast milk jaundice, I am sending you the CDC publication. Please read this for information. Again I will say bilirubin 15 mg/dL is not safe for the infant.
https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/jaundice.html#:~:text=Breast%20milk%20jaundice%20most%20often,infant's%20liver%20to%20process%20bilirubin.
Thank you very much for your insight. Levels have come down. Very much appreciate your quick turnaround replies.
Rgds.
Hi Doctor
my
total Bilirubin is 2.49
Direct Bilirubin is 1.31
Indirect Bilirubin is 1.18
A.S.T (SGOT) IS 18
A.L.T (SGPT) is 26.8
my age is 22 years
Your total bilirubin is raised. Also, direct and indirect bilirubin are raised, but SGOT and SGPT are normal. It means there is no active liver cell disease (necrosis). Your result is confusing to rule out congenital hyperbilirubinemia. It looks benign hyperbilirubinemia. It would help if you had further workup like ultrasound and repeat bilirubin total and direct, indirect.
I have done LFT
TOTAL BILRUBIN 2.1
DIRECT 0.5
INDIRECT 1.60
SGPT 51
IS THIS FINE OR NEED ANY TREATMENT BECAUSE I AM FEELING NAUSEA
Your bilirubin is raised, and SGPT is also mildly raised. You need to consult a physician for a workup and to reach the diagnosis.
My bilrubin total is 1.17 and globulin is 2.90. rest sgot, sgpt etc. Are in normal. Further my total cholesterol is 213, triglycerides 232, LDL 118, VLDL 46.4, chol/hdl ratio 4.44, total lipids 658. Pls advice
Liver functions are normal, but lipid profile is abnormal. Cholesterol and triglycerides are raised. I think you need to control the lipid profile.
Hi sir,
I took blood test recently, my direct bilirubin is 0.3 and total was 1.9 .
Kindly help me is it dangerous ?
Since I am non-alcoholic non-smoker
You should have complete lever functions, SGOT/SGPT, and alkaline phosphatase. Also, get a viral hepatitis profile.
My elder brother bilirubin total is 1.3, direct bilirubin is 0.4, indirect bilirubin is 0.9 ,globulin is 3.0, SGOT is 38, SGPT is 74, GGT is 81 and alkaline phosphatase is 62. Please kindly help me is it dangerous?? Since he is non alcoholic non smeker
SGOT is just normal, but SGPT is high, which indicates some problems with the liver. Please check his viral hepatitis markers. I will suggest repeating the liver functions test (Bilirubin, SGOT, SGPT, ALK.phosphatse, and gamma GT) after one month.
But sir his HBsAg report is non reactive. But SGPT is 74 And GGT is 81 And bilirubin total is 1.3, Direct bilirubin is 0.4 And indirect bilirubin is 0.9. So is it dangerous?
hello sir,
i am aged 30 , male ,my blood test report hemoglobin 17.3g/dl , RBC count 6.79 millions, packed cell volume- 59.6 vol% and total bilirubin -1.3 mg/dl and direct bilirubib 0.6mg/dl. please commment on the results
You Hemoglobin and RBC count are in the high range. It needs further workup and consultation by a physician.
My HBsAg report is non reactive. But SGPT is 74 And GGT is 81 And bilirubin total is 1.3, Direct bilirubin is 0.4 And indirect bilirubin is 0.9. Please kindly help me sir is it dangerous? Since I’m non smoker
My HBsAg report is non reactive. But SGPT is 74 And GGT is 81 And bilirubin total is 1.3, Direct bilirubin is 0.4 And indirect bilirubin is 0.9. Please kindly help me is it dangerous?
sir his HBsAg report is non reactive. But SGPT is 74 And GGT is 81 And bilirubin total is 1.3, Direct bilirubin is 0.4 And indirect bilirubin is 0.9. So is it dangerous?
Your LFT (SGOT/SGPT) is raised. I hope you are nonalcoholic and not taking any medication. You should also check the Hepatitis C virus. Also raised SGOt/SGPT not good for health.
Very comprehensive read. I just got checked out as well and my total bilirubin was 0.8 with direct bilirubin being 0.31 and Sgpt sgot ggt levels as well as alkaline phosphotase normal. The lab says normal values of direct bilirubin are 0.2 but mine were 0.3. Is this something to check further?
I don’t think you need to worry.
Sir My Total Serum Bilirubin Is 5.7
Conjugated Bilirubin 3.1
Unconjugated Bilirubin 2.6
What Kind Of Jaundice Is This?
I Am 21 Years Old .
I am having yellowish skin and eyes and dark urine and Pale Stools.
No Other Symptoms.
Sir My Total Serum Bilirubin Is 5.7
Conjugated Bilirubin 3.1
Unconjugated Bilirubin 2.6
What Kind Of Jaundice Is This?
I Am 21 Years Old .
I am having yellowish skin and eyes and dark urine and Pale Stools.
