Electrolytes:- Part 2 – Sodium (Na+), Blood and Serum
Sodium (Na+)
What sample for Sodium (Na+) is needed?
- This test is done on the patient’s serum.
- A random sample can be taken.
- Heparinized plasma and whole blood without sodium heparin may be used.
- Twenty-four hours of urine samples may be collected without the addition of preservatives.
- Can store the serum or urine at 2 °C to 4 °C.
- Other samples can be:
- Feces.
- Sweat.
- Gastrointestinal fluids.
What precautions will you take for the estimation of Sodium (Na+)?
- Avoid hemolysis (Although it does not cause much difference in serum or plasma sodium values).
- Lipemic serum must be ultracentrifuged before direct-selective electrodes measure Sodium.
What are the Indications for Sodium (Na+)?
- This is the patient’s routine workup.
- This is done to evaluate electrolytes and acid-base balance.
- To evaluate water intoxication, water balance, and dehydration.
- It is estimated that it takes to diagnose and treat dehydration and overhydration.
How will you describe the Pathophysiology of Sodium (Na+)?
- Sodium is the major cation of the extracellular fluid. It has a major influence on plasma osmolality.
- It is adjusted by the anti-diuretic hormone (ADH) and thirst receptors to maintain plasma volume and osmolality.
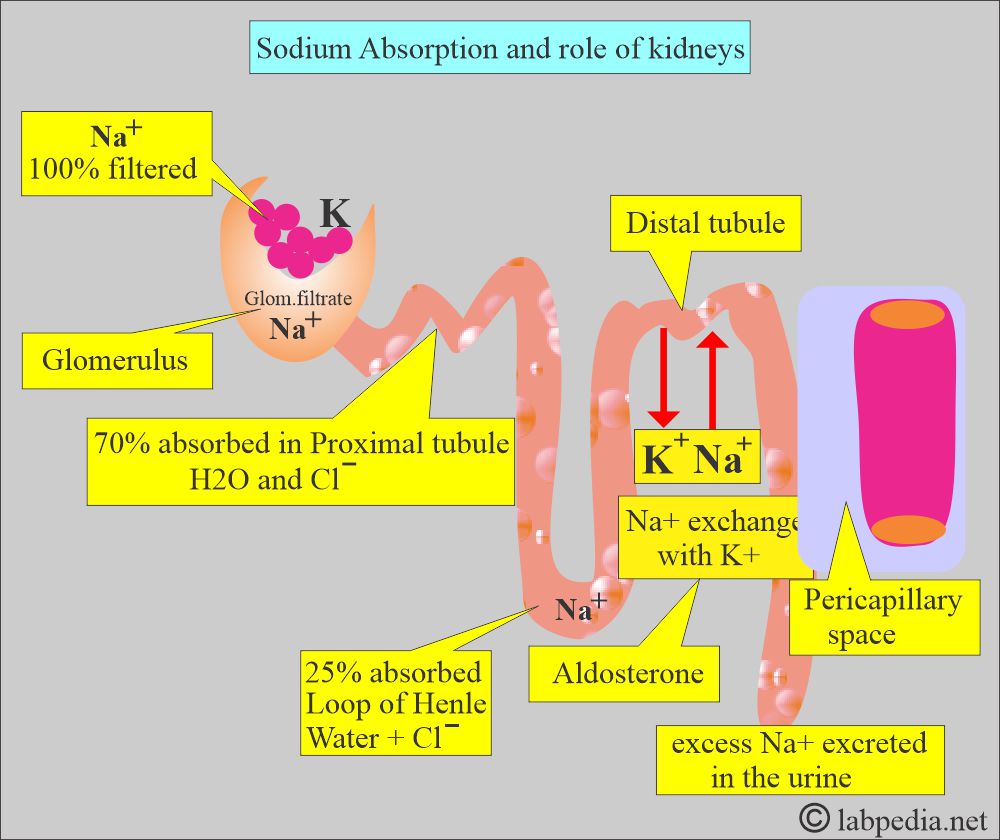
- Aldosterone causes tubular reabsorption of Sodium.
- Changes in the serum sodium reflect changes in water balance rather than sodium balance.
- Sodium has a significant quantitative effect due to its influence on electric neutrality.
What are the sources of Sodium (Na+)?
