Rheumatoid Factor (RF), Rheumatoid Arthritis (RA factor)
Rheumatoid Factor (RF)
What sample is needed for the Rheumatoid Factor (RF)?
- This is done on the patient’s serum; a fresh sample is preferred.
- A random sample can be taken.
- The sample can be stored at 2 to 8 °C for 24 hours.
What are the precautions for Rheumatoid Factor (RF)?
- Do not use plasma.
- Older adults have a false-positive result.
- Lipemic serum and hemolysis give false-positive results.
What are the Indications for Rheumatoid Factor (RF)?
- For the diagnosis of Rheumatoid arthritis.
What are the facts about Rheumatoid arthritis and Rheumatoid Factor (RF)?
- The etiology of rheumatoid arthritis is unknown.
- Genetic factors are important, as are hormonal and psychosomatic factors.
- There is evidence that immunologic factors are involved in both articular and extraarticular manifestations.
- In general, its incidence is 1 to 2 % in most populations.
Rheumatoid arthritis:
How would you define Rheumatoid arthritis?
- This chronic inflammatory disease affects joints, especially the metacarpal and phalangeal joints.
- The most common joints are the proximal interphalangeal joints and the wrist.
- This is one of the autoimmune diseases.
- Age: This is seen in 70% of the cases in the second and third decades. The peak age is 35 to 50 years.
- The older age group and being overweight are commonly recognized risk factors for arthritis.
- Sex: This is the disease of females with a male-to-female ratio of 1:3 to 5.
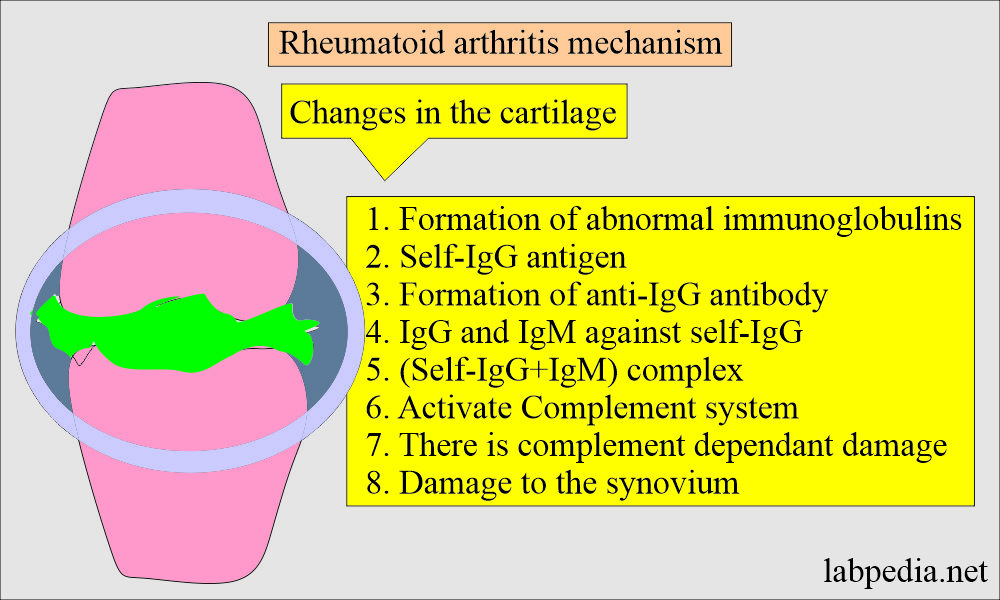
What is the mechanism of injury in Rheumatoid arthritis?