My Skin Is Itching No Other Symptoms.
What kind Of Jaundice is this?
Itching is a sign of obstructive jaundice. Yellow skin appears when bilirubin is above 2 mg/dL. It would help if you had an ultrasound abdomen to rule out gall stone or any other cause of obstruction.
Respected Sir,
My son 17 years old affected by Type 1 diabetes, finding bilirubin 1.5MGms% Direct 0.8, indirect 0.7. SGOT 10.5U/L, SGPT 13.2. Any advise for him. three years back he affected by Jaundice.
I think to check Hepatitis B and C. His enzymes are normal. No need to worry, and just do his every 3 to 6 months, his LFT (liver function test).
Very nicely elaborated. I have 0.35mg/dL. Let kindly me know about any treatment or precautions,
The bilirubin is normal. I don’t know about your all liver function test?
Dear doctor, in the last few months I had 3 blood tests with the following results:
February 2021:
Bilirubin Total= 1.51 mg/dl
Bilirubin Direct = 0.44 mg/dl
AST = 19 U/L
ALT = 15 U/L
Alkaline Phosphatase = 40 U/L
Total Protein = 7.28 g/dl
Albumin = 4.18 g/dl
April 2021
Bilirubin Total = 2.02 mg/dl
Bilirubin Direct = 0.58 mg/dl
AST = 21 U/L
ALT = 16 U/L
Alkaline Phosphatase = 50 U/L
Total Protein = 7.66 g/dl
Albumin = 5.24 g/dl
July 2021
Bilirubin Total = 1.43 mg/dl
Bilirubin Direct = 0.53 mg/dl
AST = 25 U/L
ALT = 17 U/L
Alkaline Phosphatase = 53 U/L
Total Protein = 7.46 g/dl
Albumin = 4.14 g/dl
LDH = 139 U/L
My doctor ignored the result and tells me about a probable Gilbert syndrome. He told me to stay calm. But I am quite worried, since I see that the direct Bilirubin is the one that rises the most (not the indirect one which is what happens in Gilbert’s syndrome).
In my last analysis, the Direct Fraction was 37% and the Indirect Fraction 63% if I did not do the math wrong.
I will greatly appreciate your response and if I can definitely rest assured with these results.
Best regards from Argentina
Dear doctor in the last few months I had 3 blood tests with the following results:
February 2021:
Bilirubin Total= 1.51 mg/dl
Bilirubin Direct = 0.44 mg/dl
AST = 19 U/L
ALT = 15 U/L
Alkaline Phosphatase = 40 U/L
Total Protein = 7.28 g/dl
Albumin = 4.18 g/dl
April 2021
Bilirubin Total = 2.02 mg/dl
Bilirubin Direct = 0.58 mg/dl
AST = 21 U/L
ALT = 16 U/L
Alkaline Phosphatase = 50 U/L
Total Protein = 7.66 g/dl
Albumin = 5.24 g/dl
July 2021
Bilirubin Total = 1.43 mg/dl
Bilirubin Direct = 0.53 mg/dl
AST = 25 U/L
ALT = 17 U/L
Alkaline Phosphatase = 53 U/L
Total Protein = 7.46 g/dl
Albumin = 4.14 g/dl
LDH = 139 U/L
My doctor ignored the result and tells me about a probable Gilbert syndrome. He told me to stay calm. But I am quite worried, since I see that the direct Bilirubin is the one that rises the most (not the indirect one which is what happens in Gilbert’s syndrome).
In my last analysis, the Direct Fraction was 37% and the Indirect Fraction 63% if I did not do the math wrong.
I will greatly appreciate your response and if I can definitely rest assured with these results.
Best regards!
Dear doctor, in the last few months I had 3 blood tests with the following results:
February 2021:
Bilirubin Total= 1.51 mg/dl
Bilirubin Direct = 0.44 mg/dl
AST = 19 U/L
ALT = 15 U/L
Alkaline Phosphatase = 40 U/L
Total Protein = 7.28 g/dl
Albumin = 4.18 g/dl
April 2021
Bilirubin Total = 2.02 mg/dl
Bilirubin Direct = 0.58 mg/dl
AST = 21 U/L
ALT = 16 U/L
Alkaline Phosphatase = 50 U/L
Total Protein = 7.66 g/dl
Albumin = 5.24 g/dl
July 2021
Bilirubin Total = 1.43 mg/dl
Bilirubin Direct = 0.53 mg/dl
AST = 25 U/L
ALT = 17 U/L
Alkaline Phosphatase = 53 U/L
Total Protein = 7.46 g/dl
Albumin = 4.14 g/dl
LDH = 139 U/L
My doctor ignored the result and tells me about a probable Gilbert syndrome. He told me to stay calm. But I am quite worried, since I see that the direct Bilirubin is the one that rises the most (not the indirect one which is what happens in Gilbert’s syndrome).
