Magnesium level (Mg++)
Magnesium level (Mg++)
What sample is needed for Magnesium level (Mg)?
- This test is done on the patient’s serum (3 to 5 mL of clotted blood).
- A fasting sample is preferred.
- Collect blood in the metal-free container.
- Separate the red cells immediately.
- Hemolysis interferes with the test. This may give a falsely high value.
- Magnesium is Stable in blood for 3 hours and in serum at 2 to 8 °C for 8 hours.
- Separate the serum as soon as possible (within 45 minutes).
- Collect the sample in a prone position because an upright position may increase magnesium by 4%.
What are the precautions for Magnesium level (Mg)?
- Avoid hemolysis because it gives a falsely high value.
- Some drugs that give rise to low value are diuretics, insulin, and antibiotics.
- A few drugs that give high values are antacids, calcium-containing medicines, laxatives, and thyroid medicines.
- A fasting sample is preferred.
- Avoid venous stasis.
What are the Indications for Magnesium level (Mg)?
- To evaluate renal function.
- To evaluate the electrolytes.
- To evaluate magnesium metabolism to find deficiency or overload.
How will you describe the pathophysiology of Magnesium level (Mg)?
- Magnesium is the fourth most abundant cation in the body, after sodium, potassium, and calcium.
- Mg concentration in the cell is second to Potassium.
- Extracellular concentration is much lower.
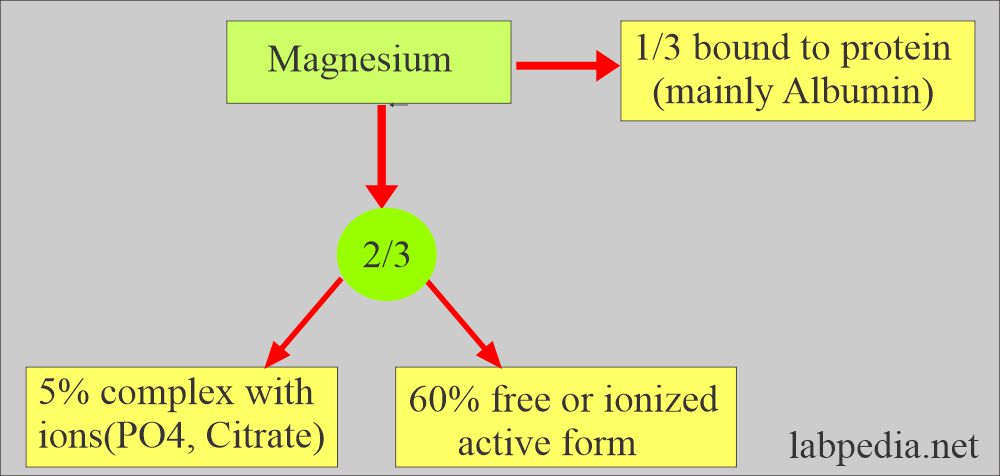
- 30% Mg in plasma bound to albumin.
- 70% Mg exists as the ion Mg++.
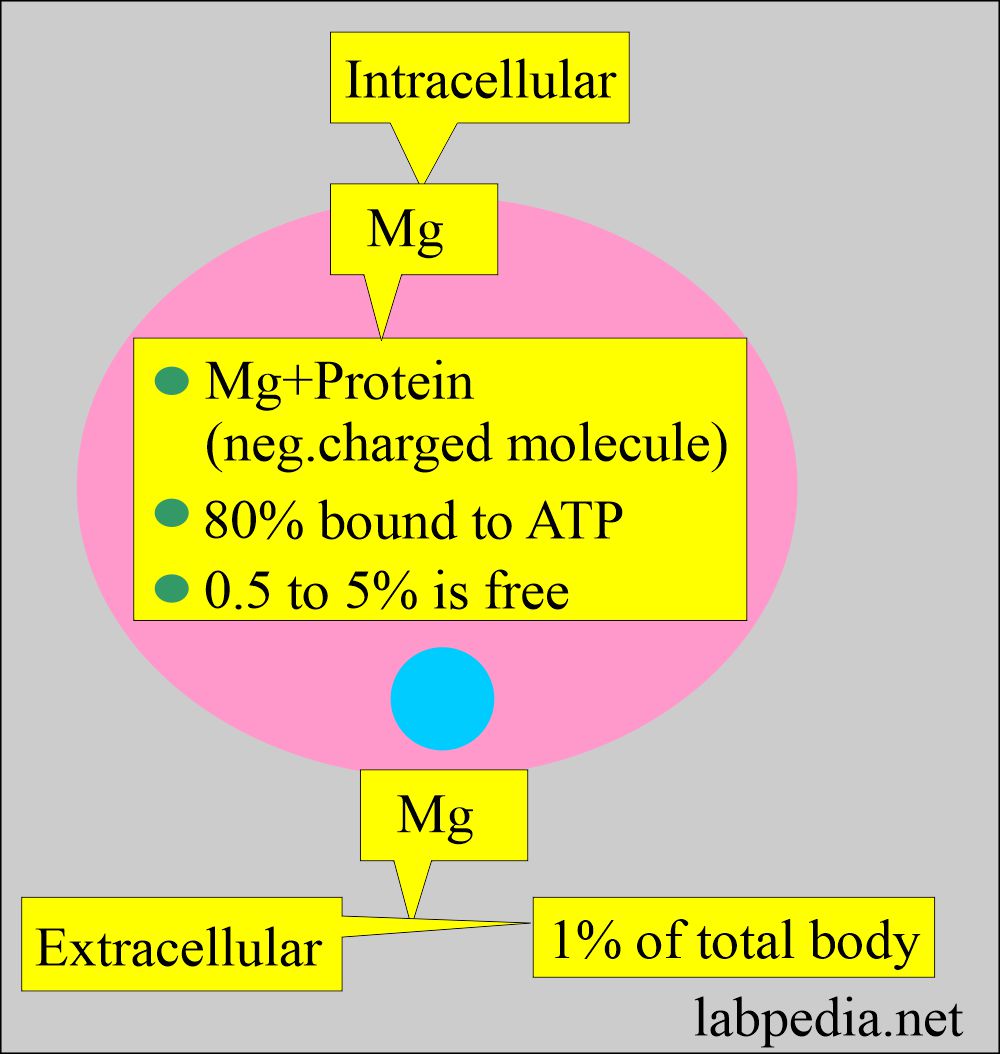
- The majority of magnesium is intracellular.
- Magnesium is stored in:
- Bone 40% to 60%.
- Within the cells, 30%.
- Muscles 20%.
- Serum 1% (RBC).
- The distribution of magnesium in the body is as follows:
- Skeleton =55%
- Soft tissue = 45%
- Extracellular fluid = 1%
- Total weight in grams = 25 G
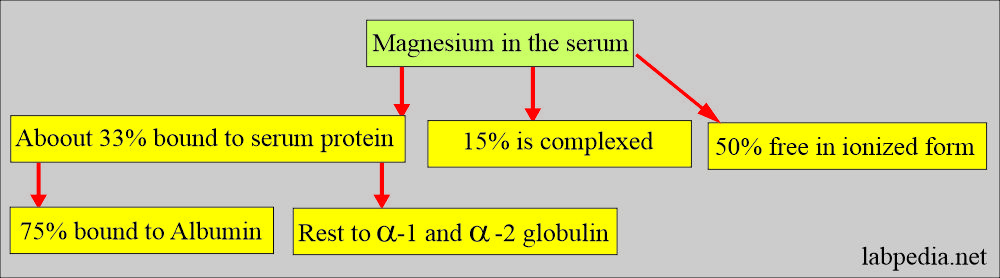
- Magnesium In the serum:
- 55% is free.
- 33% Associated with the protein (mainly albumin).
- 15% Complex with PO4, citrate, and other anions.
- Magnesium intracellular and extracellular are shown in the following diagram.
- Another source:
- 50% is present in the soft tissues, 50% in the bone, and about 1% to 5% is extracellular.