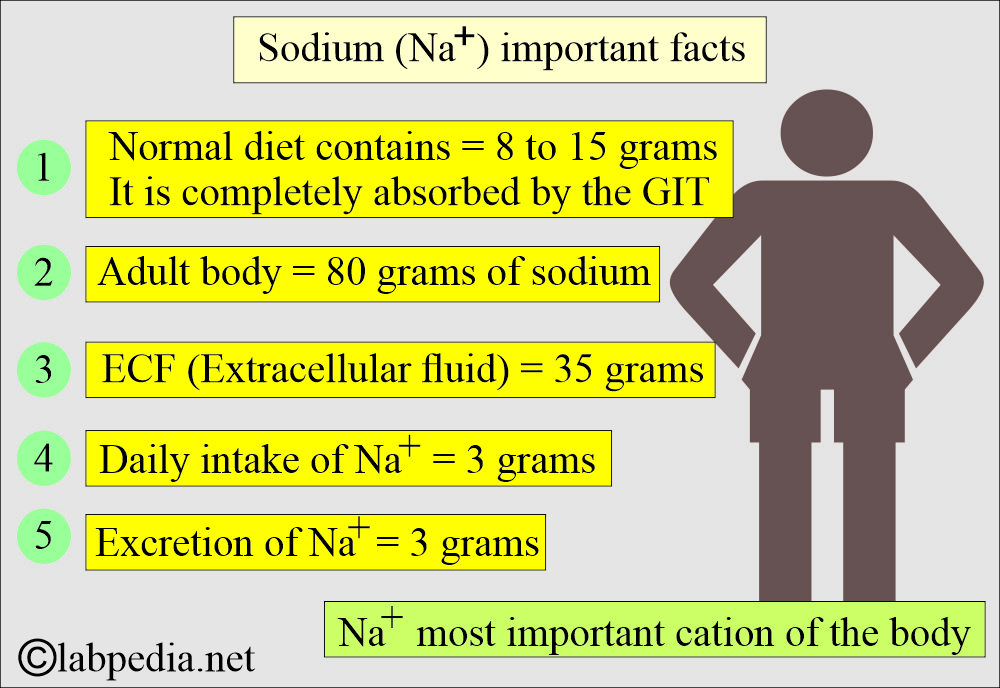
- The average adult body contains 80 grams of Sodium.
- 35 grams are present in the extracellular fluid.
- The average person consumes 3 grams of Sodium daily in the form of chloride, sulfate, and other salts.
- Also, excrete the same amount of 3 grams per day.
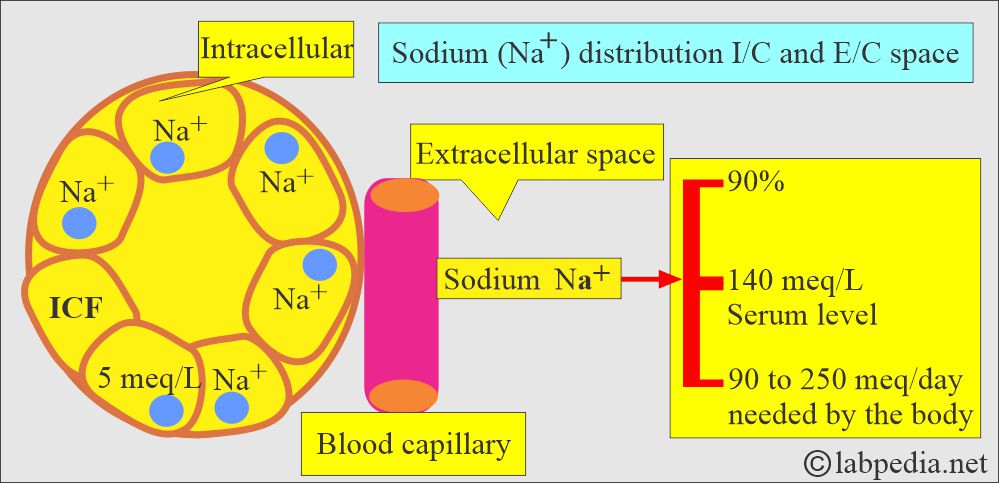
- Dietary need of Sodium = 90 to 250 meq//day.
- The normal daily diet contains 8 to 15 grams of NaCl, which is completely absorbed in the gastrointestinal tract.