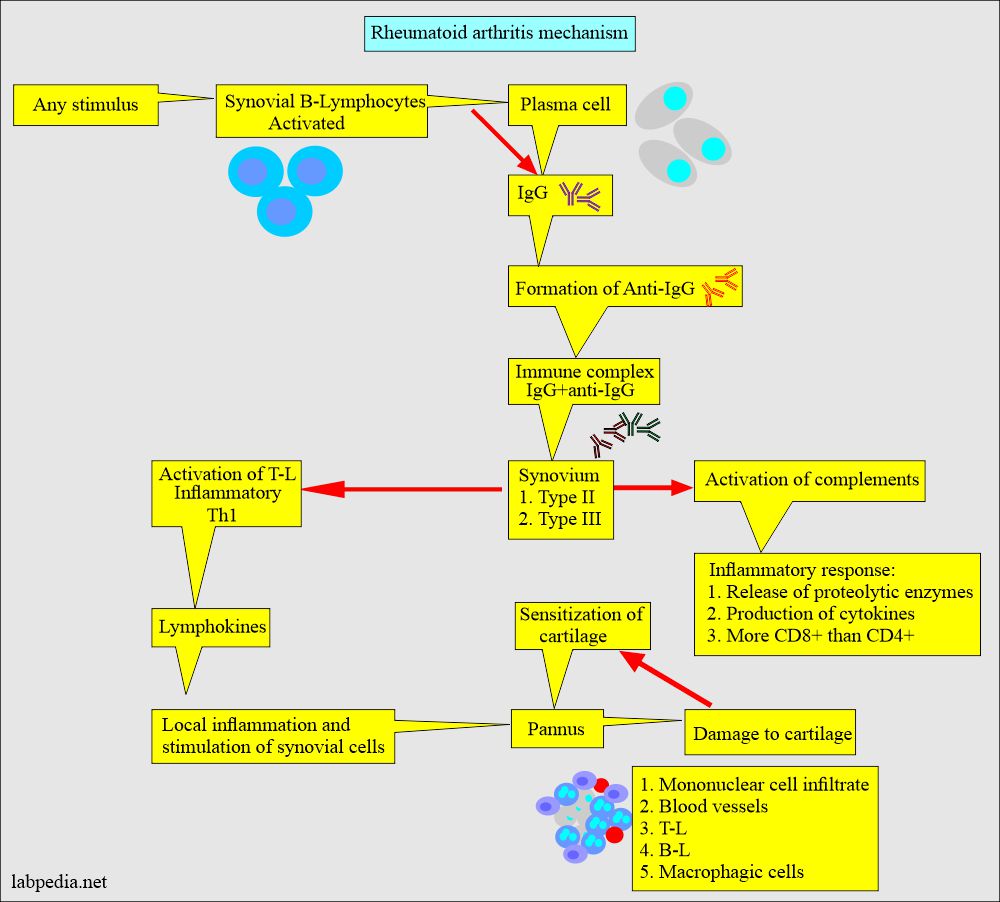
- The mechanism of injury is due to the production of abnormal immunoglobulin IgG against self-antigens.
- Possible antigens are:
- Self- IgG.
- Viral-like EBV may play a role in suppressing Ts or leading to polyclonal activation of B-Lymphocytes.
- Other viruses may be blamed, like Herpes, Rubella, and Mycoplasma.