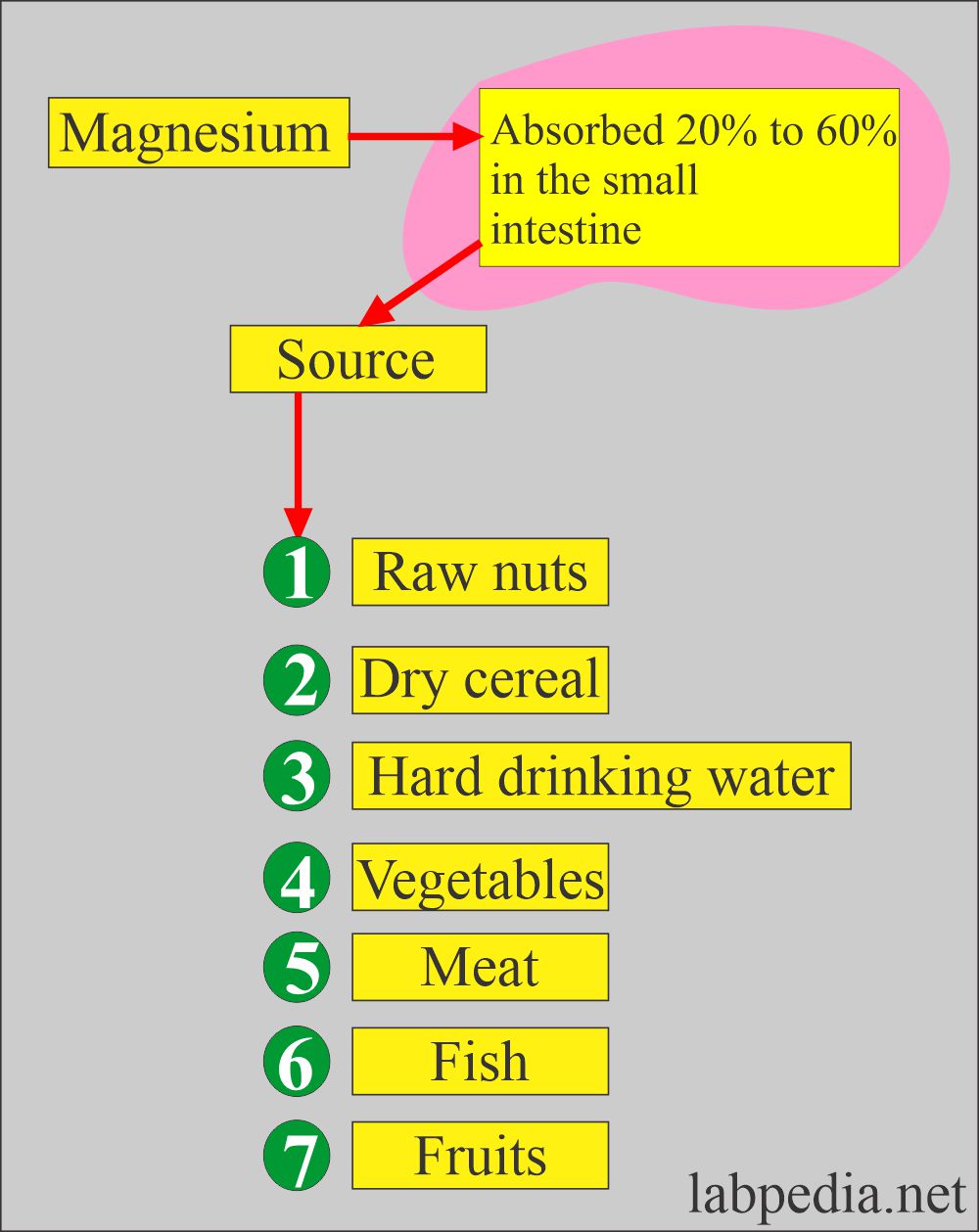
- Magnesium absorption and the source are:
- Meat.
- Green vegetables.
- It is absorbed in the upper intestine (small intestine).
- About 1/3 absorbed in the small intestine.
- 50% absorbed by the active transport or passive diffusion in the jejunum and ileum.
- Vitamin D is not needed for absorption.
- The majority of the Mg is not absorbed because of the formation of insoluble phosphates and soap in the gut.
- The average human being weighing 70 Kg will have 24 grams of magnesium.
- Excretion of the magnesium:
- Magnesium is excreted by the kidneys, primarily by glomerular filtration.
- Some tubular reabsorption also takes place.
- Parathyroid hormone (PTH) is an important regulator of the magnesium level in the blood. It occurs through the reabsorption of magnesium through the renal tubules.
- When the serum magnesium is low, it leads to increased neuromuscular excitability because magnesium competes and inhibits calcium entry into neurons.
What are the functions of Magnesium?
- Magnesium’s role in biosynthesis:
- Magnesium cofactor for >300 enzymes in the body.
- Magnesium is important for protein synthesis and enzyme activation.
- Magnesium is also important for oxidative phosphorylation.
- Magnesium’s Role in Neurons:
- Mg++ is important for neuromuscular excitability.
- It has an important role in smooth muscle contraction and relaxation.
- In cardiac patients, low magnesium levels increase the irritability of the cardiac muscles and may lead to arrhythmias.