- Sodium is the most common cation in the blood by almost 90%.
What is the role of the kidneys in Sodium (Na+) absorption?
- 100% of Sodium is filtered through the glomerulus.
- 70% to 80% is reabsorbed in proximal tubules (water and chloride).
- 20% to 25% is reabsorbed in the loop of Henle (with water and chloride).
- Kidneys are the body’s main regulator of sodium, which is excreted in excess.
What is the Distribution of the Sodium (Na+) in the body?
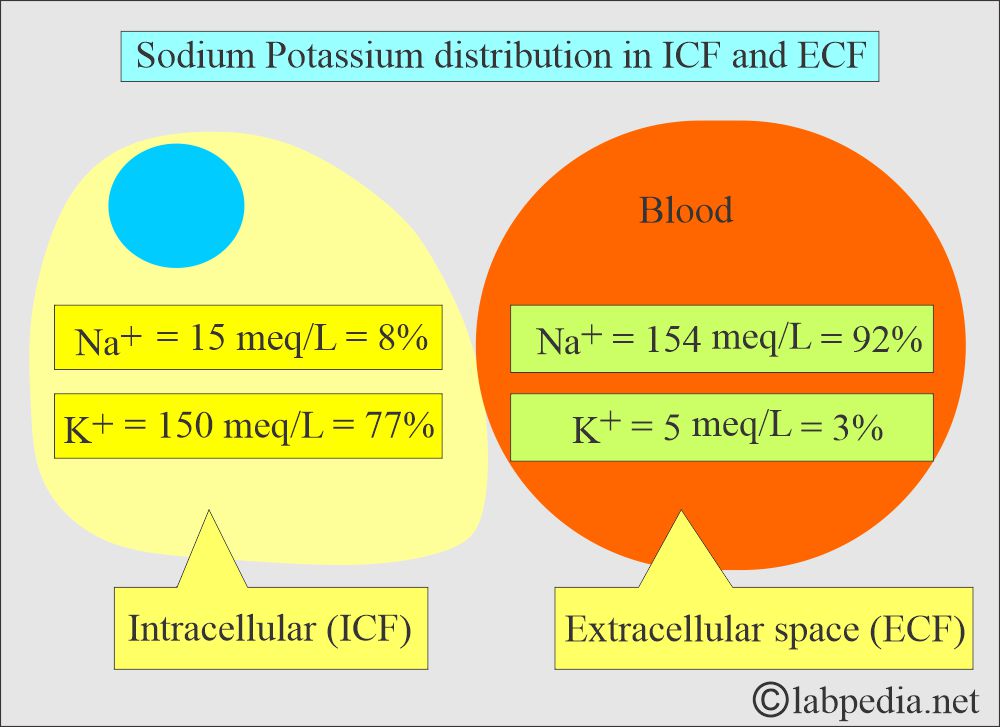
- The sodium level is the reverse of Potassium.
- Sodium 140 meq/L extracellular and 5 meq/L intracellular.
- Because Sodium is actively pumped out of cells, the concentration of Na+ reflects the Intracellular volume.
What are the Functions of the Sodium (Na+)?
- Sodium is a major component of extracellular osmolality. It is almost half the osmolality of the plasma.
- So, Sodium’s main function is to maintain osmotic pressure and acid-base balance.
- Sodium also helps to transmit nerve impulses.
- Sodium, along with potassium and calcium, maintains neuromuscular irritability for the conduction of nerve impulses.
- Sodium helps in the acid-base balance through sodium bicarbonate and sodium phosphate.
- Sodium participates in cellular chemical reactions and in membrane transport.
- The body can maintain Sodium very well except for a few pathological conditions.
How will the body maintain the sodium (Na+ ) level?
- Maintenance of sodium level depends upon the following:
- Renal blood flow.
- Carbonic anhydrase activity.
- Aldosterone.
- Other steroid hormones can control through:
- Anterior pituitary gland.
- Renin enzyme secretion.
- Antidiuretic hormone ( ADH ).
- Vasopressin secretion.
- Sodium level is a result of the balance between dietary intake and renal excretion.
- Aldosterone acts by:
- Stimulating the Kidney to conserve Sodium.
- Decrease renal loss of Sodium.