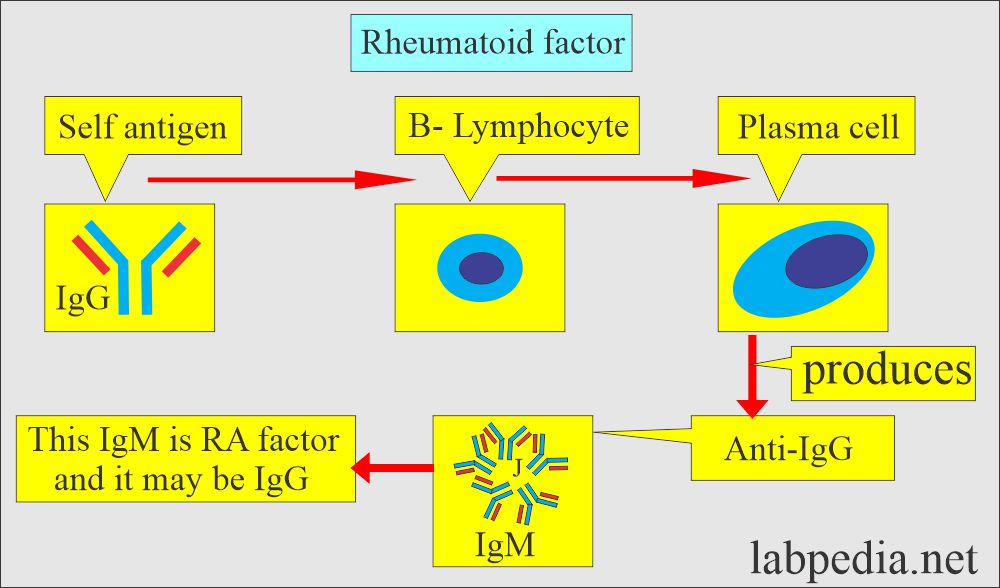
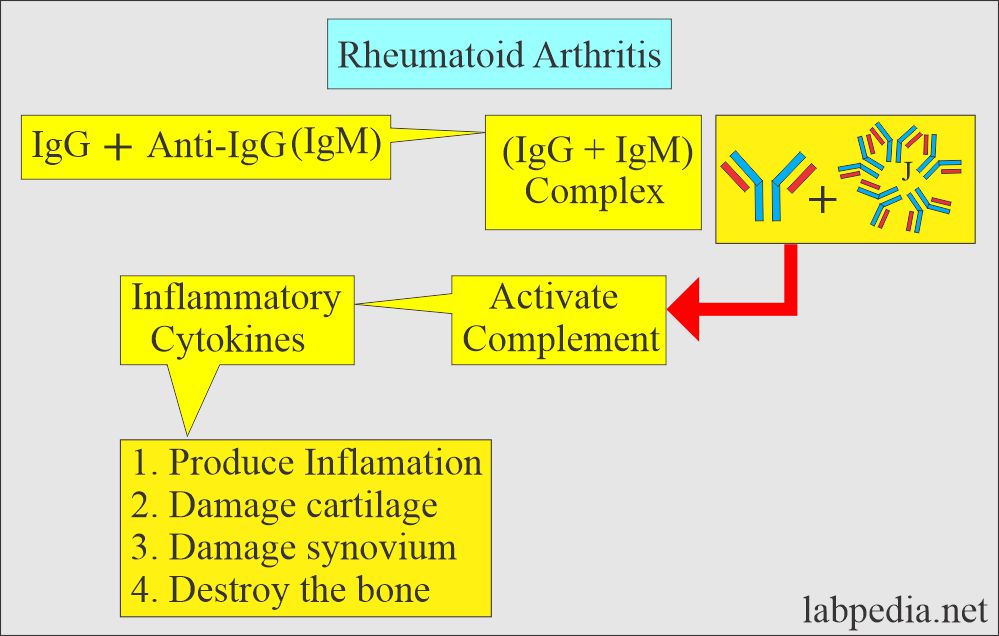
- Synovial lymphocytes produce IgG, which is recognized as foreign and gives rise to the immune complex (IgG + Anti-IgG).
- Anti-IgG and anti-IgM are formed against this abnormal IgG (anti-gamma.-globulin Ab).
- RF antibody is directed against the Fc fragment of IgG, and these are usually IgM.
- RF factor or antibody is not specific for rheumatoid arthritis because it is also seen in other autoimmune diseases.
- These antigen and antibody complexes activate the complement system and cause damage to the synovium.
What is the Mechanism of damage to cartilage and bone?
- Mainly, IgM is the RF Factor, and sometimes IgG and IgA may be the RF factor.
- RF factors such as IgA give rise to very severe diseases when found.
- Tissue other than synovium may be the site of this Ag+Ab complex reaction like :
- Blood vessels.
- Lungs.
- Heart.
- Nerves.
- 80% of the patients are RF factor-positive.