In my last analysis, the Direct Fraction was 37% and the Indirect Fraction 63% if I did not do the math wrong.
I will greatly appreciate your response and if I can definitely rest assured with these results.
Best regards from Argentina
Your question is answered.
Dear doctor, in the last few months I had 3 blood tests with the following results:
February 2021 *** April *** July:
Bilirubin Total= 1.51 mg/dl *** 2.02 mg/dl *** 1.43 mg/dl
Bilirubin Direct = 0.44 mg/dl *** 0.58 mg/dl *** 0.53 mg/dl
AST = 19 U/L *** 21 U/L *** 25 U/L
ALT = 15 U/L *** 16 U/L *** 17 U/L
Alkaline Phosphatase = 40 U/L *** 50 U/L *** 53 U/L
Total Protein = 7.28 g/dl *** 7.66 g/dl *** 7.46 g/dl
Albumin = 4.18 g/dl *** 5.24 g/dl *** 4.14 g/dl
LDH = n/a *** n/a *** 139 U/L
My doctor ignored the result and tells me about a probable Gilbert syndrome. He told me to stay calm. But I am quite worried, since I see that the direct Bilirubin is the one that rises the most (not the indirect one which is what happens in Gilbert’s syndrome).
In my last analysis, the Direct Fraction was 37% and the Indirect Fraction 63% if I did not do the math wrong.
I will greatly appreciate your response and if I can definitely rest assured with these results.
Best regards from Argentina
Dear doctor, in the last few months I had 3 blood tests with the following results:
February 2021 *** April *** July:
Bilirubin Total= 1.51 mg/dl *** 2.02 mg/dl *** 1.43 mg/dl
Bilirubin Direct = 0.44 mg/dl *** 0.58 mg/dl *** 0.53 mg/dl
AST = 19 U/L *** 21 U/L *** 25 U/L
ALT = 15 U/L *** 16 U/L *** 17 U/L
Alkaline Phosphatase = 40 U/L *** 50 U/L *** 53 U/L
Total Protein = 7.28 g/dl *** 7.66 g/dl *** 7.46 g/dl
Albumin = 4.18 g/dl *** 5.24 g/dl *** 4.14 g/dl
LDH = n/a *** n/a *** 139 U/L
My doctor ignored the result and tells me about a probable Gilbert syndrome. He told me to stay calm. But I am quite worried, since I see that the direct Bilirubin is the one that rises the most (not the indirect one which is what happens in Gilbert’s syndrome).
In my last analysis, the Direct Fraction was 37% and the Indirect Fraction 63% if I did not do the math wrong.
I will greatly appreciate your response and if I can definitely rest assured with these results.
Thank you very much!
Your AST and ALT are normal, which indicates that there is no liver cell necrosis. So this is benign, mild hyperbilirubinemia. Just in routine, take more fruits, avoid alcohol intake and tobacco smoking.
Hello.
I took a blood test and my levels were
3.0 total
2.5 indirect and 0.5 direct last September
I had a CT scan of abdomen and saw unremarkable (liver, gallbladder and pancreas)
I recently had another blood test
Total 2.2
Indirect 1.9
Direct 0.3
AST was 16
ALT was 22
Negative for hepatitis
4.5 Albumin
2.4 Globulin
Having Pale/yellowish stools last month
What do you think
You have not mentioned age?. Anyhow your enzymes are normal, which shows no liver cells necrosis. There is indirect hyperbilirubinemia. It looks like benign hyperbilirubinemia. I will suggest a follow-up.
I’m male and 37
I am male age 24 having billiribum total is 1.3,indirect is 1.3 and having sgpt is 54 and sgot is 51 and this value are comparabely similar for past three month.
These values are the upper limit of liver functions. There is mild injury going on in the liver. Are you taking any drugs?
sir can you give the latest treatment guidelines for unconjugated hyperbilirubinemia. thank you.
First, you have to find out the cause of unconjugated hyperbilirubinemia; then, you have to follow a different protocol for each disease.
sir, my total billiribum is 1.4 since march 2021. Before it was 1.2. SGPT and SGOT is slightly high. I am diabetic for the last 15 years. SGPT and SGOT are can lowering by Lamarin 70 twice daily. But builrubin cannot. Any detailed examination is required?
You have not mentioned that how much SGOT/SGPT is raised. I hope you are not taking alcohol. Only you need in routine liver functions test after every three months interval. Please also check the viral hepatitis profile. Ultrasound of the abdomen, particularly the liver, may be advised.
Thank you Sir, as per the test result dated 25-oct-21, Bilrubun total:1.4 mg/dl , bilrubin direct:0.5mg/dl, SGOT: 43 U/L, SGPT: 65 U/L, Alkaline phospatase: 63 U/L, Total protien 6.5 gm/dl and albamin: 4.4 gm/dl. I am not alcoholic. RFT parameters as found in in permissible limit.
Thank you sir.