- Mg++ had synergistic action along with sodium, calcium, and potassium ions.
- Magnesium absorption/Excretion:
- Magnesium helps with the absorption of calcium from the intestine.
- Magnesium deficiency mobilizes calcium from the bones.
- Magnesium deficiency may lead to abnormal calcification in the aorta and kidneys.
- It is important for the clotting mechanism.
- It has an important role in:
- Oxidative phosphorylation.
- Glycolysis.
- Cell replication.
- Protein Biosynthesis.
- Nucleotide metabolism (nucleic acid synthesis).
- Contraction of the muscular tissue.
- It is important for the action of ATP (adenosine triphosphate). It is bound to the ATP molecule.
- It takes part in phosphorylation, which is the main source of energy.
- The kidney:
- It is the organ that balances Mg.
- The kidney will conserve when the intake is low and excrete the excess when the intake is high.
- In a damaged kidney with decreased renal function, magnesium may be retained in the body and increase the serum magnesium level.
- Aldosterone promotes the excretion of the Mg++ together with K+ and the retention of Na+.
What are the causes of increased magnesium (Hypermagnesemia)?
- Antacids.
- Enemas.
- Parenteral therapy in patients with renal failure.
- Administration of Mg in a patient with renal failure.
- This raised serum magnesium leads to the following:
- Decreased neuromuscular transmission (depression of neuromuscular system).
- The decrease in cardiac conduction.
- Slow, deep tendon reflexes.
- There is respiratory depression.
- Magnesium-containing antacids may increase the magnesium level.
- Hemolyzed sample.
What are the signs and symptoms of increased magnesium (Hypermagnesemia)?
- Lethargy.
- Slurred speech.
- Nausea and vomiting.
- Muscles weakness.
- Deep tendon reflexes disappear at the level of between 5 to 9 mg/dL.
- Depressed respiration is seen at 10 to 12 mg/dL.
- Hypotension.
- Bradycardia.
- Cardiac arrest at a higher level.
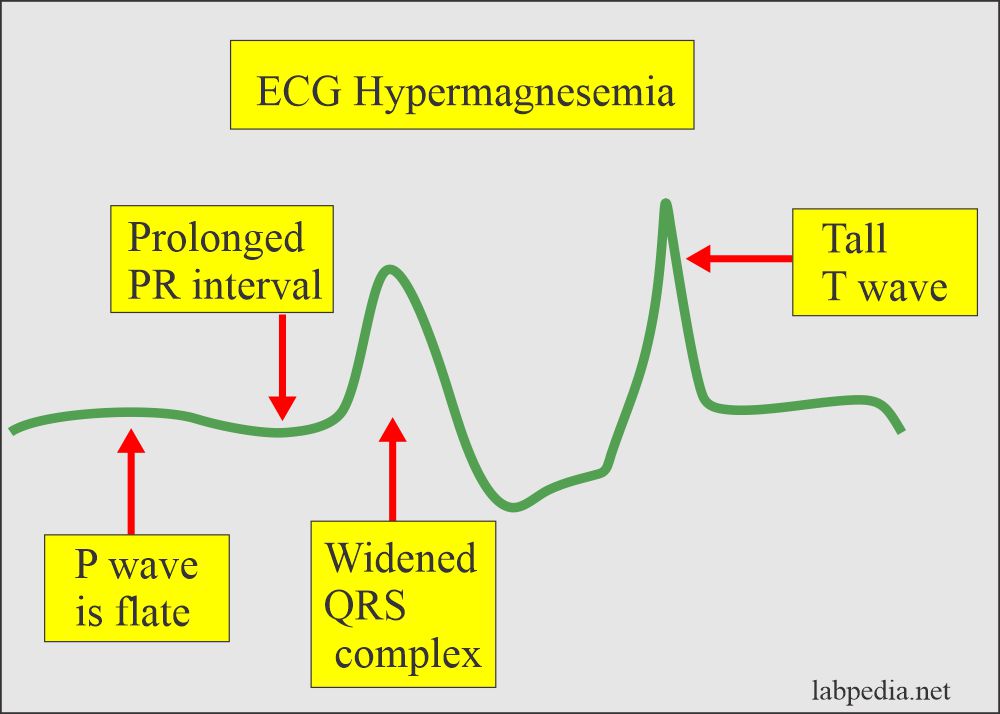
- ECG shows typical changes as follows:
- Tall T wave.
- Widened QRS.