- A negative RF factor does not rule out Rheumatoid arthritis.
What are the Clinical criteria for a diagnosis of rheumatoid arthritis?
- Positive rheumatoid factor (RF positive).
- Morning stiffness for at least 6 weeks.
- Pain in motion or tenderness in at least one joint for the last 6 weeks.
- The common site is the wrist, metacarpophalangeal, and proximal interphalangeal joints.
- Swelling of one joint for at least 6 weeks.
- Symmetrical bilateral joint swelling.
- Subcutaneous nodules (called rheumatoid nodules).
- Typical radiological changes, including bony decalcification.
- Other clinical findings are:
- The patient may have weight loss and fatigue.
- There are ocular abnormalities like the inflammatory lesion of the sclera and the episclera.
- The patient may develop neuropathy.
- There may be cardiac manifestations like pericarditis.
- Pulmonary manifestation is pleural effusion.
- Felty’s syndrome is complex of:
- Rheumatoid arthritis.
- Splenomegaly.
- Anemia, and neutropenia.
- Amyloidosis may develop as a complication.
How will you diagnose Rheumatoid arthritis?
- CBC shows lymphocytosis, thrombocytosis, and raised ESR.
- Synovial fluid examination shows mainly neutrophils (around 75%).
- Radiological findings show a narrowing of the joints.
- Serology: Rheumatoid factor (RF) is positive in >70% of the cases.
How will you perform a Rapid latex agglutination test?
- This reaction depends upon the antibody in the patient’s serum, known as a rheumatoid factor.
- The strength of a positive reaction may be graded as follows:
- 1+ = There is minimal clumping with a slightly opaque background.
- 2+ = Small clumping with a slightly opaque fluid background.
- 3+ = Moderate clumping with a fairly clear fluid background.
- 4+ = Large clumps with a clear, fluid background.
- This test can be done qualitatively by tube test where the serum is diluted.
- The serum can be diluted from 1:20 to 1:640 or 1:5120.
- Add one drop of latex solution (well-mixed).
- Mix all the tubes and incubate at 37 °C for 15 minutes.
- Centrifuge tubes for 2 or 5 to 10 minutes, depending on the centrifuge machine’s revolution.
- Gently resuspend and examine under the microscope for the presence of clumps (macroscopic agglutination).
- This is reported as IU/mL.
What are the American Rheumatism Association criteria?
- American Rheumatism Association has 11 criteria for the diagnosis of Rheumatoid arthritis.
- 7 are required for the diagnosis of classical Rheumatoid arthritis.
- 5 are required for a definite diagnosis.
- 3 are required for probable cause of rheumatoid arthritis.
- Diagnostic tests are:
- Positive rheumatoid factor (RF).
- Poor mucin clotting of synovial fluid.
- Characteristic changes in the biopsy in the synovium.
- Characteristic changes in the rheumatoid nodule.
What is the normal value of Rheumatoid Factor (RF)?
Source 1
- Rh- factor is negative.
- By sheep agglutination test = Negative (1:16)
- By Nephelom = <30 U/mL
Source 2
- Negative (<60 units/mL) by nephelometry.
- Older adults may have slightly increased values.
Another source
- The RF factor is negative.
- 0 to 20 U/mL.
- In the case of titration, then its titer should be more than 1: 80.
What are the conditions where the Rheumatoid Factor (RF) is Positive?
- Rheumatoid arthritis.
- Other autoimmune diseases are SLE, Sjogren’s syndrome, and scleroderma.
- Chronic viral infections.
- Tuberculosis.
- Chronic active hepatitis.
- Syphilis.
- Infectious mononucleosis.
- Leukemia.
- Biliary Cirrhosis.
- Renal disease.
- The antinuclear antibody is positive in 55% of Rheumatoid arthritis patients.
- There are patients with RF-negative arthritis.
Questions and answers:
Question 1: What is the cause of Rheumatoid arthritis?
Question 2: Rheumatoid factor positivity in how many numbers of patients?