- Antidiuretic hormone (ADH) controls:
- Reabsorption of water at distal tubules.
- .This will be affected by the concentration or dilution of Sodium.
- Physiologically, Sodium and water are interlinked.
- Increased free body water = Sodium diluted, Na+ concentration decreases, Kidney conserves Sodium and excretes water.
- Decreased free body water = Serum sodium will rise, and now the kidneys will conserve water. Na+ level became normal.
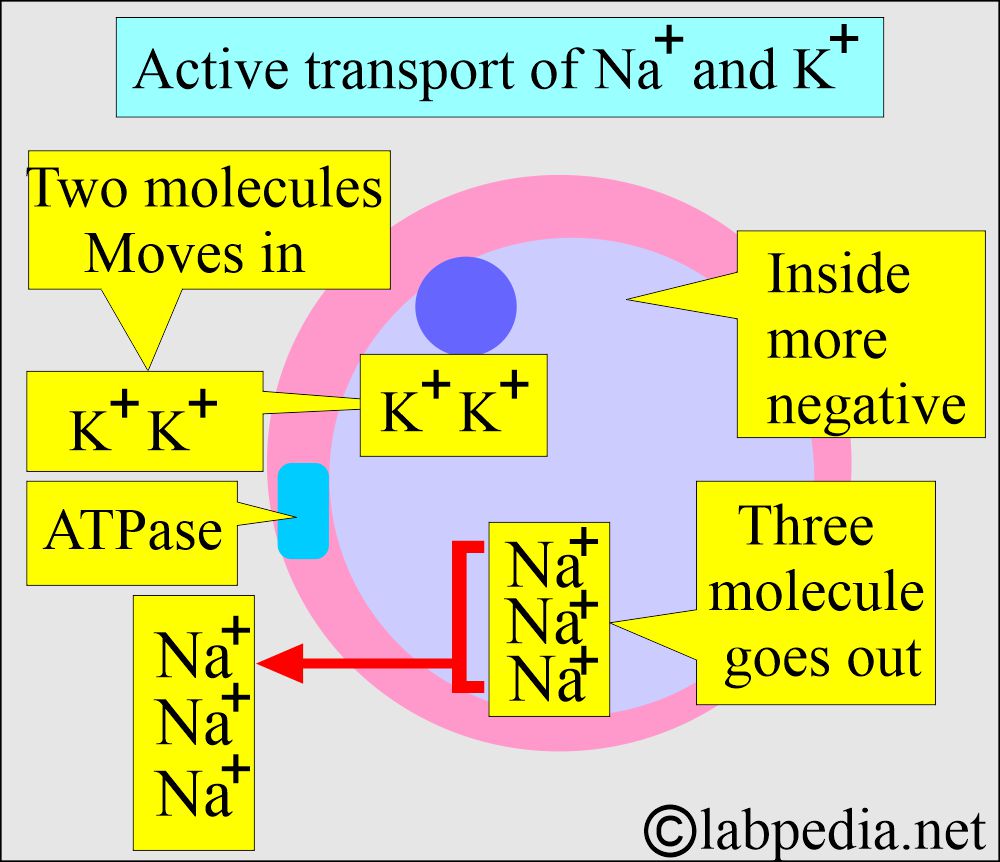
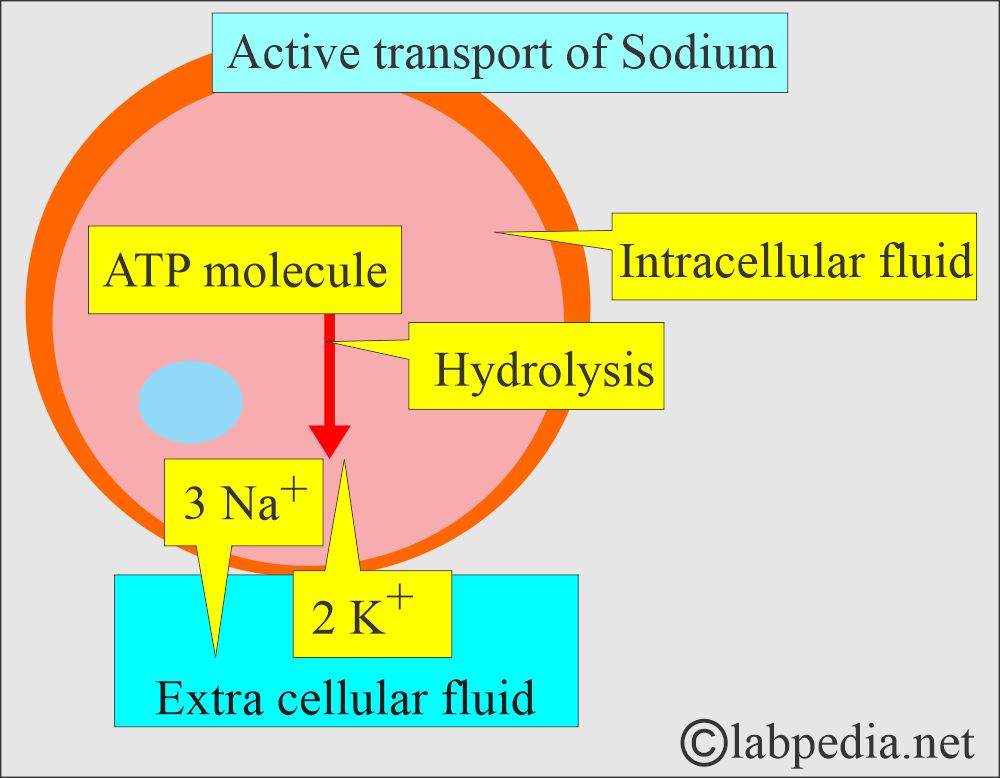
How will you describe the Active transport of Sodium (Na+)?
- This is found in most cells, especially muscles and nerves.
- The excitable tissue has high concentrations of Na+, K+, and ATPase.
- With the help of the ATPase enzyme in the cell membrane, three molecules of Na+ go out, while only two molecules of K+ go in.
- So, the inside is negatively charged.
What are the Signs/Symptoms of Hyponatremia?
- When the level is <125 meq/L (<135 mmol/L).
- <120 meq/L is severe hyponatremia.
- The patient will feel weak.
- When Level <115 meq/L.
- The patient will have confusion and lethargy.
- May progress to a stupor and coma.
- There is a decreased glomerular filtrate rate, as seen in congestive heart failure.
- Hyponatremia is seen in the case of:
- Low salt intake.
- There is premenstrual retention of Sodium and water.
- Adrenocortical hyperfunction.
- Hyperaldosteronism.