Thank you Sir, as per the test result dated 25-oct-21, Bilrubun total:1.4 mg/dl , bilrubin direct:0.5mg/dl, SGOT: 43 U/L, SGPT: 65 U/L, Alkaline phospatase: 63 U/L, Total protien 6.5 gm/dl and albamin: 4.4 gm/dl. I am not alcoholic. RFT parameters as found in in permissible limit.
Thank you sir.
Hi Sir
Latest LFT report is as below for age 39 years (male)::
Bilirubin (Total) 1.33 mg/dL
Bilirubin Direct 0.38 mg/dL
Bilirubin Indirect 0.95 mg/dL
Total Protein 6.88 gm/dL
Albumin 84 9/dl BCG
Globulin 2.04 gm/dL
Albumin: Globulin 2.37
Alkaline Phosphatase 89.19 U/L
ALT/ SGPT 66.10U/L
AST/ SGOT 34.76 U/L
Gamma GT (GGT) 16.09 U/L
My weight is decreasing since 4-6 months (from 48 to 45.2 kg)
I am taking ursocol 300mg and Trinergic-L since 25 days, please advise if anything else to consider to address weight loss
Dear Kumar
I can answer limited questions. There is a mild increase in the SGPT, which is specific for the liver cell injury. But your SGOT is normal which is not clear to me. Would you please repeat your Liver function test from a different lab?. I have no idea about the side effects of the medicines.
Hi Sir.
I repeated my LFT and also tested for lipid profile. Here are the results:
Bilirubin (Total) 1.43 mg/dL
Bilirubin Direct 0.37 mg/dL
Bilirubin Indirect 1.06 mg/dL
Total Protein 7.16 gm/dL
Albumin 4.81 g/
Globulin 2.35 gm/dL
Albumin: Globulin 2.05
Alkaline Phosphatase 99.82 U/L
ALT/ SGPT 51.60 U/L
AST/ SGOT 32.95 U/L
Gamma GT (GGT) 12.95 U/L
Total Cholesterol : 197.84 mg/dL
HDL : 46.50 mg/dL
LDL: 120.19 mg/dL
non-HDL : 151.34
VLDL : 31.15 mg/dL
Triglycerides : 138.30 mg/dL
Medicines advised:
1) Udiliv
2) Rifagut 400
3) DDR 30
4) Betonin syp.
Kindly provide your feedback .
Thanks
Kumar
Hello Doctor,
My baby 1 month old(female) was tested for jaundice and the Total bilirubin values are as follows
15.7 – Direct(1.9) and Indirect(13.8)
12.3 – Direct(2.3) and Indirect(10.0)
11.9 – Direct(2.1) and Indirect(9.8)
8.3 – Direct(2.3) and Indirect(6.0)
7.2 – Direct(3.4) and Indirect(3.8)
7.2 – Direct(3.9) and Indirect(3.3)
As per the current latest LFT test(Today’s)
7.2 – Direct(3.9) and Indirect(3.3)
SGOT – 219
SGPT – 123
ALP – 448
Total protein – 4.1
Albumin – 3.0
Globulin – 1.1
Albumin/Globulin – 2.7
GGT – 72
Ultrasound and CT scan revealed that there are multiple small hemangomas on the liver.
HIDA scan was normal.
Please let us know, if the current LFT report is normal?
The current LFT report is abnormal. This LFT shows liver cell injury because SGOt/SGPT are raised. Alkaline phosphatase is raised in children and should be considered normal.
Thank you, Doctor for the quick response. Is there any concern, is it dangerous?? We are going to follow up with doctor today. How long does it take usually for the bilirubin to come down to normal levels in babies? Per our data, is there any improvement in the bilirubin levels? Baby’s Direct bilirubin level is going up each time, while the indirect is coming down. Is there any concern?
Thank you sir, would repeat the LFT /lipid test and share for your kind review
Ok, I will work on these two topics and you can check in just one week’s time.
please see this link. It is updated.
https://labpedia.net/liver-function-tests-part-1-liver-function-tests/
Dear Sir,
MY TSH-8.6
Total-2.35
Direct–0.75
Indirect-1.60
Alkaline phosphatase-49
what is this? and what should I do doctor sir?/
Help me
https://labpedia.net/thyroid-part-2-thyroid-stimulating-hormone-tsh-thyrotropin/
Your TSH indicates hypothyroidism. Please see the above link.
You have not mentioned a total of 2.35; is this bilirubin?
Hello Dr, I recently completed 6 months of antibiotics for a chronic UTI. Now my bilirubin is elevated and I am worried. I am 43 year old female, otherwise healthy. Take NP thyroid for hypothyrodism (this my only medication) Here are my values:
Bili Indirect 0.2
Bili Direct 1.2
Total 1.4
AST 13
ALT 10
Alkphos 54
Hemoglobin 13.3
I am sorry, here are the correct numbers!