- Flattened P wave.
- Increased PR interval.
What are the causes of low magnesium (Hypomagnesemia) and magnesium deficiency?
- Low magnesium is seen in:
- Hospitals.
- Intensive care units.
- Alcohol abuse increases the loss of magnesium in the urine.
- Malabsorption.
- I/V fluid therapy without magnesium.
- Hemodialysis.
- Diabetic ketoacidosis.
- Severe diarrhea.
- Hypercalcemia.
- Congestive heart failure.
- Some of the medicines, like thiazide diuretics, Cyclosporin, Cisplatin, and gentamicin.
What are the signs and symptoms of low magnesium (Mg++)?
- Low magnesium levels may lead to:
- Neuromuscular irritability with tetany and seizures.
- This is because Mg++ inhibits the entry of calcium into neurons.
- Cardiac arrhythmias may be seen. This may be related to hypokalemia and intracellular potassium depletion, secondary to magnesium deficiency.
- Tachycardia and hypotension.
- Increased reflexes.
- Muscle cramps.
- Nystagmus.
- Neuromuscular irritability with tetany and seizures.
- ECG changes are difficult to document in low Mg++, which is associated with other electrolyte imbalances, such as hypokalemia and hypocalcemia.
What are the normal values of Magnesium level (Mg)?
Source 1
| Age | mg/dL |
| Newborn | 1.5 to 2.2 |
| 5-month to 6 year | 1.7 to 2.3 |
| 6 to 12 year | 1.7 to 2.1 |
| 12 to 20 year | 1.7 to 2.2 |
| Adult | |
| 60 to 90 year | 1.6 to 2.4 |
| >90 year | 1.7 to 2.3 |
| Higher in females during menses | |
- To convert into SI unit = 0.4114 = mmol/L
Source 2
- Adults = 1.3 to 2.1 meq/L (1.8 to 2.6 mg/dL).
- Child = 1.4 to 1.7 meq/L (1.7 to 2.1 mg/dL).
- Newborn = 1.4 to 2.0 meq/L (1.5 to 2.2 mg/dL).
What causes increased magnesium (Mg++, hypermagnesemia) >2.5 meq/L?
- Oral intake of Mg++ in the presence of chronic renal failure.
- Renal failure and oliguria.
- Dehydration.
- Addison’s disease.
- Diabetes mellitus uncontrolled (rare).
- Antacids containing magnesium.
- Hypothyroidism.
- Multiple myelomas.
- The enema contains Mg++.
- Treatment of Mg++ deficiency.
What is the complication of Hypermagnesemia?
- It may cause respiratory paralysis and cardiac arrest.
What causes decreased Magnesium (Mg deficiency) <1.0 meq/L?
- Malabsorption (Kwashiorkor).
- Malnutrition (a diet low in protein intake).
- Prolonged nasogastric suction.
- Extensive bowel resection.
- Acute and chronic diarrhea.
- Intestinal and biliary fistula.
- Neonatal primary hypomagnesemia.
- Cirrhosis.
- Hypoparathyroidism.
- Hyperaldosteronism.
- Alcoholism, chronic.
- Chronic renal tubular disease.
- Chronic pyelonephritis.
- Interstitial nephritis.
- Glomerulonephritis.
- Renal tubular acidosis.
- Postrenal transplantation.
- Phosphate depletion.
- Hypercalcemia of any cause (Hyperparathyroidism).
- Hemodialysis.
- Chronic pancreatitis.
- Long Term I/V therapy,
- Diabetic acidosis.
- Idiopathic cause.
- Drugs:
- Diuretic therapy (furosemide).
- Cisplatin.
- Cyclosporin.
- Amphoterin B.
- Cardiac glycosides.
- Increased Excretion by the kidney:
- Tubular disorder.
- Pyelonephritis.
- Glomerulonephritis.
- Excess lactation.
- Pregnancy.
What are the complications of Hypomagnesemia (Mg++)?
- There are tetany, delirium, agitation, muscle weakness, and, ultimately, cardiac arrhythmias.
- There may be decreased Calcium, Phosphate, and Potassium levels.
What are the critical values of Magnesium?
- Hypomagnesemia = < 1.2 mg/dL (< 0.5 meq/L); there may be tetany.
- Hypermagnesemia = > 5 .0 mg/dL (> 3 meq/L).
Questions and answers:
Question 1: What is the level of hypomagnesemia?
Question 2: What is the raised critical level of magnesium?