What are the Signs/Symptoms of Hypernatremia?
- >160 meq/L is the critical value for the patients.
- The patient will have dry mucous membranes.
- Thirst.
- Agitation and restlessness.
- Hyperreflexia.
- Mania and convulsion.
- There is increased excretion of Sodium in the urine.
- Hypernatremia is seen in the following conditions:
- Hypoaldosteronism.
- Adrenal failure.
- Diuretic therapy.
- Salt-losing nephritis.
- Physiologically, there is increased salt intake.
What is the NORMAL level of Sodium (Na+)?
Source 1
| Age | meq/L | |
| Premature cord blood | 116 to 140 | |
| Premature by 48 hours | 128 to 148 | |
| Newborn cord blood | 126 to 166 | |
| Full-term | 133 to 146 | |
| Infants | 139 to 146 | |
| Child | 138 to 145 | |
| Adult | 136 to 145 | |
| >90 years | 132 to 146 | |
| Urine 24 hours | meq/day | |
| Male | Female | |
| 6 to 10 years | 41 to 115 | 20 to 69 |
| 10 to 14 years | 63 to 177 | 48 to 168 |
| Adult | 40 to 220 | |
| Sweat | meq/L | |
| Child and adult | 10 to 40 | |
| Cystic fibrosis | 70 to 190 | |
| Feces | <10 (7.8 ± 2) | |
| Saliva | meq/L | |
| Without stimulation | 6.5 to 21.7 | |
| After stimulation | 43 to 46 | |
| CSF | 136 to 150 | |
| Amniotic fluid | meq/L | |
| 28 weeks | 124 to `48 | |
| 48 weeks | 115 to 139 | |
- To convert into SI units x 1.0 = mmol/L
Source 2
- Blood/Serum:
- Adult Sodium = 136 to 145 meq /L
- Infants’ Sodium = 133 to 142 meq /L.