Hello Dr, I recently completed 6 months of antibiotics for a chronic UTI. Now my bilirubin is elevated and I am worried. I am 43 year old female, otherwise healthy. Take NP thyroid for hypothyrodism (this my only medication) Here are my values:
Bili Indirect 1.2
Bili Direct 0.2
Total 1.4
AST 13
ALT 10
Alkphos 54
Hemoglobin 13.3
Your total bilirubin is not significant. Enzymes are normal. Just relax and repeat the complete liver function test after 2 to 3 months. Eat more fruits.
Thank you Dr. What do you make of the itching then? Isn’t this associated with a high billirubin level? I worry about pancreatic tumors.
You have not mentioned itching. Your Alkaline phosphatase is normal. So itching may be due to any other reason and not related to the liver.
hI sir, last week 24.02.2022 i have taken LFT test and reports as below Please need your help and advise sir pelase
BILLIRUBIN-TOTAL – 2.0
BILLIRUBIN DIRECT -0.6
BILLIRUBIN INDIRECT – 1.4
SGOT – 16
SGPT- 15
GAMMA GT – 12
ALKALINE PHOSPATASE – 62
TOTAL PROTEIN – 7.0
ALBUMIN- 4.5
GLOBULIN- 2.50
A/G RATIO- 1.80
You have indirect hyperbilirubinemia. Rest your liver function tests are normal. If you have no symptoms, repeat bilirubin after 1 to 2 months. If bilirubin is still raised without any symptoms, it is benign hyperbilirubinemia. In the future, you need to check your bilirubin level.
Doctor i am feeling good except having on and off vomitting sensation rarely apart from that doing my routing thing normally. Please advice on this also please
Thanks for your kind words Doctor, Benign Hyperbilirubinemia is anything need to concern or worry. What kind of treatment i need to further go ahead and advice on the diet to follow doctor please. Benign hyperbilirubinemia i am little worried Doctor, is it anything serious on this. Please help and guide please
Suppose you don’t find any other abnormality except bilirubin. In benign hyperbilirubinemia, keep an eye on the bilirubin level. You can repeat LFt every 6 months interval.
Doctor, one more request Doctor . I am having GERD issues also and feeling irration in throat on and off its anything related to my LFT please advice. Reports already shared for your kind references please
GERD has no relation with benign hyperbilirubinemia. You should do dinner at least 3 hours before going to sleep. Also, raise the bedhead side.
Hi Sir.
I repeated my LFT and also tested for lipid profile. Here are the results:
Bilirubin (Total) 1.43 mg/dL
Bilirubin Direct 0.37 mg/dL
Bilirubin Indirect 1.06 mg/dL
Total Protein 7.16 gm/dL
Albumin 4.81 g/
Globulin 2.35 gm/dL
Albumin: Globulin 2.05
Alkaline Phosphatase 99.82 U/L
ALT/ SGPT 51.60 U/L
AST/ SGOT 32.95 U/L
Gamma GT (GGT) 12.95 U/L
Total Cholesterol : 197.84 mg/dL
HDL : 46.50 mg/dL
LDL: 120.19 mg/dL
non-HDL : 151.34
VLDL : 31.15 mg/dL
Triglycerides : 138.30 mg/dL
Medicines advised:
1) Udiliv
2) Rifagut 400
3) DDR 30
4) Betonin syp.
Kindly provide your feedback .
Thanks
Kumar
Your bilirubin level is slightly raised. SGPT also is mildly raised. HDL is fine, but you can still increase by exercise. HDL is good cholesterol and prevents blood vessels damage. If you can decrease LDL below 100 mg/dL and also triglycerides. This will be good for your heart. I can not comment on the medication.
Thanks for your kind words Doctor, Benign Hyperbilirubinemia is anything need to concern or worry. What kind of treatment i need to further go ahead and advice on the diet to follow doctor please. Benign hyperbilirubinemia i am little worried Doctor, is it anything serious on this. Please help and guide please
Thank you so much for the feedback sir.
Hello Doctor.. I did LFT and my findings are –
Total Bilirubin – 1.1 mg/Dl
Direct B – 0.4mg/dl
Indirect B – 0.7mg/dl
Sgot- 38 IU/L
Sgpt – 44 IU/L
What is the probable disease and next steps if you can suggest pls.. I had Covid omicron and also I’m occasionally alcoholic
Your LFT is in the normal range. Except SGPT is the upper normal. I will suggest eating more fruits, and off and on, don’t drink alcohol because it can cause injury to liver cells.
Good day doctor, I am treating hbv with tenofovir, my total bilirubin is 15.59, conjugated bilirubin is 6.6, ast is 32.9, alt is 35.9, alkaline is 90, albumin is 4.4, total protein is 7.1, should I worry?
Hi Doctor
I did test for lipid profile. Here are the results:
Bilirubin (Total) 14.2 μmol/L
Bilirubin Direct 5.7 μmol/L
Total Protein 72.5 g/l
Albumin serum 47.3 g/l
Alkaline Phosphatase 84 IU/L
ALT/ GPT 38 IU/L
AST/ GOT 24 IU/L
Total Cholesterol : 5.04 mmol/L
HDL : 1.13 mmol/L
LDL: 3.63 mmol/L
Triglycerides : 1.22 mmol/L
.Also I did Fibroscan for liver and it show the following results:
CAP measurement = 261 (S2 level)
Fibrosis reading = 6 (F1 Stage)
I did LFT tests for different time but why still showing Direct Bilirubin =5.7 above the normal range (0-5.1)
Thank you
Dear Ahmad Issa
Your all test favors the possibility of Dubon Jhonson syndrome or Crigler Najjar syndrome type 2. You have basically unconjugated hyperbilirubinemia. Dubon Jhonon syndrome is less likely because, in this syndrome, bilirubin is usually <4 mg/dL; rarely, it may go high. Please ask your physician to work for Crigler Najjar syndrome type 2.
My baby has total bilirubin of 1.6,please can I go ahead and administer the bcg injection on her?9
1.6 bilirubin slightly raised. I hope other liver function tests are normal. What is the age of the baby?. I think you can wait for a few weeks.
A.S.A ( Dr. Riaz )
I wanna to know the condition is normal?
Patient age (23)
In LFTs
-Total bilirubin is 0.9 mg/dl
But
-Direct bilirubin 0.0 mg/dl
-Indirect 0.0 mg/dl
And remaining all values normals…..,
Sir tell me condition ….. jazakallah
WAS: Bilirubin is in the normal range. No need to worry.
Hello, I have the 3 bilurubins elevated over the range, I have upper right side of my abdomen, swollen abdomen, swollen face, etc. pain, … what could the 3 elevated bilirubins could be suggesting? Thank you!!
3 mg/dl level of bilirubin is high. It would help if you had an abdomen ultrasound and needed a consultation with the physicians. Please check the complete liver function tests and viral hepatitis profile.
37 male
Total bilirubin 1.8
Protein 7.1
Albumin 4.7
Alt 28
AST 19
All phos 46
Ratio 2.0
Have been dieting low carb/intermittent fasting for a month & lost 25lbs/8% recently, have been under a little stress so appetite is down a little but no other symptoms. Any worries?
All your tests are normal, except total bilirubin is 1.8 mg/dL, slightly more than normal values. Please repeat bilirubin along with AST and ALT after one month.
Female 32 age .my total bilirubin is 0.70 direct 0.60.indirect 0.10 .SGPT 18.SGOT 25.0.alkaline phosphate 81.00.protein total7.00.albumin 4.20.globulin 2.80. AG ratio1.5.slight itching.slight dark urine..my cholesterol total 237.. kindly tell me..
Except for cholesterol, other blood tests are in the normal range. Itching may be due to some skin issue; consult a dermatologist. As regards cholesterol, please exercise and control your diet.
Hi Sir,
can you please reply your mail id, i will forward my uncles report.Total bilirubin is 15 mg/dl
[email protected]. But you can write reports here also.
Thank you sir for the clear explanation!
I have a question.
If
total Bi=direct + indirect
Can you also say
total Bi=UCB+CB?
And also is Delta bilirubin different from indirect bilirubin bound to Albumin for transportation?
UCB+CB = Total bilirubin. While delta-bilirubin is different and is protein bound.
Hello doctor, I’m a medical student and I have a question please. How to differentiate between the 2 types of hyperbilirubinemia based on the lab values? I mean direct Bi increases obviously in direct hyperbilirubinemia (e.g. biliary obstruction) but it also increases in indirect hyperbilirubinemia (e.g. hemolysis). Is there a cut-off value or percentage for direct bilirubin above which we can say it’s direct hyperbilirubinemia pattern and below which we can say it’s indirect hyperbilirubinemia pattern?
In case of biliary obstruction, there is increased Alkaline phosphatase, which will be normal in hemolysis.
Hi, Doctor, Mine
BILIRUBIN, TOTAL 1.35 mg/dL
ALKALINE PHOSPHATASE 121 U/L
GAMMA GLUTAMYL TRANSFERASE (GGT) 91 U/L
BILIRUBIN, DIRECT 0.37 mg/dL
BILIRUBIN, INDIRECT 0.98 mg/dL
TOTAL PROTEIN 7.9 g/dL
ALBUMIN 4.8 g/dL
GLOBULIN 3.1
ALBUMIN/GLOBULIN RATIO 1.6
ASPARTATE AMINOTRANSFERASE (AST/SGOT) 40 U/L
ALANINE AMINOTRANSFERASE (ALT/SGPT) 85
Kindly suggest Am i have any liver function problem?
SGPT is raised, which indicates liver cell injury. Please check your viral hepatitis profile, and have ultrasonography. You need a consultation with a physician. Please repeat the test after 1 to 3 months.