- Premature infants = 132 to 140 meq/L.
- Urine Sodium = 40 to 220 meq/day with an average sodium intake of around 8 to 15 grams/day.
- (varies with dietary intake).
- CSF Sodium = 136 to 150 meq/L.
- Feces Sodium = Mean value is <10 meq/day.
What are the Causes of Hypernatremia (Increased serum Sodium (Na+)?
- Hypernatremia clinically may have a presentation of:
- Hypovolemic patients who have hypotension, tachycardia, and poor skin turgor.
- Euvolumic patients have normal blood pressure, normal pulse, skin turgor, and no edema.
- Hypervolemic patients show edema.
- Dehydration.
- Insufficient water intake.
- Hormone causes are:
- Primary aldosteronism (Adrenal insufficiency).
- Adrenal hyperplasia.
- Cushing’s syndrome.
- Diabetes insipidus.
- Steroid therapy.
- Coma.
- Excessive Sodium in Intravenous Therapy.
- Skin is loose, like excessive sweating and burns.
- Vomiting.
- Extensive thermal burns.
- Loss from the GI tract.
- Use of diuretics.
- Pulmonary losses like hyperventilation.
What are the causes of Hyponatremia (Decreased serum Sodium (Na+)?
- Hyponatremia patients may have clinical presentations like;
- Hypovolemic patients will have hypotension, tachycardia, and poor skin turgor.
- Euvolumic patients will have normal blood pressure, normal pulse, skin turgor, and no edema.
- Hypervolumic patients will have edema.
- Deficient dietary intake.
- Decreased Sodium in the I/V therapy.
- Diuretics.
- Chronic renal insufficiency.
- Aspiration of pleural or peritoneal fluids.
- Excessive water intake.
- Congestive heart failure.
- Ascites.
- Pleural effusion.
- Ectopic secretion of ADH.
- Pyloric obstruction.
- Malabsorption syndrome.
- Diabetic acidosis.
- Hypothyroidism.
- Nephrotic syndrome.
- Absolute loss of Sodium from the body:
- Prolonged vomiting.
- Excessive sweating.
- Prolonged diarrhea.
How will you describe Hyponatremia (Sodium (Na+) when the patient is hypovolemic?
- Renal losses due to:
- Diuretics
- medullary renal disease
- Addison’s disease
- External losses due to:
- Gastrointestinal losses
How will you define Pseudohyponatremia?
- This condition is usually caused by an excess of lipids in the serum. Serum sodium ions are not dissolved in the lipids.
- The following are the causes of pseudohyponatremia:
- Hyperglycemia
- Hyperlipidemia
- Hyperproteinemia
Sodium (Na+) level in blood and urine in various conditions:
| Various clinical conditions | Sodium (Na+) level in the blood | Sodium (Na+) level in urine |
| Diarrhea | Decreased | Decreased |
| Dehydration | Increased | Increased |
| Malabsorption | Decreased | Decreased |
| Starvation | Normal | Normal or Increased |
| Excessive sweating | Decreased | Decreased |
| Pyloric obstruction | Decreased | Decreased |
| Congestive heart failure | Normal or decreased | Decreased |
| Pulmonary emphysema | Normal | Decreased |
| Acute renal failure | Decreased | Decreased |
| Chronic renal failure | Decreased | Increased |
| Renal tubular acidosis | Decreased | Increased |
| Primary aldosteronism | Increased | Decreased |
| Adrenal cortical insufficiency | Decreased | Increased |
| Diabetic acidosis | Decreased | Increased |
| Diabetes inspidus | Normal or increased | Normal |
| Thiazide diuretics | Decreased | Increased |
| Mercurial diuretics | Decreased | Increased |
| Diamox (Acetazolamide) | Decreased | Increased |
What is the Critical value when the patient needs an immediate intervention?
- Na+ <120 meq/L. The patient will have weaknesses and neurologic symptoms.
- Na+ >160 meq/L. This may cause heart failure.
What precautions should be taken to correct hyponatremia?
- Too rapid a correction of hyponatremia can lead to central pontine myelin-lysis.
- The too-slow correction will lead to cerebral edema.
Questions and answers:
Question 1: What are the critical values of serum Sodium?
Question 2: What is the explanation of the pseudohyponatremia?
Note: Please see more details on Serum electrolytes.