My newborn baby has Albumin bilirubin of 2.3 mg/dl , Total bilirubin of 4.5 mg/dl and Direct bilirubin of 2.2 mg/dl. Is my baby okay?
Please let me know the age of the baby. In newborn babies, if jaundice appears after a few days, it is called physiologic jaundice and only needs phototherapy (tube light or sun).
If jaundice appears in the first 1 to 2 days, it is pathological jaundice. In that case baby needs workup.
Dear Doctor,
My son aged 16 identified with jaundice couple of months before and sharing the blood results.
Total Bilirubin = 3.2 —- 4.88 last month (May 2023) it has come down to 3.2
Bilirubin Direct =1.0 — from 2.0 last month (May 2023) it has come down to 1.0
Bilirubin Indirect= 1.4 — from 1.6 last month (may 2023) it has come down to 1.2
Hepatitis A,B,C all are negative
Abdomen scan on liver and spleen mild enlarge initially and it has come down normal in recent reports
SGOT (AST) – 29
SGPT(ALT) – 35
ALP – 102
He is currently taking Liv 52 DS(30 days – 60 tabs), Ferrodal syrup(15 days), Silybon 70 (15 days 30 tabs) based on the advice from our (general physician). His eyes are slight yellowish in both side. I took the billirubin test from other lab it was shown as total bilirubin – 1.50 – Direct bilirubin – 0.20 and Indirect bilirubin – 1.30 (23-May 2023)
Could you please suggest the next set of actions?
Thanks
N Satheesh
Your son SGOT/SGPT are normal. There is increased indirect bilirubin. So please ask you physician to exclude Hereditary jaundice like Gilbert’s syndrome.
Thanks a lot Doctor.
Sir Asalam o alikum
Sir my age 38
Total bilirubin 3.2 mg/dl
SGPT (ALT) 14 U/L
SGOT (AST). 17 U/L
Alkaline phosphatase 46 U/L
Hepatitis ABC all negative
All test clear but my bilirubin isn’t going down more than 15 years. how will it decrease plz help I apply Qatar visa my medical will be cleared or not
Sir Asalam o alikum
Sir my age 38
Total bilirubin 3.2 mg/dl
SGPT (ALT) 14 U/L
SGOT (AST). 17 U/L
Alkaline phosphatase 46 U/L
Hepatitis ABC all negative
All test clear but my bilirubin isn’t going down more than 15 years. how will it decrease plz help I apply Qatar visa my medical will be cleared or not.
Doctor said Genetic problem and there is no treatment for it.
Your other liver tests are normal. If jaundice is not disappearing for the last 15 years. Please consider the hereditary (Congenital) bilirubinemia.
Dear Sir,
Assalam Alaikum,
Age: 34 Years
Height: 5.7
Weight: 79 Kg
I have had jaundice 18 years ago I had gone through the treatment and was recovered. But my eye color turned to yellow and my skin turned dark and dull as well. I.ve been living with yellow eyes and dull skin complexion for the last 18 years.
But this didn’t effect my overall health. I was and still active all the time. I do a lot of aerobics exercise like jumping ropes, weight lifting. Overall I am more active and strong as compared to others.
But few days ago, I started getting Cyctic Acne(Which contains pus) on my face and body which got worst after days. A doctor advised me to go for LFT test.
below is the LFT test result from DOW Lab:
LFT Test
S. Total Bilirubin: 0.47 mg/dl
S. Direct Bilirubin: 0.19 mg/dl
S. Indirect Bilirubin: 0.28 mg/dl
SGPT (ALT): 36 U/I
Alkaline Phosphatase: 163 U/I
Gamma GT: 26 U/I
SGOT (AST): 22 U/I
Can you please tell me about my Liver condition. Will it be cured after medications or I am in the danger zone?
Thanks & Best Regards,
Hamid Nisar
Your liver functions are normal. I do not see any abnormality in this LFT.
Many thanks for your quick response!
but my LFT indicates 3 things
(i) Alkaline Phosphasate 163.
(ii) Direct bilirubin: 0.19
(iii) Indirect Bilirubin: 0.28
mentioned above readings are high. What do you think, wouldn’t that be a problem in future?
Hello Dr Riaz,
This is absolutely a brilliant article, totally complete and most relevant information. Thanks for sharing.
I am one of the dr, who works in remote village area and see lots of prolonged jaundice babies. Due to low economic reasons, I have to really think and see which important tests, I need to do. Is it possible to speak to you or email you. Could you please share your email or any way to contact you please. Thanks.
Thanks for the comments. You can email me, [email protected]. I am living in USA. You can leave message on whatsapp (+16085723654)
Hi Dr, i recently got a blood test done for bilirubin and found my bilirubin to be 1.31 mg/dl. Can this condition be checked with diet precautions or do you suggest the need to get more tests done?
Please repeat your bilirubin level after 1 to 2 months. Meanwhile eat more fruits.
Hi Dr. I am 46 year male recently blood test and found, total serum bilirubin 1.26 mg/dl, serum bilirubin total 1, SGPT, SGOT is normal, plz suggest
Your bilirubin level looks to be in normal range. In case if you are worried, please repeat bilirubin after one month. Your SGPT/SGOT are normal which negate liver cell injury.
Hello Dr. Riaz,
Hope you’re doing well. I am a 21 year old male with asymptomatic raised bilirubin levels. No known co-morbids. No itching, no discolouration, normal urine, normal bowel. Slight fatigue, if I compare it with my previous energy levels, I think I get tired slightly more quickly. Otherwise, no symptoms whatsoever.
Here is my medical record:
12/01/2022:
Total Bilirubin: 30 umol/l
ALT: 19 U/L
ALP: 98 U/L
Albumin: 50 g/l
12/07/2023:
Total Bilirubin: 42 umol/l
ALT: 26 U/L
ALP: 66U/L
Albumin: 51g/l
14/08/2023:
Total Bilirubin: 1.9mg/dl
Direct Bilirubin: 0.59mg/dl
Indirect Bilirubin: 1.31 mg/dl
ALT: 19 U/L
AST: 19 U/L
ALP: 90 U/L
GGT: 12 U/L
Total protein: 7.1 g/dl
Albumin: 4.9 g/dl
Globulin: 2.2 g/dl
Albumin to Globulin ratio: 2.2
Your indirect bilirubin is slightly raised. This may be hereditary type of bilirubinemia. But I will suggest repeating liver function tests after 2 months. Meanwhile take abundant fruits.
Thank you for your response. The direct bilirubin also seems to be high, the range mentioned in the report is 0 – 0.25mg/dl. Is that fine? Also, I forgot to mention before please note that some values are in different units due to tests being conducted at different lab facilities.
Any fruits in particular? And will vitamin supplements be of any help?
Thank you in advance!
Sir I am preparing for the Defense service but in medical I got declared unfit due to indirect Hyper Billirubin …… Sir my weight is increasing , but indirect billirubin is fluctuating too much some time it becomes 0.5 and sometimes it’s become 3.0 and sometimes 2.2 sir what I do please suggest any medicine or treatment
You have genetic abnormality which is the cause of benign hyperbilirubinemia. Tab barbiturate may help to decrease the bilirubin. Other method is phototherapy.
My baby recently hv jundice now also she look yellow and my baby age was 41 days my baby total bilirubin level is 14.22 mg/dl
Direct bilirubin is 0.47 mg/dl
Indirect bilirubin is 13.75 mg/dl
Its normal are high what should i do pls help
Your baby jaundice still present (41 days), it is pathological jaundice. There is possibility of Crigler-najjar syndrome and Gilbert’s syndrome. Please consult hepatologist or gastroenterologist.
Hi doctor
My total bilirubin is -1.88 mg/dl
Direct bilirubin is- 0.69 mg/dl
Indirect bilirubin is -1.19 mg/dl
SGPT/ALT -84 U/L
SGOT/ASP-57 U/L
Your bilirubin i mildly elevated, but SGPT is high, while SGOT is also mildly raised. One can say that these liver functions are abnormal. You need more workup like gama-GT and Ultrasound abdomen. Check your HBV and HCV viral profile. If needed consult hepatologist/gastroenterologist or some good physician.
I recently did LFT
Total bilirubin 1.14
direct bilirubin 0.19
Indirect bilirubin 0.95
SGOT 22.90
SHPT 16.9
ALP 72.90
GGT 15.1
Total protein 7.92
Can you please tell me what is to be done?
Only total bilirubin is slightly more than the normal value. All other tests are normal. Please repeat LFT after one month. Meanwhile eat more fruits. I will suggest that this LFT is normal. Please relax.
Total bilirubin is 1.14 so I think that comes under normal range right? And indirect has slightly increased I.e 0.98?
My bro in law..Age 35 …please Suggest ..Hepatitis ..A…Cholestatic ..Jaundice….Total Bilirubin 30.5
Direct 15.6
Indirect 14.9
SGOT ..AST..170
SGPT ..ALT ..146
ALP ..271
Anti HCV Non reactive
HBSAg negative
PT INR 1.49
Renal Functional Tests all Normal
Total Proteins..Albumin,Globulin are Normal
GGT Normal..I.e.35
MCV 81.1…. Low
RDW 20.3 .. high
MPV 14.1….High …please needed Suggestion
Total bilirubin is too high, but SGOT/SGPT not corresponding to bilirubin level. Alkaline phosphatase is not too high which should be high in obstructive jaundice.
Please repeat LFT from good, reputed laboratory. You can check for Anti-HAV IgM level to rule out hepatitis A.
Please also check blood urea and creatinine to rule out hepatorenal syndrome.